Subject
Supervised Injection Services (SIS) in Interior BC as the means of managing the problem of substance dependence.
Context
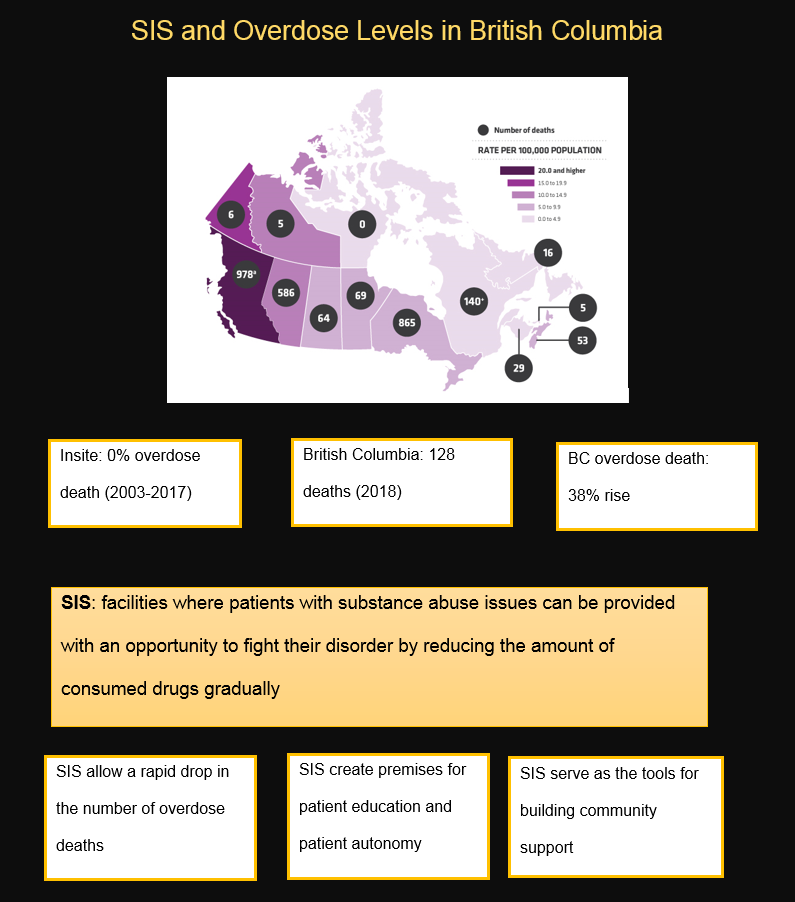
The problem of use disorder has been quite topical for British Columbia (BC), Canada. Supervised Injection Services (SIS) have been established in other areas of Canada, such as Vancouver, yet Interior BC remains without the specified type of support for people with substance dependency issues (Government of Interior BC, 2018). The levels of successful chemical dependency management are currently much higher in Vancouver than in Interior BC (BC Center for Disease Control, 2018).
According to the recent statistics, there have been 213 cases of illegal use disorder overdose cases compared to 83 in Vancouver Coastal and 34 in the Interior (BC Center for Disease Control, 2018). Furthermore, statistics show that in 85% of the lethal cases, no emergency call was made (BC Harm Reduction Services, 2018). According to the recent crime statistics, 73% of the substance-related offenses in Interior BC are associated with drug possession (“Cannabis crime statistics in Canada,” 2016). Historically, Interior BC is not predisposed to criminal activity related to illegal drugs.
The case under analysis represents Liam Brown, an indigenous Canadian living in rural British Columbia, with a history of substance dependence. Liam has also had several adverse childhood experiences (ACES) and has strong dyslexia. The client was abused by his father, who used physical and emotional intimidation on his child. Although Liam’s mother divorced Liam’s father after the abuse had been discovered, Liam was not provided with the required therapy.
The specified experiences can be considered as a serious psychological trauma that could have affected his further development and may have led to the current problem of chemical dependency. The problems are aggravated by COPD, the lack of education, absence of family support, unpaid rent, and job loss. The health care practitioner will work with Liam to identify past coping skills, recognize the effect of his present choices on his health and well-being, and begin forming a plan for care.
Financial constraints, the lack of patient education, and service inaccessibility define the problem in the specified region and, particularly, in the case in question (BC Center for Disease Control, 2017; Centre for Addiction and Mental Health, n.d.). The patient’s current category can be defined as severe since he lacks control over his problem almost entirely. Therefore, assistance in the form of supervised injections and therapy, as well as detailed consultations, should be provided.
Furthermore, the historical issues such as the refusal to view use disorder as a mental health issue and, thus the absence of social support or SIS-related services for the specified demographic should be regarded as a factor for the development of use disorder (Potier, Laprévote, Dubois-Arber, Cottencin, & Rolland, 2014; Potier et al., 2014).
The historical context also defines the attitudes toward drug addiction in the specified area, representing it as a social stigma that alienates a patient from a community immediately (BC Center for Disease Control, 2017; Potier et al., 2014). Furthermore, the false assumption that illegal use disorder immediately leads to HIV/AIDS is a popular myth that affects the lives of people such as Liam (BC Center for Disease Control, 2017).
Finally, factors associated with access to healthcare services and particularly SIS, play an important role in defining their chances for recovery. Liam lives in a rural setting, which is quite far from the nearest SIS, such as Kelowna or Kamloops (approximately 4 hours of driving). With the opening hours of the specified SIS between 9 a.m. and 5 p.m., patients who live in rural areas like Liam cannot access the proposed SIS services. Building a larger number of SIS that is located in the vicinity of the target population should be seen as an adequate response to the specified problem (Harris & Rhodes, 2013).
Priorities in Relation to Health Promotion or Prevention
There is a strong need for establishing SIS-related services in interior Interior BC, Canada. Because of high rates of drug overdoses, it is critical to take the necessary measures to assist the patient in fighting his dependency and preventing relapse and OD (“Health Canada approves supervised injection sites for Kelowna and Kamloops,” 2017). At present, several immediate, short-, and long-term priorities can be identified.
In terms of immediate steps that should be taken, one has to name the need to prevent the instance of drug overdose (OD) caused by the lack of education in the patient (“9 deaths in 5 days: more overdoses reported in B.C. Interior,” 2018). Therefore, it is critical for an APRN to create an outreach program for the patient to provide patients with the crucial info formation about use disorder. The program will be housed at a local nursing facility, where patients will be provided with consultations and the necessary education.
Short-term objectives include improving the working hours of the available SIS in Kelowna and Kamloops, promoting education among patients and nurses, and using a multidisciplinary approach toward managing the problem by enhancing cooperation between nurses and physicians. The latter step will require introducing uniform instructions for managing the needs of patients with use disorder issues. Finally, long-term goals incorporate the enhancement of SIS’s services and its further use for improving health outcomes within the community, at the same time, increasing the levels of patient awareness and education among the vulnerable population members.
In order to adders the social determinants of health listed above, one should incorporate a theoretical framework that would encourage the implementation of the proposed change. Specifically, one should focus on using the psychosocial theory (Fiorati, Arcêncio, & Souza, 2016).
The identified framework will help nurses understand the choices that patients make due to the social and economic factors that affect their lives. Particularly, the psychosocial theory, such as Eriksson’s theory of development, will allow addressing the traumatic events that occurred to the patient in his childhood (Fiorati et al., 2016).
Health Promotion Interventions, Strategies or Approaches
As stressed above, when considering the available intervention strategies, one should consider the enhancement of patient-nurse communication as the platform for use disorder management. Thus, at present, the short-term strategy should include recognizing the problem of use disorder in Interior BC and establishing the objectives for improving the quality of care by shaping the current SIS schedule before SIS facilities are built in rural areas.
The suggested step will set the premise for building a program for use disorder management. In the long-term prospects, the SIS will be integrated into the existing healthcare framework as a community center, where people with use disorder problems will be provided with the required support. However, given the current short-term objectives, it is critical to establish a virtual version of SIS that will imply providing patients with the support and consultations needed to sustain their health.
The long-term strategy as it pertains to the problem of SIS introduction into the Interior BC setting implies rearranging the current infrastructure of SIS. Moreover, a change in their schedule, including the facilities that will be built in the future, will have to be improved so that patients from remote areas could access them faster. For instance, the current approach for scheduling used by Interior Health does not leave any opportunities for people traveling from Interior BC to the Interior facility to receive the required support.
Specifically, the range of 12 p.m. – 3.30 p.m. from Tuesday to Friday does not leave any room for patients to adjust to the tight schedule, given the complex infrastructure of the transportation services. Therefore, short-term access to care must be improved (Interior Health, n.d.).
Finally, a long-term strategy concerning the establishment of SIS in the Interior BC setting will have to be established in order to advance the current situation. The fact that a lot of Canadians with drug dependency issues die without SIS in the vicinity indicates that there is an urgent need to build one in the Interior BC environment (Interior Health, n.d.). Since setting an SIS center in the Interior BC context is likely to take a significant amount of time, it is reasonable to start with introducing mobile tools as the immediate assistance to the people that require treatment against drug addiction.
The use of applications that will allow contacting SIS staff members immediately will lead to the successful management of urgent health-related issues. However, it should be noted that building a physical SIS will require a substantial amount of time. Therefore, to address the needs of the target population, one will have to create a virtual environment where nurses will be able to provide patients with consultation and care. Telehealth should be incorporated into the set of the available techniques (Canadian Agency for Drugs and Technologies in Health, n.d.).
Moreover, the long-term objective of handling the problem of social prejudices has to be mentioned as one of the major problems that need to be addressed. The specified issue can be handled with the help of a patient education program that can be performed along with the introduction of SIS services into the context of the Interior BC setting. The specified change will allow reducing the levels of alienation between the patient and his family, as well as his community, in general.
By providing knowledge and education to community members, SIS works will create the setting in which patients will not feel ashamed to use SIS services. Moreover, the support of family members and the community will create the platform for a faster recovery among the vulnerable group, with a significantly lower chance of relapse (Best et al., 2016). Thus, the specified strategy will help to meet the objective of encouraging the community and family support for patients with use disorder issues, as well as reduce the harmful effects of social prejudices.
Implementing Health Promotion Strategies and Engaging with Patients/Families in Clinical Practice
One should consider applying the strategies aimed at harm reduction as a short-term goal. Specifically, one will have to recognize the fact that supervised injection is needed due to the threat of relapse and OD. In the process, the program, such as Insite, should be viewed as an example (Ng, Sutherland, & Kolber, 2017). The SIS program in question will have to be based on the same idea of patient independence and family support and incorporate these long-term considerations into its framework.
Specifically, SIS created in the Interior BC setting will have to follow the example set by Insite and similar facilities in Vancouver (Canadian Center on Substance Use and Addiction, n.d.). For instance, Insite will provide the example of involving patients’ families and community members as the support for further intervention and treatment (see Fig. 1).
Another important long-term goal that needs to be included in the body of the SIS program that will be implemented in the Interior BC setting is the infrastructure issue. Because of the physical unavailability of the services, patients may face significant difficulties accessing the SIS facility.
Thus, mobile applications for consulting SIS experts will have to be provided for the patients that are either hesitant about using the service or face difficulties reaching it physically for specific reasons. The mobile services will have to include an application for contacting an expert immediately and asking for online support such as the delivery of the relevant information or online consultations.
In order to make the specified issues relevant to the patient represented in the case study, one will need to introduce the foundation for family-oriented therapy. Particularly, the fact that the patient is currently completely detached from the closest people in his life shows that the further efforts made at SIS will have to be geared toward assisting the patient in building a rapport with his family members.
In addition, the overall level of prejudices in the community seems to affect the patient’s condition significantly, which means that the healthcare experts working at SIS should also integrate a strategy aimed at increasing the levels of awareness within the community. Finally, the fact that the patient needs to develop tighter control over his cravings in regard to drugs indicates that the therapy process should start with a very slow and gradual reduction in the number of drugs administered to the patient regularly. The patient’s financial insecurities will also need to be handled, respectively, with SIS providing the patient with free services to assist him in paying his rent and becoming financially secure.
The focus on patient education and the increase in the level of nurse competencies should also be seen as a necessary step. By building patients’ agency and independence, a nurse will help them acquire the necessary knowledge and skills for preventing relapse and avoiding instances of recidivism. Similarly, educating patients’ family members should be regarded as essential since the target population will require emotional and psychological support.
Counseling should be used as the means of helping families of people with use disorder issues to acquire the necessary information. Nurse education, in turn, will require interdisciplinary cooperation as the pathway to improving the quality of care (McKenna, Pajnkihar, & Murphy, 2014).
The integration of a shared decision-making model into the policy should also be deemed as critical. The inclusion of the specified approach will help build confidence in patients, thus encouraging them to acquire the proposed behaviors and fighting their dependency issues successfully. With the introduction of the proposed tool and the enhancement of patient education, one will be able to create premises for patient independence and responsibility regarding the management of use disorder. The use of shared decision-making will allow patients to become more confident in handling their disorder. Furthermore, the specified step will lead to patient education.
Conclusions and Relevancy
The introduction of SIS into the environment of Interior BC and especially its remote areas, including rural ones, may assist in targeting people of different cultural and ethnic backgrounds. Because of the difficulties that the specified demographic may have in adjusting to the Interior BC setting, as well as the problems associated with communication, people from different ethnic and cultural backgrounds will require the active support of SIS and the community in order to fight mental health issues and especially the problem of substance overuse.
The information learned in the course of the case analysis is bound to serve as the basis for me to deliver better performance in the clinical setting and assist patients more effectively. Particularly, it will be necessary to use counseling as the means of involving family members, build the framework for patient education by increasing their awareness and encouraging education and multidisciplinary cooperation among nurses.
The adoption of the framework described above will contribute to building a rapport with vulnerable groups and empowering them to make a positive shift in their health status. By using the examples of other organizations such as Insite, I will create the environment in which patients will feel comfortable and where they will no longer experience the social and economic constraints that prevent them from seeking help in their regular setting.
References
BC Center for Disease Control. (2017). Overdose response reports. Web.
BC Center for Disease Control. (2018). Illegal drug overdose events. Web.
BC Harm Reduction Services. (2018). By the numbers: The opioid overdose emergency in BC. Web.
Best, D., Beckwith, M., Haslam, C., Alexander Haslam, S., Jetten, J., Mawson, E., & Lubman, D. I. (2016). Overcoming alcohol and other drug addiction as a process of social identity transition: The social identity model of recovery (SIMOR). Addiction Research & Theory, 24(2), 111-123.
Canadian Agency for Drugs and Technologies in Health. (n.d.). Telehealth: Summary of evidence. Web.
Canadian Center on Substance Use and Addiction. (n.d.). Supervised injection facilities (SIFs): FAQs. Web.
Cannabis crime statistics in Canada. (2016). Web.
Centre for Addiction and Mental Health. (n.d.). Addiction. Web.
Government of BC. Illicit drug overdose deaths in BC. January 1, 2008 – September 30, 2018. Web.
Harris, M., & Rhodes, T. (2013). Hepatitis C treatment access and uptake for people who inject drugs: A review mapping the role of social factors. Harm Reduction Journal, 10(1), 7-17. Web.
Health Canada approves supervised injection sites for Kelowna and Kamloops (2017). CBC. Web.
Interior Health. (n.d.). Mobile supervised consumption services. Web.
McKenna, H., Pajnkihar, M., & Murphy, F. (2014). Fundamentals of nursing models, theories and practice (2nd ed.). New York, NY: John Wiley & Sons.
Ng, J., Sutherland, C., & Kolber, M. R. (2017). Does evidence support supervised injection sites? Canadian Family Physician, 63(11), 866-866.
9 deaths in 5 days: More overdoses reported in B.C. Interior. (2018). Web.
Potier, C., Laprévote, V., Dubois-Arber, F., Cottencin, O., & Rolland, B. (2014). Supervised injection services: What has been demonstrated? A systematic literature review. Drug and Alcohol Dependence, 145, 48-68. Web.