Introduction
- Opioid crisis – a serious public health issue;
- Opioids commonly abused;
- Heroin & prescription opioid medications, e.g., codeine;
- Highly addictive – induce endorphin release (Mayo Clinic, 2018);
- Opioid abusers are a vulnerable population:
- Potential addiction & mental disorders;
- Injection-related infections & death from overdose;
- Limited access to addiction interventions.
The rising rate of opioid use raises serious public health concerns. The potential for addiction to opioids like heroin and prescription medications for short-term pain relief, such as methadone, is high (Hahn, 2011). These substances bind to opioid receptors in the brain to induce endorphin release, which causes short-lived pleasure effects (Mayo Clinic, 2018). Besides the risk factors that lead to opioid misuse, issues of addiction, mental disorders, injection-related infections, overdose deaths, and limited access to treatment make opioid abusers a vulnerable population.
Health Risks & Substance Abuse
- Known health risk of opioid use are:
- Injection-related infectious diseases, e.g., hepatitis C & HIV/AIDS (Dan & Giroir, 2018);
- Overdose deaths – oral/parenteral route causes a fast release;
- Drug dependence & addiction (Mayo Clinic, 2018);
- Opiate withdrawal symptoms;
- Psychological effects: euphoria, respiratory depression, etc. (Dixon & Xiong, 2018).
Substance abuse is linked to poor health outcomes. Dan and Giroir (2018) identify injection-related infections, such as hepatitis C and HIV/AIDS, and deaths resulting from a drug overdose as the primary effects of opioid abuse. Specifically, oral or parenteral administration causes a fast release of these formulations, resulting in euphoric states, respiratory depression, and suppressed pain sensation (Wixon, 2018). The short-lived pleasure effects associated with opioid use increases the risk of repeated abuse and addiction (Mayo Clinic, 2018). Other health risks include decreased gastrointestinal motility, nausea, and vomiting.
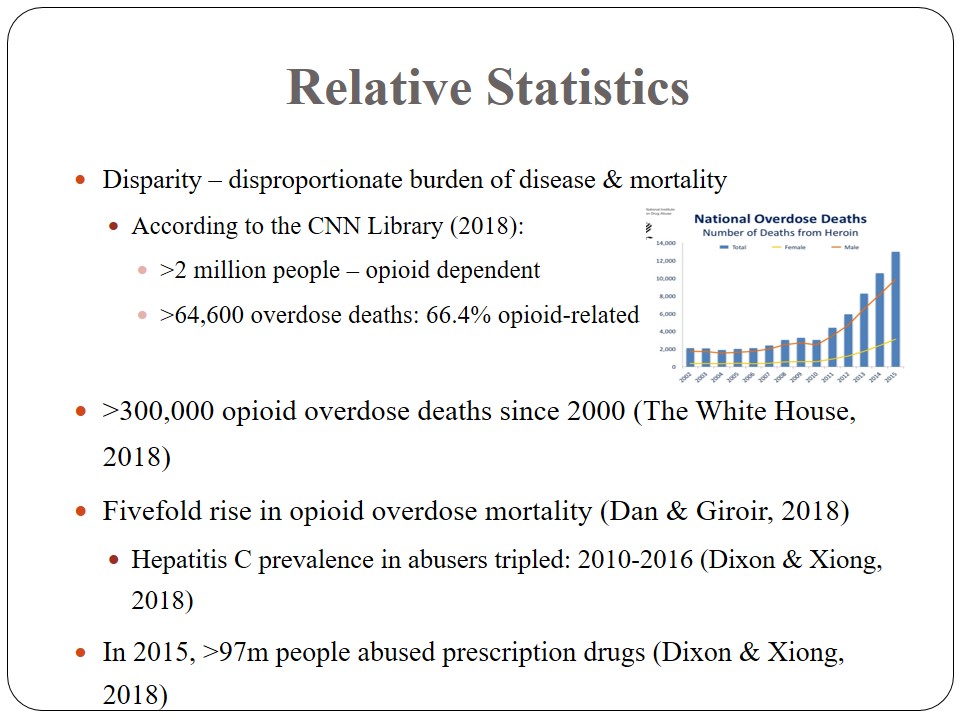
Relative Statistics
- Disparity – disproportionate burden of disease & mortality:
- According to the CNN Library (2018):
- >2 million people – opioid dependent;
- >64,600 overdose deaths: 66.4% opioid-related;
- >300,000 opioid overdose deaths since 2000 (The White House, 2018).
- According to the CNN Library (2018):
- Fivefold rise in opioid overdose mortality (Dan & Giroir, 2018):
- Hepatitis C prevalence in abusers tripled: 2010-2016 (Dixon & Xiong, 2018).
- In 2015, >97m people abused prescription drugs (Dixon & Xiong, 2018).
Disparities in morbidity and mortality rates exist between substance abusers and other populations. The CNN Library (2018) estimates that over two million people are either opioid dependent or have misused prescription drugs. Overdose deaths in this population are about 64,600 annually, adding up to 300,000 mortalities since 2000 (The White House, 2018). A threefold increase in hepatitis C prevalence among abusers was reported between 2010 and 2016 (Dixon, 2018). A fivefold increase in opioid overdose mortality was recorded over the same period.
Health Impact
- Social issues related to opioid use:
- Opioid addiction & dependence;
- Stress, domestic violence & abuse;
- Unproductive society;
- Family or marital problems;
- Poor educational outcomes – young age;
- Problems with law enforcement (antisocial personality);
- Risk of injection-related infections;
- Mental disorders:
- Comorbid mood/anxiety disorders, e.g., paranoid disorder & borderline disorder.
- Risky or thrill-seeking behavior;
- Heavy tobacco use;
- Severe depression or anxiety;
- Risk of fentanyl poisoning – cocaine adulteration (Katz, 2017).
- Environmental issues – vulnerability results from:
- Poor or disadvantaged neighborhoods – Appalachia:
- High overdose deaths in Appalachia & New England (Katz, 2017).
- Limited access to quality treatment;
- Lower literacy levels – social status;
- Social exclusion and isolation;
- Environmental stress – dull environments;
- An influx of cheap opioids, e.g., fentanyl.
- Poor or disadvantaged neighborhoods – Appalachia:
- Economic issues: increased health utilization costs:
- Cost of addiction & treatment:
- More physician visits;
- Mental health services – $6bn for opioid 2018 programs (CNN Library, 2018);
- Hospital admissions;
- ED visits;
- Physical or emotional trauma;
- Substance abuse therapy (Hahn, 2011).
- Cost of addiction & treatment:
- Economic issues:
- Medical expenses – treatment of comorbidities – hepatitis C:
- High prescription costs: >5 times that for nonabusers;
- Drug dependence.
- Legal ramifications – drug-related crime;
- Wages and employment – unproductive society;
- Absenteeism from work:
- Reduced productive time.
- Fatal cost – overdose-related deaths.
- Medical expenses – treatment of comorbidities – hepatitis C:
- Cultural issues:
- Lifestyle appeal – nonmedical opioid use (euphoria):
- Administration: snorting (62%) & IV (26%) (Hahn, 2011).
- Misuse of prescription (pain relief) drugs;
- Relief from stress;
- Peer influence;
- Availability of cheap opioids;
- Poor regulatory safeguards.
- Lifestyle appeal – nonmedical opioid use (euphoria):
Opioid use is linked to various effects on social health. First, it leads to the problem of opioid addiction or dependence that affects normal functioning. It also a risk factor for psychological stress, domestic violence, and abuse (Dixon & Xiong, 2018). Opioid addiction often predisposes individuals to poverty, unemployment, and family problems or broken relationships due to impaired social functioning. Young abusers are likely to report poor educational outcomes and criminal behavior or legal problems. The risk of infections, including HIV/AIDS, is also high because of the sharing of injection needles among addicts.
Other social consequences of substance use include a predisposition to psychiatric disorders, including comorbid mood and anxiety disorders. Poor mental health is a serious problem faced by users that impacts their relationships and well-being in the society. Opioid abusers may also exhibit risky or thrill-seeking behaviors, exposing themselves to health hazards or sexually transmitted infections. Recreational use of opiate derivatives or prescription drugs will lead to heavy tobacco use, which increases the risk of respiratory problems and lung cancer (Katz, 2017). These chronic conditions reduce the productivity and quality of life of the addicts. It also increases the risk of fentanyl poisoning due to cocaine adulteration.
Opioid use affects and is shaped by a host of environmental factors. It is highest in poor or disadvantaged regions. Katz (2017) demonstrates that trends in opioid use show a geographical variation with disproportionate overdose deaths reported in impoverished areas such as Appalachia. These regions have a limited access to treatment, lower literacy levels or social status, and an influx of cheap opioids like fentanyl. Exposure to environmental stress also increases the likelihood of substance use. Dull environments that are devoid of opportunities for interpersonal interaction and support can also predispose individuals to substance abuse. Social exclusion and isolation of addicts render them homeless and destitute.
The economics of opioid use highlight the scope of the problem of substance abuse and its impact on the healthcare system. Opioid addicts make more physician or ED visits than non-users do. They are also heavy users of inpatient mental health services, trauma care, and substance abuse therapy (Hahn, 2011). Medical costs for this population is up to “eight times higher than for non-abusers”, i.e., $15,884 versus $1830 per individual (Hahn, 2011, p. 109). Thus, the cost burden of opioid abuse to the health care system and health insurance is significant. Increased federal spending on addiction treatment and rehabilitation will affect primary care in other critical areas.
The medical expenses related to opioid use have a significant impact on the healthcare system. Specifically, the treatment costs for comordities, such as hepatitis C, and fantanyl poisoning are higher among abusers than non-abusers (Hahn, 2011). There is also the issue of high spending on prescription drugs. Another economic aspect is the legal ramifications of opioid use. Abusers are more likely to engage in crime, straining law enforcement resources and correctional facilities. Opioid abuse creates an unproductive society, increases absenteeism from work due to drug dependence effects, and can lead to death.
A number of cultural stressors aggravate the problem of opioid abuse. A culture of lifestyle appeal drives many people to use nonmedical opioids for relaxation and euphoria. The preferred routes of administration by 62% and 26% of users include snorting and injection, respectively (Hahn, 2011). The misuse of prescription drugs without physician directions, availability of cheap opiate derivatives, and poor regulatory safeguards are other cultural issues exacerbating this problem. The nonmedical use of opioids is meant to bring relief from stress and pain. Peer influence and alcohol abuse also contribute to the abuse of hard drugs, including opioids.
Recommendations
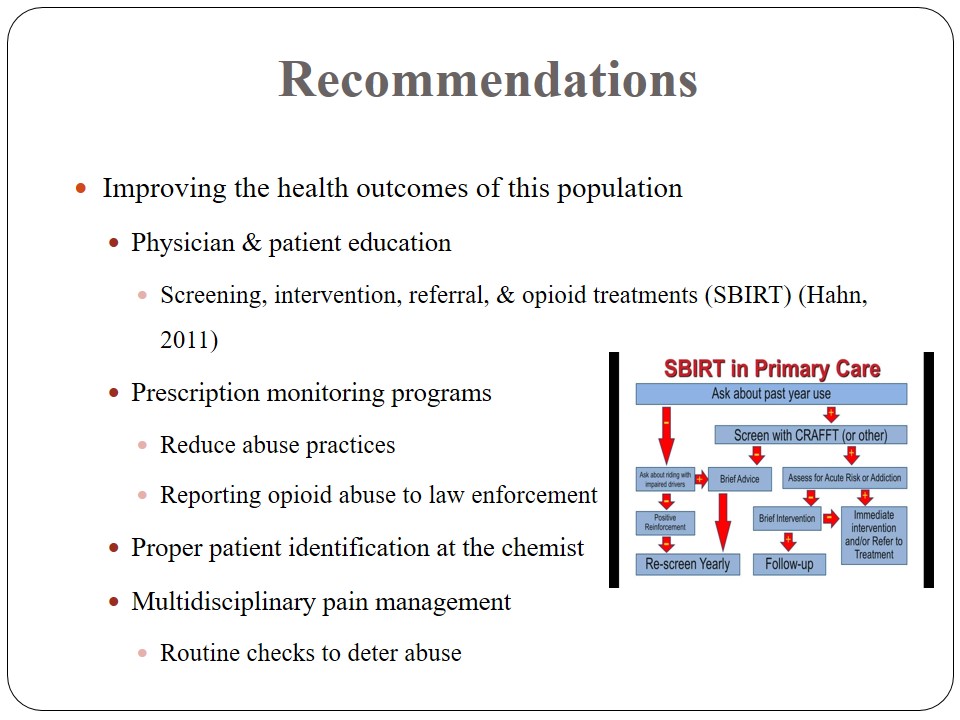
- Improving the health outcomes of this population:
- Physician & patient education:
- Screening, intervention, referral, & opioid treatments (SBIRT) (Hahn, 2011);
- Prescription monitoring programs:
- Reduce abuse practices;
- Reporting opioid abuse to law enforcement;
- Proper patient identification at the chemist;
- Multidisciplinary pain management:
- Routine checks to deter abuse;
- Physician & patient education:
- The release of abuse-deterrent formulations:
- Slow-release properties.
- Neutralizing antagonists.
- Unpleasant side effects (Hahn, 2011).
- Controlled opioid distribution.
- Access to addiction treatments, e.g., methadone (Katz, 2017).
- Safe injections:
- Medical supervision of injection-drug addicts.
Diverse measures are recommended for improving the health outcomes of opioid abusers. Physician education on effective tools for screening, intervention, referral, and treatment (SBIRT) can help identify and help at-risk individuals (Hahn, 2011). Provider-led prescription monitoring programs can be crucial in reducing abuse practices. These measures may involve reporting patients abusing opioids to law enforcement. Proper identification of the patient at the point of sale is recommended to restrict or control nonmedical use of these drugs. Additionally, multidisciplinary pain management approaches can also improve this population’s health outcomes. Referrals to specialists that use alternative methods will help curb the problem of opioid and prescription drug abuse.
Supply-side variables can also help improve the health outcomes of substance users. Pharmaceutical firms are developing drugs that could counteract the effects of opioid abuse and addiction. Among the mechanisms of action considered in designing these formulations are slow-release properties, neutralizing antagonists to deter overdose, and unpleasant side effects at high dosage levels (Hahn, 2011). Other measures with a potential to reduce the health outcomes of the abusers include controlled distribution of the drugs and the provision of addiction treatments like methadone (Katz, 2017). Medical supervision can also ensure safe injections to prevent infections such as hepatitis C and HIV/AIDS.
Policy Changes
- Adequate appropriation for medication-based addiction treatment (Katz, 2017).
- Removal of barriers to Medicaid coverage.
- Legislations promoting private health insurance.
- Prosecuting prescribers flouting the law.
- Electronic prescribing policies at the hospital level.
- Safe opioid prescribing.
- Severe penalties for drug trafficking.
- Preventive measures – educating people on opioids & effects.
Policy changes are required to tackle the opioid crisis in the country. In this view, ensuring adequate appropriation for medication-based addiction treatment and removing Medicaid barriers to inpatient care for addiction are necessary (Katz, 2017). Mandatory coverage of addiction-related treatment by private insurers would also improve the outcomes of opioid addicts. Prosecuting prescribers flouting the FDA-approved dosage levels would deter substance misuse. At the hospital level, electronic prescribing would prevent medication errors. Severe penalties for drug trafficking and awareness programs can also prevent opioid abuse.
References
CNN Library. (2018). Opioid crisis fast facts . Web.
Dan, C., & Giroir, B. P. (2018). Integrating infectious disease prevention and treatment into the opioid response. Web.
Dixon, W. D., & Xiong, G. L. (2018). Opioid abuse. Web.
Hahn, K. L. (2011). Strategies to prevent opioid misuse, abuse, and diversion that may also reduce the associated costs. American Health & Drug Benefits, 4(2), 107-114. Web.
Katz, J. (2017). Short answers to hard questions about the opioid crisis. The New York Times. Web.
Mayo Clinic. (2018). How opioid addiction occurs. Web.
The White House. (2018). The opioid crisis. Web.