Abstract
This study analyzes heliox therapy as a medical intervention that is done using oxygen and helium to aid in the process of alleviating various respiratory distresses. Heliox therapy has been in use in the medical field since 1935 when it was first used in the treatment of asthma (Brandao & Britto et al., 2011, p.948).
It is also used as a medical intervention of COPD (Chronic Obstructive Pulmonary Disease) (Allan & Thomas et al., 2009, p.1175) and bronchiolitis. Before the use of helium as a carrier gas, nitrogen was used as the carrier gas for oxygen. This makes helium easy to inhale, hence facilitating rapid oxygen absorption in the blood stream.
The study also presents a description of a psychological problem and in particular the problems experienced by acute asthmatic people in terms of carbon dioxide exchange. As a therapy option, a gas mixture of nitrogen and oxygen can be administered into the blood stream of a patient to supply the necessary oxygen deficit in the effort to minimize the work required to absorb adequate air to meet the oxygen needs of patients. Another alternative is to use helium-oxygen gas mixture in a therapeutic intervention referred as heliox therapy.
Further, the study provides an overview of the associated diseases including clinical and physiologic effects. The study also provides the technical considerations when giving the heliox therapy. Besides, it offers the positive effects that the therapy has on acute asthmatic patients. Finally, the study provides the role played by a therapist when giving any therapeutic intervention.
Description of the Physiologic Problem
Acute asthmatic people have problems in carbon dioxide exchange. Before medicinal interventions are done, it is necessary for short-term interventions in the preparation of medicinal interventions to be conducted to ensure that patients awaiting treatment have sufficient carbon dioxide exchange. Among the alternatives available for physiologic experts are mechanical ventilations, bronchodilators, and ticosteroids among others.
While attempting to address this problem, consideration of scholarly evidence on the effectiveness of heliox therapy in the treatment of respiratory infection is important. Yilmaz, Daglioglu, and Yildizdas et al. (2013) did a research on the effectiveness of heliox in acute respiratory distress syndrome where they found out that heliox is associated with positive responses of ARDS inflation apart from having positive impacts on the treatment of obstructive lung ailments (p.47).
Since 1930s, heliox has been used in the treatment of reparatory ailments even before bronchodilators were invented. In the modern age, heliox is normally deployed in situations involving the narrowing of the large airway passages due to tumors (Yilmaz, Daglioglu &Yildizdas et al, 2013). However, it is also used for medium airways, especially in case of asthma and COPD (Hess et al., 2006). Heliox is also deployed in other medical interventions involving difficulties in availing adequate oxygen to the patients’ body systems.
For instance, upon studying the effects of shifts of breathing gas from air to heliox mixtures on the resolution of air bubbles in lipid and aqueous tissues of recompressed rats, Hyldegaard, Kerem, and Melamed (2011) concluded that there should be no delays in the deployment of heliox in the treatment of “air driving induced-decompression sickness” (p.2183).
This suggests that heliox therapy can be utilized as a therapeutic intervention for all respiratory problems in patients waiting medical intervention since heliox has no curative effect.
Overview of the associated Diseases including Clinical and Physiologic effects
Heliox therapy can be used in the treatment of asthma and COPD. The application of heliox in the therapeutic intervention for asthma attracts controversy. In a meta-analysis research involving four random trials for treatment of acute asthma using heliox in an emergency care setting conducted on adults together with children by Rodrigo, Rodrigo, Pollack, and Travers as quoted by Chevrolet (2001), no evidence of the effectiveness of heliox was recorded (p.180).
Studies done by Hurford and Cheifetz (2007) and Kneyber et al. (2009) record high rates of airflow when heliox is used in place of airox for patients who are not intubated. There is scholarly agreement that heliox has no curative impact on the treatment of crisis involving acute asthma. This implies that heliox should never be used as a replacement of corticosteroids therapy and/or bronchodilators.
Chevrolet (2001) insists that heliox should be used as a therapeutic intervention for acute asthma following the failure of bronchodilator therapy in managing the condition (p.181). Resorting to heliox on the failure of bronchodilator therapy eliminates the necessity of intubation. Chevrolet (2001) maintains that this procedure is an immensely dangerous therapeutic intervention for people suffering from acute asthma (p.182).
However, heliox has also been used in patients who have been intubated in the medical history of treatment of asthma. For such patients, heliox has been found to produce positive outcomes through enhancing reduction of pressure of inflation (Chevrolet, 2001). This makes the therapy important for persons having ventilation difficulties accompanied by hemodynamic instability.
Another associated disease for heliox is COPD. Heliox is used in COPDs who are intubated, or not intubated (Randsoe, Kvist & Hyldegaard, 2008, p.1493; Myers, 2006, p.620). In the treatment of COPD, the standard medical approach is to start with NIV. When COPD patients are acutely decompensated, probabilities for respiratory failure increase often leading to high WOB (Palange & Valli et al., 2004, p.1639).
To minimize the chances of occurrence of fatigue of inspiratory muscles, NIV is administered. Scholars such Allan and Thomas et al. (2009) and Venkataraman (2006) confirm that WOB can be reduced further when NIV is combined with heliox. Heliox reduces the work of breathing in two major ways. It increases the tendency of laminar flow of oxygen within the respiratory system of a patient while reducing airflow resistance due to turbulence.
Hess et al (2006) evidence this effect by arguing that where laminar flow occurs in small air passages, gas viscosity is directly related to the viscosity. In such passages, this suggests that heliox possesses minimal effects on WOB. However, in large passages, turbulence flow occurs. In such a situation, the resistance to flow of a gas is related directly to the density of the gas flowing through the passages (Hess et al., 2006). This means that heliox has incredible effects in reducing WOB.
Technical Considerations of the Therapy
Various scholarly findings exist on the effectiveness of heliox therapy in producing positive effects for persons suffering from respiratory diseases. However, certain difficulties may make the therapy not common in all hospitals across the world. Technical challenges are one of the difficulties.
Successful administration of heliox therapy requires the possession of some prescribed technical expertise (Gupta, Grayck, & Cheifetz, 2004, p.1041). The equipment deployed in the process is also expensive. Debate also continues to develop on the consideration of the overall benefits of heliox therapy when gas concentration levels differ. Particular interest is on the development of guidelines on the specific levels of concentration of oxygen and helium that should be used for treatment of different respiratory ailments under specified circumstances.
Technical expertise is important in the use of heliox therapy. When the mixture of the gases is used at less than 36 degrees centigrade, hypothermia may be experienced.
There are technical difficulties of ensuring that the right amount of the gas mixture is delivered to meet the patients’ specific needs. Where heliox is used for patients who breathe spontaneously, pressurization of heliox in the ratio 78 (helium) to 22 (oxygen) is necessary (Chevrolet, 2001). Although helium is a largely profuse constituent in the world, its mining procedures are expensive.
In this line of argument, Chevrolet (2001) puts the cost of a 60-liter tank for heliox (78:22 helium-oxygen mixtures at 200 bars) at 275 US dollars in Switzerland. Upon considering issues of uncertainness of the possible stay of patients in ICU and the benefits of the use of heliox in the effective management of the patients’ respiratory diseases, reduction of this cost is necessary. This presents technical challenges in terms of looking for new cost-effective methods of production of heliox.
Positive effects of the Therapy
Asthmatic people experience challenges of airflow obstructions causing hyperinflation of lungs. The challenges result in an increase in the work required for inhalation processes. This introduces mechanical disadvantages to the inspiratory muscles to an asthmatic person (Brandao & Britto et al., 2011, p. 298).
Helium provides an advantage compared to nitrogen due to its lower density (Hess et al., 2006, p.605). Over the years, heliox has been used for medical applications, which do not involve respiratory ailments. It is also used in the treatment of ailments such as fractional obstruction of airways due to growths associated with malignancy together with engorgement of the esophagus.
Such swellings may be caused by allergic infections and/or anaphylaxis. Under such conditions, heliox finds applications in that it helps in the provision of the required oxygen levels while ensuring that such people do not incur the inspiratory muscle mechanical disadvantages.
Effectiveness of the use of heliox in medical interventions of asthma is enhanced by its properties compared to air. Its density is less than that of air. Consequently, compared to air, heliox has a lower resistance to flow in the airways. Ultimately, “WOB (work of breathing) is reduced” (Chevrolet, 2001, p.179).
Many health institutions recognize the deployment of heliox in the treatment of respiratory related ailments to the extent that respiratory therapists encourage the keeping of gas cylinders of heliox within hospitals for emergency care services. Amid its effectiveness as a therapeutic intervention for respiratory infections, heliox administration is done with optimal monitoring and vigilance (Gupta, Grayck & Cheifetz, 2004, p.1041).
Monitoring is done using chest radiographs and various mechanisms of monitoring arterial gas in the effort to provide a means of determining lung volumes together with gas exchanges (Gupta, Grayck & Cheifetz, 2004, p.1041). Gupta, Grayck, and Cheifetz (2004) studied the effects of heliox and high-frequency jet ventilation on a five-year old infant suffering from acute conditions of respiratory failure due to gas trappings, acidosis, and air leak.
Heliox therapy produces positive effects for patients with respiratory problems, which result in increased work of breathing. Myers evidences positive effects on the use of NPPV in the reduction of intubation rates for some patients who are carefully selected for treatment of acute respiratory ailments (2006, p.622). When Heliox is used in conjunction with NPPV, patients depict even better response rates, especially in case of those having COPD (Palange & Valli et al., 2004, p.1639).
While various studies such as Hess and Chatmonqkolchart (2000) present the benefit of increased survival rate on the use NPPV particularly for patients having respiratory failures related to COPD, deployment of heliox has positive effects when used in the treatment of patients having severe obstruction of airways or asthma.
Adverse effects/Hazards
In practical applications of heliox therapy, no substantial effects on patients have been recorded. Indeed, according to Hunt, Wiliams, Frith, and Schembri, heliox mixtures are nontoxic and do not produce any long lasting impacts on the patients’ bodies (2010, p.30). The only determinant of the mixing ratio is the mixture flow characteristic. Airflow within airways occurs through laminar, then transitional flow, and finally through turbulent flow.
High resistances characterize turbulent flow as evidenced by higher Reynolds number (Hess et al., 2006). While air may be enriched with oxygen for use in place of helium, it has a higher tendency of changing from laminar to turbulent flow in comparison with heliox since it has a higher density (Hess et al., 2006, p.605). The density of heliox at 1 atmosphere is 0.5g/l compared to 1.25 g/l for of air (Hunt, Wiliams, Frith & Schembri, 2010).
Low density ensures that a maximum amount of oxygen is delivered through the body systems of the patient with minimal work of breathing (WOB). Air, helium, and nitrogen are used as carrier gasses. A carrier gas should have minimal adverse effects on the patient if any.
No negative effects on the patients have been recorded on the use of air, nitrogen and Helium as carrier gases. Hunt, Wiliams, Frith, and Schembri further inform that heliox gas mixture of 79 percent helium and 21 percent oxygen has equal viscosity to identical gas mixtures where nitrogen is used in place of helium where heliox has one-sixth of the density of the nitrogen oxygen mixture (2010, p.30).
This inclusion of a high percentage of helium in the heliox gas mixture is influenced by the low-density property in comparison to nitrogen rather than medical effects or hazards. However, even though heliox has no adverse effects on the patient, Hess and Chatmonqkolchart (2000) maintain that it has adverse effects on the functioning of the respiratory care facilities and equipment (p.161) including function monitors for pulmonary, ventilators, nebulizers, and flow meters.
Role of the Respiratory Therapist
In case of heliox therapy, respiratory therapists are important. They make decisions on whether the therapy should be administered to patients. In an effective use of heliox therapy, therapists have to address the question of whether the physiologic problem revealed by patients can be treated at least in the short term before medicinal interventions are introduced through heliox therapy or a combination of various therapeutic interventions. The chart below shows how therapists go about administering the therapy for asthmatic people.
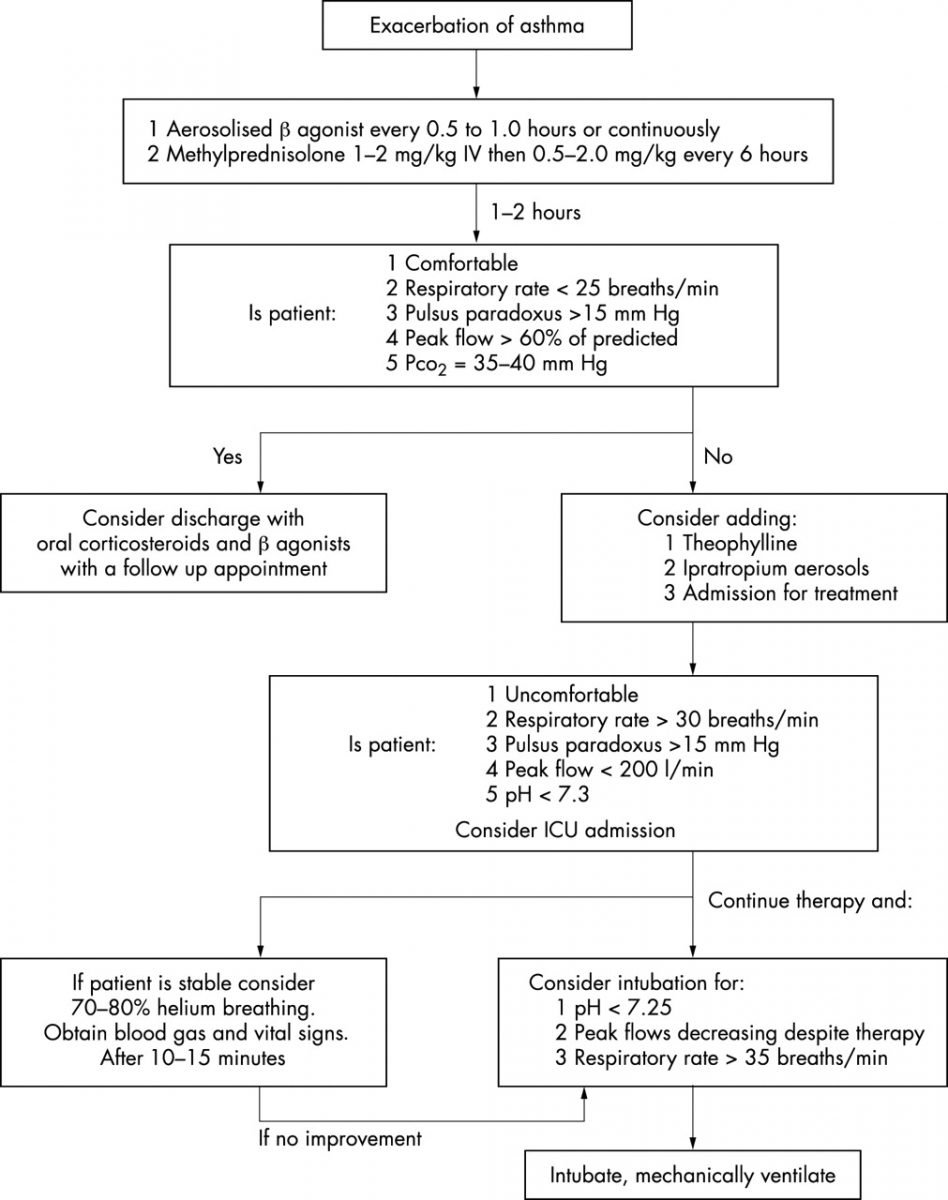
Source: Reuben & Harris (2004)
From the chart above, respiratory therapists can play proactive roles in the diagnosis of the condition of the patient to determine the necessity of conducting other therapeutic interventions for patients with acute asthma before proceeding to the administration of heliox therapy (Therapists play incredible roles in the process of evaluation of the requisite intervention by considering the appropriateness of various alternatives in the context of cost considerations and the condition of the patient prompting the administration of a therapy).
Respiratory therapists also determine patients’ heliox requirements. This helps in the determination of the right volumes of the heliox gas mixture that is necessary for administration to meet the requirements of patients. The chart also evidences that the process of asthma treatment entails decision-making processes based on the condition of patients. Such decisions require human decision-making interfaces. The respiratory therapist can only play this role.
Conclusion
Persons suffering from acute asthma require a breathing aid to minimize WOB, which is caused by increased mechanical load on the respiratory system muscles. While there are different therapeutic interventions to help in the achievement of this goal, the paper focused on the heliox therapy. Use of heliox therapy has been in the medical filed in 1930s.
Although it was first deployed in the treatment of asthma, it has found other applications such as the treatment of COPD (Chronic Obstructive Pulmonary Disease) and bronchiolitis. The therapy involves deployment of helium as the oxygen carrier gas. Compared to air or nitrogen-oxygen gas mixture, helium-oxygen gas mixture in the ratio of 80:20 or 79:21 has low density.
Hence, it results in low resistances of flow in large air passages where the flow resistance is directly related to the density. In such passages, the flow is mainly turbulent. Reduction in resistance of flow results in low WOB. This has an effect of immense relief to patients with breathing difficulties associated with asthma and brokerage of large air passages due to infections such as tumors.
Although heliox therapy has no side effects in patients, the study revealed some technical difficulties associated with it together with looking for cost effective approaches to produce heliox gas mixture. Such approaches are necessary before the therapy can become common and/or a quick alternative in all hospitals across the globe.
Reference List
Allan, P., & Thomas, K., et al. (2009). Feasibility of Noninvasive Ventilation with Helium-Oxygen Gas Flow for Chronic Obstruction Pulmonary Disease during Exercise. Respiratory care, 54(9), 1175-1182.
Brandao, D., & Britto, M. et al. (2011). Heliox and forwards- leaning posture improve the efficacy of Nebulized bronchodilator in acute Asthma: a randomized trial. Respiratory Care, 56(7), 947-952.
Chevrolet, J. (2001). Helium Oxygen Mixtures in the Intensive Care Unit. Critical Care, 5(4), 179-181.
Gupta, V., Grayck, E., & Cheifetz, I. (2004). Heliox administration during high frequency jet ventilation Augments carbon dioxide clearance. Respiratory Care, 49(9), 1038-1044.
Hess, D., & Chatmonqkolchart, S. (2000). Techniques to Avoid Intubation: Noninvasive Positive Pressure Ventilation and Heliox Therapy. Int Anesthesiol Clin, 38(3), 161-187.
Hess, D., Fink, J., Venkataraman, S., Kim, I., Myers, T., & Tano, B. (2006). The History and Physics of Heliox. Respiratory Care, 51(6), 602-612.
Hunt, T., Wiliams, M., Frith, P., & Schembri, D. (2010). Heliox, Dyspnoea and Exercise in COPD. European Respiratory Review, 19(115), 30-39.
Hurford, W., & Cheifetz, I. (2007). Should Heliox Be Used for Mechanically Ventilated Patients? Respiratory Care, 52(5), 582-591.
Hyldegaard, O., Kerem, D., & Melamed, Y. (2011). Effects of Breathing Gas Shifts from Air to Heliox Mixtures on Resolution of Air Bubbles in Lipid and Aqueous Tissues of Recompressed rats. European Journal of Applied Physiology, 111(9), 2183-2193.
Kneyber, M., Heerde, M., Twisk, J., Ploz, F., & Markhors, D. (2009). Heliox reduces respiratory system resistance in respiratory syncytial virus induced respiratory failure. Critical Care 13(3), 1-15.
Myers, T. (2006). Use of Heliox in Children. Respiratory Care, 51 (6), 619-631.
Palange, P., & Valli, G. et al. (2004). Effects of Heliox on Lungs Dynamic Hyperinflation, Dyspnea, and Exercise Endurance Capacity in COPD Patients. Journal of Applied Psychology, 9(7), 1637-1642.
Randsoe, T., Kvist, M., & Hyldegaard, O. (2008). Effect of oxygen and heliox breathing on air bubbles in adipose tissue during 25-kPa altitude exposures. Journal of Applied Physiology, 10(5), 1492-1497.
Reuben, A., & Harris, A. (2004). Heliox for asthma in the emergency department: a review of the literature. Emergency Medicine, 21(1), 131-5.
Venkataraman, S. (2006). Heliox during Mechanical Ventilation. Respiratory Care, 51(6), 632-639.
Yilmaz, S., Daglioglu, K., & Yildizdas, D et al. (2013). The effectiveness of Heliox in acute respiratory distress syndrome. Annals of Thoracic Medicine, 8(1), 46-52.