Definitions
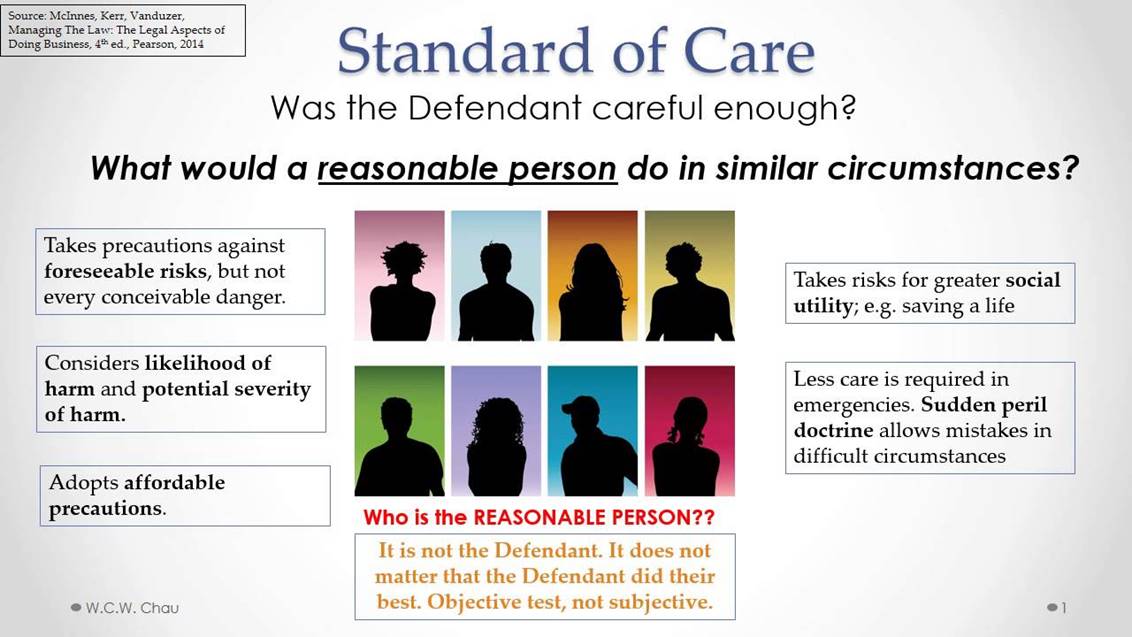
- Standard of care – reasonable and ordinary care, skill or diligence given by practitioners in good standing.
- Malpractice – failure of professional skill that results in injury or damage (Buppert, 2018).
- Risk of liability – a medical professional can be found legally responsible for a mistake if found to have acted negligently by breaching the standard or duty of care.
These are basic definitions for terms that will be seen commonly in this presentation regarding adherence to the standard of care and malpractice. As evident, they are all inherently intertwined. The standard of care is a professional and ethical duty that nurses have in their jobs. Malpractice is a failure to fulfill this duty, resulting in the risk of liability, a legal aspect which allows involved parties to sue for damages.
Key Elements of Malpractice
If being sued for malpractice, the plaintiff must prove four components of negligence:
- A medical professional owed a duty.
- The medical professional breached the standard of care.
- The injury sustained came as a direct result of that breach (causation).
- Resulting damages must also be proven (Urology Times, 2016).
Any lawsuit that alleges malpractice will being with a summons and a formal complaint of negligence. Most commonly, these state that the medical professional failed to adhere to the applicable standard of care by failing to properly diagnose or treat the patient. The components listed on this slide must be proven, with admissible evidence as it would be in any court case. It is important to note that the standard of care will vary based on jurisdiction since it is not universal across states (Urology Times, 2016).
Malpractice is a legal term for an act of negligence:
- It is the failure to use reasonable care or improper and unethical conduct or unreasonable lack of skill by a holder of a professional position (Watson, 2014).
- Improper performance, failure to adhere to procedure, failure to adhere to the standard of care, and failure to communicate or obtain patient informed consent are most common malpractice issues.
- Malpractice coded payouts include injury include death, grave permanent injury, and minor permanent injury (Jordan, Quraishi, & Liao, 2013).
The rapidly changing healthcare environment is causing nurses to face ethical and legal challenges without proper guidance or protocols, increasing the risk of being included in a malpractice litigation process. Nurses are being held accountable to patients and the public for professional judgments, actions while on duty and outcomes. Malpractice can be avoided by practicing competent care, identifying risks, and using evidence-based approaches to treatment.
Regulatory Compliance in Practice
- Family practice and adult/geriatrics are the highest nurse specialties for liability claims (Watson, 2014).
- Malpractice claims are rising against nurse practitioners.
- The changes in the scope of practice result in APRNs being the only culpable party (Miller, 2013).
- Strict regulations leading to the dismissal of noncompliant patients.
- Healthcare providers fearful of liability are pursuing options to avoid troublesome or noncompliant patients (Stelmach, 2015).
Regulatory compliance has become increasingly important as policies have become stricter and malpractice suits have risen year over year. APRNs hold significantly more responsibility for clinical practice and have the authority to diagnose and treat patients independently of physicians, which places the responsibility on them in cases of malpractice. In turn, this may have negative consequences such as providers turning away noncompliant patients.
- Gerontology is an evidence-based nursing specialty focusing on addressing the concerns of older adults.
- Standards include a professional performance with maintaining practice competency.
- All aspects of the nursing process: assessment, diagnosis, planning, implementation, and evaluation.
- Professional level of behavior in the role, including ethical, communication, cultural, education, leadership, quality, and environmental health among others (Bickford, 2018).
In terms of what it means to adhere to regulatory compliance in gerontological nursing, it differs very little from standard nursing practice. The practice is focused on older adults, who are more physiologically fragile. They require a more caring and thorough approach in aspects such as patient education and communication since there are potential concerns for misunderstanding. Professionalism and patience are vital in this specialization.
State Coding Compliance Issues
- Patients signed up for and billed for out of network services without consent.
- Improper diagnostic coding procedures, including those regarding transfers and readmissions.
- Need for improved recordkeeping and identification of common errors in patient records.
- Opens up exposure to malpractice lawsuits.
These state coding compliance issues are similar to those of federal ones discussed in the next slide. It is important to discuss how these errors ultimately place NPs under liability for violating the standards of care by improperly billing or documenting a patient. It creates a potential for a lawsuit under categories such as failure to get informed consent from a patient or failure to adhere to standards of care in diagnosing and treatment. Following coding protocols is considered one of the best ways to ensure nursing competency.
Federal Coding Compliance Issues
- Documentation – poor documentation issues and inconsistency among providers, including limited utilization of EHR and proper procedures.
- Coding – incorrect principal diagnosis selection and subsequent assignments of comorbidities of HAI complications.
- Query process – conflict information or documentation as a result of errors in the categories above (AHRQ, n.d.).
As evident, the federal coding compliance issues largely match the state of practice problems. These aspects on a national level are much larger and critical since the government reimburses states and healthcare providers based on their coding and documentation. These issues, however, create a potential for administrative or clinical errors on behalf of the medical staff that leads to malpractice. Misplaced documentation or a wrong coding of a diagnosis can significantly impact or delay competent care, placing the NP entering the data at risk of liability.
Legal Implications
- Federal regulations require compliance with standards of care to be eligible for Medicare participation from healthcare providers.
- Failure to comply may lead to criminal and civil liability from the government.
- If an NP fails to adhere, it may result in a negligence lawsuit.
- Failure to comply with state regulations regarding nursing practice may lead to loss of license and criminal charges in severe cases (Lockhart, 2017).
When negligence is committed by a nurse, it places them at jeopardy of legal risk, from both the patient as well as the government. For example, Medicare fraud is often investigated when incorrect coding is selected for billing, even if unintentionally. Meanwhile, if the patient is harmed, there is a potential for a malpractice suit if all the factors listed previously are present.
- Risk of disciplinary action by nursing boards.
- Successful malpractice claims result in significant costs.
- Average judgment payout of $282,297 per claim (Watson, 2014).
- Risk of poor-quality ratings from the healthcare provider.
Continuing from the previous slide, a board of nurses may choose to review conduct on criminal charges if grossly negligible or purposefully unethical actions that may result in temporary or permanent loss of license. Overall, negligence claims have significant trickle-down effects on costs, which range in the hundreds of thousands of dollars in payouts, legal fees, and penalties. Furthermore, the healthcare provider may face poor-quality ratings for some time which organizations must legally make public. As a result, the Medicare and Medicaid eligibility of healthcare providers may be potentially reviewed for failure to comply with performance measures.
Malpractice Policy Options
- Standards of care are based on professional standards, scopes of practice, legislation, and local facility policies and protocols.
- Regulation is necessary but medical malpractice law creates unnecessary pressure without significantly improving quality.
- Practitioners often go overboard by ordering additional tests or treatments to protect against lawsuits.
- Malpractice policy should focus on the deterrence of errors by imposing expectations regarding quality rather than liability (Frakes & Jena, 2016).
Standard of care regulation is complex as it is evidently necessary to maintain a high quality of service and offer guidelines. However, in the context of malpractice, practitioners should not fear liability for any potentially non-standard action or situation which may commonly occur in medical care. It is difficult to find a balance in policy that both promotes quality and eliminates purposefully negligent behavior while protecting those who committed a mistake.
- Medical malpractice insurance is a specialized concept of professional liability insurance, required in most states and healthcare systems to practice.
- Malpractice insurance policy options vary by circumstance.
- Claims-made policies – lower premium, gap coverage, risky.
- Occurrence policies – higher base premium, universal claims coverage.
The rise in claims has made medical malpractice insurance a necessity in most places to cover the multi-hundred thousand-dollar costs of the lawsuit. Usually, there is no difference in the type of damage coverage, but rather when the policy is triggered. Claims-based policies often lower premium which increases as policy matures, reaching a maximum at some point. Leads to gaps in coverage that is risky since policy must be active during the malpractice incident and when a claim is filed. Occurrence policies cover any claim for negligence during the coverage period, even if the lawsuit was filed afterward (American College of Physicians, n.d.).
Risk Management
- All NPs face risks in clinical practice.
- Vital to practice litigation avoidance techniques.
- Upkeeping on information regarding the standards of care.
- Avoiding careless errors such as breach of confidentiality or giving medical advice in unofficial settings (Buppert, 2018).
- Promote institutional protections such as clearly written protocols and supervision of NPs.
In conclusion, the primary theme of this presentation regarding adhering to the standard of care comes down to risk management. NPs will always face clinical and business-related risks in practice. There is always the potential of malpractice suits from dissatisfied or disgruntled patients. However, if an NP knows and understands the standards of care including policy and written protocols, there should be no issues at mitigating any risk. These factors serve as vital protective measures on an individual and institutional level.
References
AHRQ. (n.d.). Documentation and coding for the AHRQ quality indicators.
American College of Physicians. (n.d.). Medical malpractice insurance.
Bickford, C. J. (2018). A contemporary look at gerontological nursing.American Nurse Today, 13(6), 48.
Buppert, C. (2018). Nurse practitioner’s business practice and legal guide (6th ed.). Sudbury, MA: Bartlett & Jones Learning.
Frakes, M., & Jena, A. B. (2016). Does medical malpractice law improve health care quality? Journal of Public Economics, 143, 142-158. doi:10.1016/j.jpubeco.2016.09.002
Jordan, L. M., Quraishi, J. A., & Liao, J. (2013). The national practitioner data bank and CRNA anesthesia-related malpractice payments. American Association of Nurse Anesthetists Journal, 81(3), 178-182.
Lockhart, L. (2017). Nurses under investigation.Nursing Made Incredibly Easy, 17(2), 55.
Miller, K. P. (2013). The national practitioner data bank: An annual update. The Journal for Nurse Practitioners, 9(9), 576-580.
Stelmach, E. I. (2015). Dismissal of the noncompliant patient: Is this what we have come to? The Journal for Nurse Practitioners, 11(7), 723-725.
Urology Times. (2016). You’ve been sued for malpractice: What happens next. Web.
Watson, E. (2014). Nursing malpractice: Costs, trends and issues. Journal of Legal Nurse Consulting, 25(1), 26-31.