Introduction
Depression is one of the most common mental disorders that occur in different populations. It is characterized by a long-term clinical condition of the patient, which does not improve without medication and therapy. Moreover, certain populations, like children, adolescents, and older adults, are more vulnerable to various mental disorders due to their emotional susceptibility (Selph & McDonagh, 2019). This assignment will analyze the nuances and features of depression treatment in children.
Causes and Symptoms of Depression
The causes of depression in children can be biological, psychological, and environmental. Selph and McDonagh (2019) note that among the biological causes of depression in children may be hereditary depression in parents, being overweight, chronic diseases, and hormonal changes during puberty. In addition, depression in children can develop under the influence of external circumstances, such as relationships with parents and peers, academic problems, or disasters. Among the psychological factors influencing the development of depression in children, Selph and McDonagh (2019) distinguish violation of emotional regulation, low self-esteem, negative thinking, and previously diagnosed depressive disorder. Therefore, the main reasons are related precisely to the violation of social ties with parents or exclusion from the company of peers.
The main symptoms of depression in a child may include sleep disturbances, weight gain or loss, difficulty concentrating, loss of interest in activities that used to bring pleasure, increased irritability, and prolonged sadness. At the same time, it is necessary to distinguish between lousy mood and symptoms of depression. The task of parents or guardians is to talk with the child about his experiences and feelings. Depression is characterized by “a persistent depressed mood with the inability to anticipate future enjoyable events” (Selph & McDonagh, 2019, p. 610).
Moreover, children under eight may have problems verbalizing feelings (Mullen, 2018). Therefore, it is necessary to pay attention to changes in the child’s behavior, such as persistent somatic complaints, excessive crying and screaming, and prolonged anhedonia. In addition, Mullen (2018) notes that children of any age with a depressive disorder are characterized by “thoughts of worthlessness or suicide” (p. 277). Hence, when detecting the slightest changes in the child’s behavior, which may be signs of depression, it is necessary to seek medical help from professionals.
Diagnosing Depression in Children
The main reason for the vulnerability of children to depression is incompletely formed emotional intelligence and the ability to control reactions to various situations. Children are more receptive to negative comments and often take everything personally, regardless of other circumstances. The initial assessment of the child’s mental state takes place by talking with the parents and the patient to identify the main complaints and symptoms.
Moreover, it is possible to use laboratory tests of patients’ blood to diagnose depression. For example, Zhou et al. (2018) experimented with detecting depression in children through biomarkers in their blood. One of the biomarkers is adenosine and inosine, a reduced level of which indicates a greater vulnerability of the child to depression.
In addition, one of the symptoms of depression is metabolic disorders, which lead to sudden weight loss or weight gain. Therefore, Zhou et al. (2018) found that the level of uric acid, which is “a major circulating antioxidant,” affects the child’s resistance to stress and depression. Therefore, plasma biomarkers may be an effective method for diagnosing depression in children.
Medication Treatment Options
For mild forms of depressive disorder, first of all, it is necessary to use psychotherapy and group therapy for the child. However, drug treatment with antidepressants is the primary option “for moderate-to-severe depression or depression that has not responded to an adequate trial of psychotherapy” (Mullen, 2018, p. 277). The use of medications should be supported by therapy for the best effect in treating depression.
The age of patients imposes certain restrictions on the choice of medicines and their allowable dosages. Zhou et al. (2020) found that “nefazodone and fluoxetine were associated with fewer dropouts than sertraline, imipramine, and desipramine” (p. 596). Patients reported fewer side effects from nefazodone and fluoxetine than from other drugs. In addition, Zou et al. (2020) conducted a study using a placebo pill in combination with psychotherapy. This treatment option was quite effective for patients, but its effectiveness is difficult to predict.
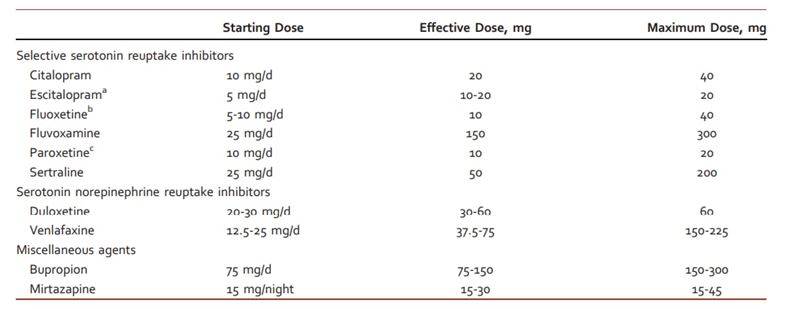
Despite the fact that children are just as susceptible to depression as adults, drug treatment for them is very different. Fluoxetine is the only FDA-approved antidepressant for children (U.S. Food & Drug Administration, 2019). Moreover, abnormal use of antidepressants can aggravate the main symptoms of depression, so it is necessary to adhere to precise dosages. Mullen (2018) states that for the results of drug treatment to be more predictable, it is necessary to start treatment with the minimum effective dose (Figure 1). Taking other medicines is possible only in severe conditions of the patient and under the constant supervision of a doctor.
Medication Considerations
Option 1:
- Fluoxetine (Prozac) 10 mg
- 1 tab, PO, qDay
- Dispensed amount 30
- Zero refills.
Option 2:
- Duloxetine (Cymbalta) 30 mg
- 1 tab, PO, qDay
- Dispensed amount 14
- Zero refills.
Option 3:
- Sertraline (Zoloft) 25 mg
- 1 tab, PO, qDay
- Dispensed amount 14
- Zero refills.
Monitoring
Despite the general recommendations for taking medications, regular monitoring of the patient’s condition, including laboratory tests, is necessary. Laboratory tests of the patient’s blood can help identify evidence of antidepressant abuse, which can lead to addiction. Moreover, monitoring helps to identify comorbid medical issues like “hypothyroidism, anemia, autoimmune disease, and vitamin deficiency” (Selph & McDonagh, 2019, p. 610). Depression in children can often be accompanied by other conditions, such as eating disorders and anxiety.
Special Considerations
Legal Considerations
The primary legal consideration in treating depression in children is that they cannot make their own treatment decisions. Therefore, the main decision-makers are the parents or guardians of the child. The physician must inform the patient’s caregivers of the child’s condition and treatment progress. Furthermore, the doctor must inform the social workers if the parents were the main cause of the child’s depression.
Ethical Considerations
Ethical considerations in medical practice include not harming the patient and leaving the final decision on treatment to the patient. In the case of children, decisions about good medication should be made by the parents as the patients’ caregivers. It is essential that the healthcare professional offer the patient and their caregivers several treatment options with a description of their effects and possible side effects. In addition, the proposed options should be the most beneficial for the patient.
Cultural Consideration
A health worker caring for patients with depressive disorder should be culturally sensitive to the child. Selph and McDonagh (2019) note that racial, ethnic, and LGBTQ discrimination is a common cause of social exclusion leading to depression. The doctor’s task is to identify and reduce the influence of these factors on the patient’s mental state. In addition, cultural considerations include such concepts as the language barrier, an individual’s relationship with healthcare providers, and religious beliefs. Therefore, it is necessary to make sure that the patient and his caregivers understand the specifics of the condition and the importance of its proper treatment.
Social Determinants of Health
Social status affects the development of depression in children to the same extent as in adults. In particular, children from low-income families are more likely to experience depression due to poor living conditions (Bernaras, Jaureguizar, & Garaigordobil, 2019). The healthcare worker’s role is to offer alternative treatment options and assistance programs, including community-based organizations, that can be accessible to low-income families.
Further Information
Most often, depression occurs in school-age children, so several programs are aimed at preventing the development of the disorder. Most of these programs are designed for teenagers aged 11-12. However, Bernaras, Jaureguizar, and Garaigordobil (2019) note that there are programs for young children, including the Penn Resiliency Program (PRP), the Aussie Optimism Program, FRIENDS, and FORTIUS. These programs help children identify and express their emotions, which helps reduce their risk of developing depression.
In addition, programs perform a supportive function and contribute to establishing social interactions with the child. Another critical factor is that these programs perform an educational function. Moreover, these programs collaborate with medical professionals who specialize in mental disorders in children.
Conclusion
Therefore, children are one of the most vulnerable categories for developing depression. Drug treatment has many medical nuances and special considerations related to the age and status of the patient. The task of the attending physician is to provide comfortable medical treatment for patients, taking into account the legal, ethical, and cultural aspects. In addition, the doctor must consider the social determinants that affect the patient’s condition and the success of treatment.
References
Bernaras, E., Jaureguizar, J., & Garaigordobil, M. (2019). Child and adolescent depression: A review of theories, evaluation instruments, prevention programs, and treatments. Frontiers in psychology, 10, 543. Web.
Mullen, S. (2018). Major depressive disorder in children and adolescents. Mental Health Clinician, 8(6), 275-283. Web.
Selph, S., & McDonagh, M. S. (2019). Depression in children and adolescents: Evaluation and treatment. American family physician, 100(10), 609-617. Web.
U.S. Food & Drug Administration (2019). Depression Medicines. Web.
Zhou, X., Liu, L., Lan, X., Cohen, D., Zhang, Y., Ravindran, A. V., Yuan, S., Zheng, P., Coghill, D., Yang, L., Hetrick, S.E., Jiang, X., Benoliel, J.-J., Cipriani, A., & Xie, P. (2018). Polyunsaturated fatty acids metabolism, purine metabolism and inosine as potential independent diagnostic biomarkers for major depressive disorder in children and adolescents. Molecular psychiatry, 24(10), 1478-1488. Web.
Zhou, X., Teng, T., Zhang, Y., Del Giovane, C., Furukawa, T. A., Weisz, J. R., Li, X., Cuijpers, P., Coghill, D., Xiang, Y., Hetrick, S.E., Leucht, S., Qin, M., Barth, J., Ravindran, A.V., Yang, L., Curry, J., Fan, L., Silva, S.G., Cipriani, A., & Xie, P. (2020). Comparative efficacy and acceptability of antidepressants, psychotherapies, and their combination for acute treatment of children and adolescents with depressive disorder: a systematic review and network meta-analysis. The Lancet Psychiatry, 7(7), 581-601. Web.