Summary
This project aims at identifying the relationship between the use of antibiotics and farming and people’s health issues related to antibiotic resistance. People consuming organic (antibiotic-free) and mass-market (produced by big farming organisations) will complete monthly reports for a year. The reports will include information concerning the consumed food, purchases (meat and dairy products), health issues, antibiotics use.
Funding Body

Medical Research Foundation can be interested in funding this project due to its possible implications. The organisation has announced its intent to fund research addressing several areas, including “the influence of human behaviour within and beyond healthcare settings” (Medical Research Foundation 2018, para. 5). The present study lies within the scope of this topic as it aims at exploring the peculiarities of the behaviour of people who have been diagnosed with an antimicrobial-resistant bacteria infection.
Background
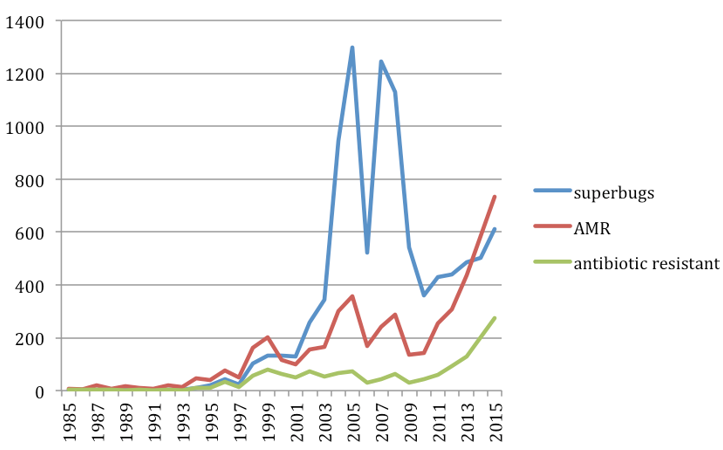
It has been estimated that approximately 25,000 people in the EU die due to antibiotic resistance (Sandoiu, 2018). It is also predicted that antibiotic resistance can account for 10 million deaths in 2050 if the current trends do not change. One of the primary reasons for this condition in people is the use of antibiotics in farming (Lee Ventola 2015). Farmers worldwide have used this type of medication to prevent the spread of illnesses in their animals, prevent the development of diseases, and even accelerate animals’ growth (Economou & Gousia 2015). However, the use of antibiotics is associated with the occurrence of antibiotic resistance in people (Watkins & Bonomo, 2016). The need for a thorough investigation into the matter is apparent.
Aims and Hypothesis
The aim of this project is to identify the relationship between people’s development of an antimicrobial-resistant bacteria infection and their behaviour with the focus on their dietary habits, as well as their exposure to animals and/or antibiotics.
The following hypothesis will guide the present study:
- People consuming mass-market products (not labelled as organic or antibiotic-free) are more likely to be infected with antimicrobial-resistant bacteria as compared to people consuming products labelled as “no antibiotics.”
The null hypothesis can be formulated as follows:
- People consuming mass-market food and those eating antibiotic-free foods have equal chances of being infected with antimicrobial-resistant bacteria.
Methodology and Programme of Work
The project will last for one year and will involve people from different parts of the UK. The potential participants will be recruited in supermarkets and retail units specialising in selling organic and/or antibiotic-free meat and dairy products. Those who agree to participate will complete monthly reports concerning their diets, purchases (only meat and dairy products will be included), and health issues (antimicrobial-resistant infection) they might have, as well as antibiotics they use, exposure to certain hazards (such as working on a farm).
The overall number of participants will be approximately 10,000 (including 5,000 consumers of organic foods and 5,000 people consuming products of big farming organisations). People over 18 years old will be included in order to avoid certain ethical issues, while other variables such as gender, ethnicity, or socioeconomic status will be excluded. Simultaneously, quarterly laboratory tests of the products bought in some of the retail units will be conducted.
Budget
The preliminary budget for the project is as follows:
Ethical Issues
This research is not associated with any considerable ethical issues as all precautions will be taken. The participants will be informed about the goals, methodology, and implications of the study. They will be informed about their rights. No vulnerable populations will be included, and the participants will sign written consent forms. Data confidentiality and anonymity will be ensured with the help of standard procedures.
Impact
The major impact of this study is its wide-scale outreach due to the sample size. The relationship between the use of antibiotics in farming and people’s behaviour will be identified or rebutted. The research may become a starting point for a larger project as the methodology can be used in other countries.
Reference List
Economou, V & Gousia, P 2015, ‘Agriculture and food animals as a source of antimicrobial-resistant bacteria’, Infection and Drug Resistance, vol. 8, p. 49-61.
Lee Ventola, C 2016, ‘The antibiotic resistance crisis: part 1: causes and threats’, Pharmacy & Therapeutics, vol. 40, no. 4, pp. 277-283.
Medical Research Foundation 2018, Funding the future of antibiotics research. Web.
Sandoiu, A 2018, ‘Drug resistance: does antibiotic use in animals affect human health?’, Medical News Today. Web.
Watkins, RR & Bonomo, RA 2016, ‘Overview: global and local impact of antibiotic resistance’, Infectious Disease Clinics of North America, vol. 30, no. 2, pp. 313-322.