Introduction
Cancers of the penis are relatively rare but present one of the biggest challenges in terms of proper diagnosis and treatment. The main reason for its late diagnosis lies in the late presentation of the patient to the clinician, and even if it takes place, the treatment is largely symptomatic at the beginning. Carcinomas are expected at later stages of the lesion development. This is thought to affect negatively the outcomes and procedures of resection can be extended to include the whole penis. The association of penile cancer with circumcision has been found to be very suggestive. For circumcised males, especially in childhood, have a very less chance of getting penile cancer than non circumcised males. This is perhaps the reason why penile cancers are more common in India, where circumcision practice is relatively less carried out.
The decision of carrying out penectomy is a very long and difficult decision to reach based on the person’s psychological response to the news as well as the present state of the condition. Although penectomy is also carried out in other conditions as well, this topic is mainly focused on cancer therapy and the role of penectomy in the achievement of goals.
Anatomy and physiology of the penis
The general organization of the penis consists of the following components. The glans penis, corpus spongiosum, the bulb of the penis, the paired corpora cavernosa which is comprised of skeletal muscles and tunica albugenia surround the smooth muscles (Hsu et al, 2004). The anatomy gives it an appearance of an independent organ. This organ is different due to the unique interplay of the skeletal, smooth muscles and the skeletal structures that form it. It is attached to the pubic ramus and ischium with the help of the periosteum, and is supported by the suspensory ligaments (Hsu et al, 2004).
The tunica albuginia is a biolayered structure that is composed of two layers of smooth muscles. The smooth muscles make up the sinusoids of the corpora cavernosa, corpus spongiosum and the glans penis. It is considered that penis is also among the 2 end artery organs of the body. It is these arteries that are assumed to play an important role in the erectile function (Hsu et al, 2004).
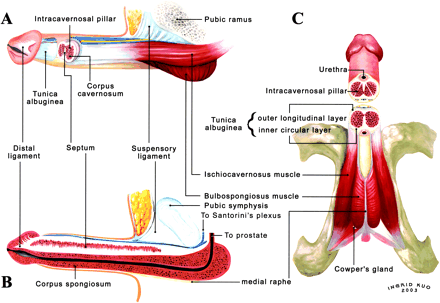
The paired corpora cavernosa and corpus spongiosum are the primary functional units of the penis. The penis receives both autonomic as well as somatic nerves. In an erection the corporeal body pressure is increased above the mean systolic blood pressure due to contraction of the perineal skeletal muscles. This increases the penile firmness. In the parasympathetic and the sympathetic fibers, it is acetylcholine that acts as the neurotransmitter. It is essentially the balance between the smooth muscle to the connective tissue that leads to the erectile response in a male. Both of these muscles lead to venoocculsion, helping in increasing the local pressure and thereby helping in reaching erection. The three stages in the penile function include the libido or the sexual desire, which is essentially a mental process, erection as a result of multiple external stimuli along with heightened response towards libido, the ejaculation in control of the sympathetic responses of the body, the organism which is under the influence of the sensations of sexual pleasure during coitus, and detumescence, which is the return to the flaccid state of the penis. All these phases follow in succession, and disturbances in any components, whether nervous or muscular can lead to defects in the penile function (Kendeel, Koussa and Swerdloff, 2001).
The development of the cancer, usually of squamous cell type, begins on the glans or the prepuce. This then expands and penetrates into the deeper corpora or the shaft of the penis. It has been reported that the flat lesions have more chances of early metastasis than the papillary type, and the nodal involvement. The femoral and the inguinal nodes are affected first. These are then followed by the superficial inguinal nodes. The complications of this cancer include sepsis and hemorrhage secondary to erosion of the femoral vessels and distant metastasis (Brosman, 2006).
Indications for surgery
Penile cancer has high mortality rates with recurrence rates that are also high if proper excision is not carried out. For this reason, initial treatments are better since reconstruction is fairly possible with good outcomes. However, the more the cancer has progressed, the more the chances of its recurrence and therefore removal of the penis or penectomy may become essential to increase the life expectancy of the individual.
Peroperative tests
The surgical procedure of penectomy is one of the major surgeries requiring good care before and after the procedure. Initial tests include blood reports, and ECG to check the working of the patient’s heart. Chest X rays and bowel preps are carried out. The area is prepared for surgery by shaving it (Surgery, A Guide for MTFs, Date unknown).
The more common diagnostic tests that are carried out in the cases of penile cancer include the ultrasound, the CT and the MRI scans. Echography has shown many false positive and false negative results, which has decreased its effectiveness in these particular cases. Ultrasounds are generally good for diagnosing enlarged or non palpable nodes for FNAC procedures. All of these procedures are however inadequate in identifying metastasis in the nodes that they detect. FNAC is in many ways superior to these methods, but relies on good sampling in cases of enlarged or non palpable nodes. Other methods of diagnostic and preoperative testing suggested include the gallium citrate scanning, sentinel node mapping (with some positive potential), medial inguinal lymph node biopsy and dynamic sentinel node mapping. These methods are already in use for diagnostic procedures however, the success rates are variable, and therefore search for newer methods of diagnosis in penile cancer are underway (Ananthakrishnan, 2006).
Mostly in the cases of penile cancer, the nodal metastasis is ascertained to understand the depth of penetration of the tumor. This is considered to be an important prognostic factor in the surgical success of the penis carcinomas. There are many problems in the diagnosing. The clinical examination is inadequate, prophylactic dissection can have high chances of morbidity and low chances of mortality. Of the minute diagnostic procedures, the dynamic sentinel node mapping has been found to be so far the better procedure among the others in diagnosing results. This test utilizes radio isotopes with or without intraoperative color dyes (Ananthakrishnan, 2006).
Usually before the procedure, an antibiotic course is carried out, which can later on be extended after the surgery to prevent any complications arising.
The surgical procedure of penectomy
It is the opinion of many surgeons that cases where there are high chances of nodal involvement and where the tumor status are T2, T3 and T4 and Grades 2 and 3 respectively are good candidates for prophylactic node dissections. The survival rates have been reported to be high when comparing to those patients who do not undergo this procedure. However, this procedure in itself can cause significant morbidity and even mortality. These can include wound breakdown and infection, and lymphoedema. Still, newer and modified approaches are considered adequate enough to prevent such incidences from happening (Ananthakrishnan, 2006).
The true surgical procedure can be a local dissection, a partial dissection or full dissection of the penis depending upon the case. In this case, surgeons recommend an aggressive approach to cancer in order to achieve long term palliation, increase survival rates and prevent recurrences. Small cancers less than 1.5 cm can be treated with local circumcision. However, those larger than these require partial or full amputation. Local wedge resection is also considered an option in some cases (Brosman, 2006).
The removal of small lesions requires the complete removal of the lesion with a good margin of normal tissue excised along with it. A two cm margin is the standard of normal tissue that is removed around the cancerous lesion. The use of section frozen is helpful in completely removing the lesion. At this time, if the surgical resection is large, then two more procedures can be carried out. These include urethral reconstruction and perineal urethrostomy (Brosman, 2006).
The Mohs Micrographic surgical procedure is considered a good treatment where local invasion is not present. This is a good procedure as it is able to preserve the normal tissues while resecting out tumorous one. Superficial lesions can also benefit from laser surgeries and therapies.
The removal of the primary tumor is followed by the removal of the inguinal lymph nodes should they be metastized as well. Retaining these lymph nodes increase the chances of pelvic lymph node metastasis, leading to further morbidity (Brosman, 2006).
Intraoperative hazards and complications in penectomy
Due to the high vascularity of the tissue, there are chances of infection, hemorrhage, profuse bleeding, dissemination of the tumor into the deeper lymph nodes etc. Most of the procedure’s complications are those that are seen in general surgical procedures, however, due to the complex neural and arterial supply, the procedure needs to be carried out with sound knowledge and good access to the surgical site.
Postoperative trends in penectomy
The first and foremost plan in the postoperative care of the penectomy patient is the pain management. The analgesic plan after penectomy can include many combinations. Either a continuous infusion of bupivacane is given at 0.25% along with fentanyl 2 micrograms at 5-15 ml/hour. Another intravenous infusion is morphine, given 1-10 mg/hour with bolus doses of 1 to 2 mg as per needed. PCA morphine is given as 1 mg bolus, with a 5 minute lockout. Diclofenic can be given at 50 mg/8 hours orally, or 100 mg/16 hrs rectally. Coproxamol, codydramol are given 2 tablets per 6 hours. Tramadol can be given 50-100 mg per 6 hours. And paracetamol can be given as 1g/ 6hours (Francesca, Echtle and Williams, 2007).
The initial and immediate post operative care is essential for the success of the treatment. Usually six to eight days are required for recovery, after which the patient is sent home and advised complete bedrest. Antibiotics, pain killers and anticoagulants are also given at this stage. (Surgery, A Guide for MTFs, date unknown)
Patients are later on advised to come for repeated checkups and followups so as to ascertain the success of the procedure and identifying any complications beforehand. These followups can then be reduced in frequency upon successful conclusion of the matter.
Nursing care plan for such patients
Pain in the cases of penile cancer can occur at any stage of the condition. Pain is early stages are attributed to subvesical obstruction leading to voiding dysfunction. In the later stages of cancer the cause of pain is inguinal in nature and is mainly due to metastasis and lymph node enlargement. This tumor mass can exert pressure on the surrounding organs, which can be another cause of pain. Lymphoedema is another reason why pain can occur in such patients (Francesca et al, 2007).
Since the care of the patient goes according to the treatment plan, in such patients the first phase of pain management is the removal of cause i.e. the removal of the tumor. Surgery, chemotherapy and the radiotherapy mark this phase of treatment. The second phase is after the surgical procedure and includes which uses pain killers for the relief of pain along with any other medicines that may be deemed necessary (Francesca et al, 2007).
Drug therapies for pain relief in penile cancer patients include NSAIDS including the COX 2 selective inhibitors as the most preferred drug among the clinicians. Other pain drugs that can be given include paracetamol and its combinations with codeine and dihydrocodiene, opioids in various administration forms and various epidurals (Francesca et al, 2007).
Debridment of the wound and prevention of wound infection is a main area of focus for the nursing team, primarily as the rates of infection in such cases are high. Patients are in considerable psychological distress due to such procedures, and therefore may warrant more attention and care than most to help them in the transition to the new state. Nurses can help by providing them with a good and friendly environment, providing rapid pain relief and giving them support during their stay in the hospital.
Conclusions
Penectomy procedures are very complex procedures and are considered one of the major surgeries to be carried out. This procedure requires good nursing care before, during and after the cancer treatment to achieve positive results. Although a relatively rare procedure, it is still the cause of significant morbidity and mortality in the patients and therefore must be carried out with due care and attention.
References
N Ananthakrishnan, 2006. Diagnosing Metastatic Disease in Inguinal Nodes in Penile Cancer: Do We Have a Test and the Evidence. Indian Journal of Urology, Vol. 22, Issue 4, pp. 345-350
F. Francesca,P. Bader, D. Echtle, F. Guinta and J. Williams, 2007. Pain Mangagement. European Association of Urology, 2007.
Stanley A Brosman, 2006. Penile Cancer. Web.
Geng-Long Hsu, Cheng-Hsing Hsieh, Hsien-Sheng Wen, Wen-Long Hsu, Chih-Hsiung Wu, Tsorang-Harn Fong, Shyh-Chyan Chen and Guo-Fang Tseng, 2004. Anatomy of the Human Penis: The Relationship of the Architecture Between Skeletal and Smooth Muscles. Journal of ANdrology, Vol 25, No. 3.
Fouad R. Kandeel, Vivien K. T. Koussa and Ronald S. Swerdloff, 2001. Male Sexual Function and Its Disorders: Physiology, Pathophysiology, Clinical Investigation, and Treatment Endocrine Reviews 22 (3): 342-388
Surgery: A Guide for MTFs. Web.