Methicillin-resistant Staphylococcus aureus is a Staphylococcal bacterium that is impervious to a collection of antibiotics referred to as beta-lactams. Beta-lactams include antibiotics such as methicillin, amoxillin, penicillin, and oxacillin (“CDC – Methicillin-resistant Staphylococcus aureus (MRSA) Infections”).
Methicillin-resistant Staphylococcus aureus are also unaffected by cephalosporins (Chang 4). Several factors contribute to antibiotic resistance in bacteria. These factors include mutations, overuse, and misuse of antibiotics (Chang 9). A good number of MRSA diseases are skin illnesses. Relentless or potentially grave MRSA illnesses happen more often to immunocompromised patients in healthcare surroundings.
However, recent occurrences indicate more people who live away from hospitals get MRSA. This strain is the “community-associated MRSA (CA-MRSA) or superbug strain” (Todar 2). The Centers for Disease Control and Prevention (CDC) cite that of the 25% to 30% of people colonized by staphylococcus bacteria, only 2% has MRSA. Colonization occurs when an individual has the bacteria, but reveals no indicators of the disease.
Chang attributes colonization to the existing equilibrium between the presence of bacteria and the body’s capability to battle the infection (2). Besides, Staphylococcus coexists with other types of bacteria on the skin, which do not allow it to dominate fully. An individual’s strong immunity also forestalls Staph infections in colonized people.
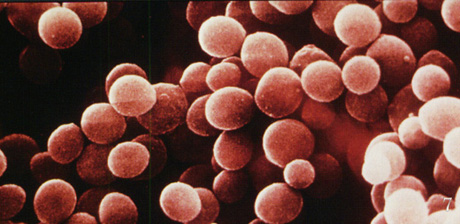
Staphylococci are sphere-shaped bacteria that come about in tiny groups similar to grapes. They are Gram-positive bacteria commonly found on noses of healthy humans (as normal flora). Other body areas such as the mouth, skin, and the digestive system also harbor Staphylococcus aureus (Todar 1).
The genus Staphylococcus belongs to family Staphylococcaceae. Staphylococcus aureus grows into a big yellow colony on enriched culture medium and is hemolytic on blood agar (1). According to Todar, the Staph bacteria display optimum growth in a variety of conditions such as sodium chloride strengths of 15% and warmth of 15oC to 45oC (1).
Staphylococci form flawlessly round cells with a thickness of one micrometer. They grow in bunches because the cells split in succession, in three perpendicular levels with the progeny staying connected to each other after every division (Todar 1).
This forms an overall appearance of an uneven assembly of cells. Staphylococcus aureus are non motile and do not develop spores (1). These bacteria produce numerous potentially hostile factors that help them during colonization of the host. Examples of these factors are surface proteins, invasions, surface factors, and exotoxins. In addition, MRSA have biochemical qualities such as immunological covers that help them continue to exist in phagocytes.
Early detection of symptoms is essential for cure and proper management of any infection. Therefore, it is crucial to identify the symptoms associated with Staphylococcal infections. Common MRSA illnesses in the community are skin diseases whose main symptoms are abscesses. These abscesses are often red, sore, enlarged and contain secretions such as pus.
The blisters often mimic the appearance of spider bites and commonly ensue at locations of noticeable skin damage (for example grazes and scratches), and sections of the body concealed by body hair such as the armpits, groin, nape, and the chin in men. MRSA in hospital situations frequently triggers dangerous infections, for example, bloodstream diseases, pneumonia, and surgical spot illnesses.
In such situations, the symptoms often differ by the kind and phase of the infection (“CDC – Methicillin-resistant Staphylococcus aureus (MRSA) Infections”). Acute MRSA may also cause conditions such as Toxic Shock Syndrome, bacteremia, and necrotizing fasciitis (Chang 2).

Most people naturally have Staphylococcus bacteria on their bodies. Therefore, body contact (skin to skin) is the main mode of spreading Staph. Athletic gear, razor blades, tattoo tools, bed sheets, and towels also pass on Staphylococcal infections. Sports activities involving close body contact (for example boxing, wrestling, and soccer) play a significant role in communicating these illnesses (Chang 9). Latest studies indicate that domestic pets for instance dogs and cats spread MRSA infections, as well.
Cure for MRSA involves wound therapy and elimination of the bacteria. Treating skin wounds requires nipping, draining, and application of antiseptics to the wounds. Elimination of the bacteria is a challenging task considering MRSA resistance to most antibiotics. However, several other antibiotics still have effects on MRSA. These include drugs such as “vancomycin, linezolid, daptomycin, tigecyclin, and quinupristin-dalphopristin” (Chang 4).
Patients must always take the antibiotics according to the prescription, and go back to the doctor if the illness refuses to go away a few days after the initiation of treatment. CDC advises healthcare givers to culture the microorganisms and do susceptibility testing. This procedure guides treatment especially in serious infections that may be unsuccessful in responding to early medication.
MRSA preclusion efforts differ according to an individual’s surroundings. However, the most effective preventive measures entail high levels of personal hygiene. People ought to keep their hands methodically clean by washing them with soap and clean water, or using alcohol-containing hand wash liquids. Chang cites that hand washing with soap must involve energetic rubbing for about 20 seconds, rinsing, and thorough drying using a disposable wipe (8).
When using alcohol-based sanitizers, sufficient amount of the solution should be rubbed meticulously on the hands paying consideration to the fingers and thumbs. The product is left to dry naturally on the hands. Chang insists that allowing the sanitizer to dry naturally gives it time to destroy germs on the hands (8). Infected people ought to ensure that they observe this routine each time they handle their wounds, which must be covered appropriately until they heal. Healthy people are supposed to avoid touching infected wounds and used dressings.
Maintaining a healthy environment by ensuring that all surfaces are clean also helps in preventing MRSA. Patients ought to continue taking the prescribed doses of antibiotics to ensure complete elimination of pathogens in the body. In healthcare settings, the CDC gives charts with relevant information on precautions to prevent infection.
These measures are similar to those in personal prevention. However, they include extra safety measures such as ensuring that infected patients are occupying their own rooms and restricting them from visiting common regions of the hospital. The CDC encourages healthcare givers to wear gloves and gowns on top of their regular clothes while attending to patients with MRSA.
Doctors and nurses are at liberty of carrying out random MRSA tests on patients by wiping a cotton swab on the patients’ nose or skin. MRSA prevention in hospitals also requires that the entire hospital undergoes disinfection once in a while. However, hospital paraphernalia can be sanitized regularly (“CDC – Methicillin-resistant Staphylococcus aureus (MRSA) Infections”).
The traits of MRSA as revealed by this paper indicate that MRSA is here to stay since Staphylococcus bacteria are part of the body’s normal flora. It is, therefore, up to humans to learn to coexist with Staphylococci by maintaining high standards of hygiene to prevent illnesses attributable to MRSA.
Works Cited
CDC – Methicillin-Resistant Staphylococcus aureus (MRSA) Infections. n.d. Web.
Chang, R. Hernan. MRSA and Staphylococcal Infections. United States of America: Lulu.com, 2006. Print.
Todar, Kenneth. “Staphylococcus aureus and Streptococcal Disease.” Todar’s Online Textbook of Bacteriology. 2012. Web.