Most of the patients in need of incubation tend to portray ventilation alterations. For this reason, they tend to experience bronchial secretion, which can complicate their evolution if not adequately controlled. Associated complications can lead to mucus plugs, atelectasis, and at times, super-infection, which favor the onset of nosocomial pneumonia. Research has not specified how the practice needs to be performed on adults living with endotracheal intubation. However, the institution’s protocols need to be followed and justify that the patients require aspirations depending on the secretion visualizations in the airways. Coughing attempts, agitation, shortness of breath, snoring, and anxiety is respiratory indicators of impairment. In this regard, patients need to be interrogated on whether they think aspiration is essential.
The scenario demonstrates a lack of proper guidelines on proper treatment intervention for pneumonia patients. For this reason, an appropriate treatment plan needs to be enacted and communicated to all nursing practitioners. To show the effect of saline installation and lack of it on the pneumonia risk, the following step by step plan is necessary:
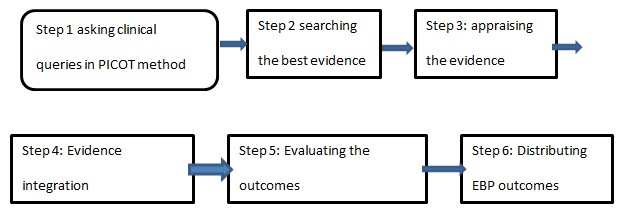
The first step involves evaluating a patient on a clinical ventilator to establish the effect of instilling the saline during suction compared to its absence. This helps in testing the risk involved in pneumonia in the patient. The second step consists in searching for the best indication using abstracts to establish evidence level. The third step will look at the accuracy of the results provided. The fourth step involves incorporating evidence provided with patient preferences and clinical expertise to determine the appropriateness of saline instillation. The next step will be used to test the effect of the saline in reducing pain and anxiety for patients. Finally, EBP results need to be disseminated through educational sessions and brochures.
The saline nebulization method can be applied compared to direct installation because the solution is uniformly spread in the lungs. This method ensures less influence of distribution by gravitation, enabling it to reach the edge of the lung to a considerable degree. In addition, the use of aerosol with particular characteristics helps optimize the fluid distribution along the distribution zone (Eekholm et al., 2020). This helps achieve more standardized humidification, making saline instillation unfit for mechanical ventilation. Typical saline installation can also lead to reduced oxygen saturation making it displace bacteria in endotracheal tubes (Eekholm et al., 2020). As portrayed in this case, the difference is a result of the lack of scientific reports that support the installation of saline.
Definition of Nursing Process and Clinical Decision-Making Process
In the long term, proper oral hygiene hand wash alongside good respiratory management helps reduce the severity of pneumonia in this category of patients. There are varied approaches that can help ensure desirable secretion control that aims to evacuate the exudate and curb complications:
Respiratory Physiotherapy
In critical care practice, chest physiotherapy encompasses vibration, drainage, and percussion of the chest wall and manual insufflation.
Postural Drainage
The change in position in TR implies the placement of particular segments of lungs greater than that of carina to help move secretions and utilize this measure in therapeutic. This change is also likely to enhance ventilation, decrease breathing, increase heart volume and facilitate proper secretion drainage. Postural changes need to be done after two or cone hours in patients with special needs for ICU ventilation, while postural drainage needs to be done in 4-6 hours.
Percussion and Chest Vibration
Vibration and percussion are two practical approaches traditionally applied to enhance airway clearance through the broadcast of energy applied to the chest wall. It is essential to realize that percussion can be done with dry blows and having hands in concave shape along the wall of the trunk of the affected region (McKinley et al., 2018). The drainage can be done through vibration by acceleration and manual flow accompanied by a rhythmic shift of either hands or squashing the chest wall during non-selective expiration. Similarly, vibration and percussion can be done by using mechanical equipment.
Mechanical or Manual Insufflation
This approach involves disconnecting a patient from a ventilator and ensuring lungs are well fit with sizeable tidal volume by using the mechanical instrument. The course is usually done with deep aspiration and slow supply, inspiration pausing and fast releasing the space to attain a high expiratory flow. This is done to end the chances of pulmonary collapse lung compliance and enhance oxygenation.
Endotracheal Suction
This is also known as ETA and is one of the most performed practices among artificial airway patients. This is part of bronchial hygiene and manual ventilation made of mechanical drag of pulmonary emissions originating from the synthetic airway to reduce the chances of its obstruction (McKinley et al., 2018). Depending on the tube selected, there are two common approaches to endotracheal suction. The first method is an open aspiration which necessitates a patient to be removed from a ventilator. On the other hand, the closed approach allows aspiration tubes to be distributed through an artificial airway without removing the patient from the ventilator.
In adults, the suction tube size needs not exceed half of the inner side of the artificial airway. During the aspiration preparation, it is expected to provide 100% oxygen for close to 60-30 seconds before the aspiration (McKinley et al., 2018). This should be done mainly to patients who are hypoxemic before the process. During this procedure, the advanced pressure of the unit needs to be checked by obstructing the end of the suction tubes right before connecting the probe suction and before any suctioning act. In this regard, it is required that the suctioning pressure be as low as possible while ensuring effectiveness in secretion extraction. Although this is an essential procedure, it is necessary to realize that it is capable of causing complications such as pain, tracheal mucosa injury, infection, discouragement, and alterations in hemodynamic parameters. Other probable injuries include atelectasis, arterial gasses, amplified arterial gasses, and bronchoconstriction.
The above EBP plan will help nursing practitioners avoid the unnecessary endangering of patients in evidence-based practice. In this regard, whenever one encounters a patient in a mechanical ventilator, it is required first to ensure the person is adequately hydrated, use mucolytic agents, and encourage the patient to move around. Moreover, the plan helps in improving the level of patient care by providing necessary information that discourages saline use in the event of suction (McKinley et al., 2018). Proper application of this plan will help ensure patients recover faster by using EBP.
It is clear from the above analysis that saline has limited time on oxygen therapy, ventilators, and intensive care. The information also helps practitioners explain to other nurses the need to avoid the use of saline during suction. It is clear from this that instilling saline increases VAP chances and lowers the respiratory tract. These undesirable outcomes cause more harm to antimicrobial characteristics in respiratory hypoxemia, cardiac arrest, infection, and bronchospasm.
References
Eekholm, S., Ahlström, G., Kristensson, J., & Lindhardt, T. (2020). Gaps between current clinical practice and evidence-based guidelines for treatment and care of older patients with Community Acquired Pneumonia: a descriptive cross-sectional study. BMC infectious diseases, 20(1), 1-12.
McKinley, D. F., Kinney, S. B., Copnell, B., & Shann, F. (2018). Long-term effects of saline instilled during endotracheal suction in pediatric intensive care: A randomized trial. American Journal of Critical Care, 27(6), 486-494.