The Change Model Description
The Johns Hopkins Nursing EBP Model:
- a problem-solving model;
- appropriate to promote the nurse’s decision-making;
- relevant to the nursing practice (Melnyk & Fineout-Overholt, 2011, p. 271).
Includes several steps:
- Practice question:
- Step 1 and 2: Recruit Interprofessional Team and Develop the EBP Question.
- Step 3: Define the Scope of the EBP and determine stakeholders.
- Step 4 and 5: Determine Responsibility of Team Members and Organize team meetings.
- Evidence:
- Step 6 and 7: Conduct Internal/External Search for Evidence and Appraisal.
- Step 8 and 9: Summarize and Synthesize the Evidence.
- Step 10: Recommendations.
- Translation:
- Step 11 and 12: Fit, Feasibility and Appropriateness of Recommendations and Action Plan.
- Step 13 and 14: Secure Support and Resources and Implement Action Plan.
- Step 15 and 16: Evaluation and Reporting Outcomes.
- Step 17 and 18: Identify Next Steps and Disseminate Findings (Dearholt & Dang, 2012).
PICO Question
In nurses working in clinics and hospitals, how does a choice to work an 8-hour shift five days a week compared to working a 12-hour shift three days a week influence the decrease in the nurse’s level of fatigue?
- P– (Patient, population, or problem): Nurses working in clinics and hospitals.
- I– (Intervention): The work in an 8-hour shift five days a week.
- C– (Comparison with other treatment/current practice): The work in a 12-hour shift three days a week.
- O– (Desired outcome): The decreased level of the nurse’s fatigue.
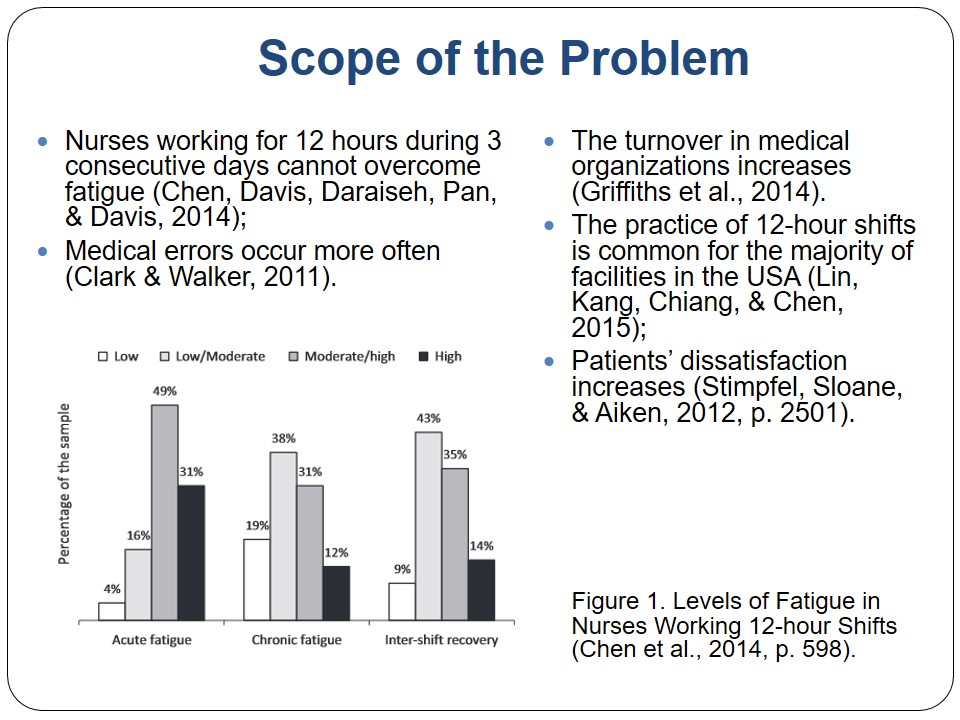
Scope of the Problem
- Nurses working for 12 hours during 3 consecutive days cannot overcome fatigue (Chen, Davis, Daraiseh, Pan, & Davis, 2014);
- Medical errors occur more often (Clark & Walker, 2011).
- The turnover in medical organizations increases (Griffiths et al., 2014).
- The practice of 12-hour shifts is common for the majority of facilities in the USA (Lin, Kang, Chiang, & Chen, 2015);
- Patients’ dissatisfaction increases (Stimpfel, Sloane, & Aiken, 2012, p. 2501).
Team and Stakeholders
- The team requires the participation of:
- the charge nurse (develop a new schedule);
- the financial manager (estimate the costs of the project and budgetary limits);
- 3 registered nurses (skilled in interviewing, conducting surveys, and analyzing data).
- Stakeholders include:
- medical workers;
- patients;
- hospital administrators.
Evidence to Implement Change
- Fatigue:
- Nurses working an 8-hour shift five days per week are less likely to experience fatigue (Sloan, 2006; Trinkoff et al., 2011).
- The level of fatigue in nurses working 12-hour shifts increases with each following shift (Stimpfel et al., 2012).
- Nurses cannot overcome the exhaustion fully during the days off (Chen et al., 2014).
- Patient Satisfaction:
- The adoption of the 12-hour shift leads to the patients’ dissatisfaction (Lin et al., 2015; Stimpfel et al., 2012).
- Patient outcomes decrease significantly when nurses choose 12-hour shifts and the overwork (Chen et al., 2014; Stimpfel et al., 2012).
- Quality of Work:
- The decreased attention caused by exhaustion leads to affecting the quality of work negatively (Clark & Walker, 2011).
- Nurses working short shifts demonstrate higher performance results in contrast to nurses working long shifts (Chen et al., 2014; Stimpfel et al., 2012).
- Longer working hours contribute to the increased mortality in medical organizations due to nurses’ fatigue (Trinkoff et al., 2011).
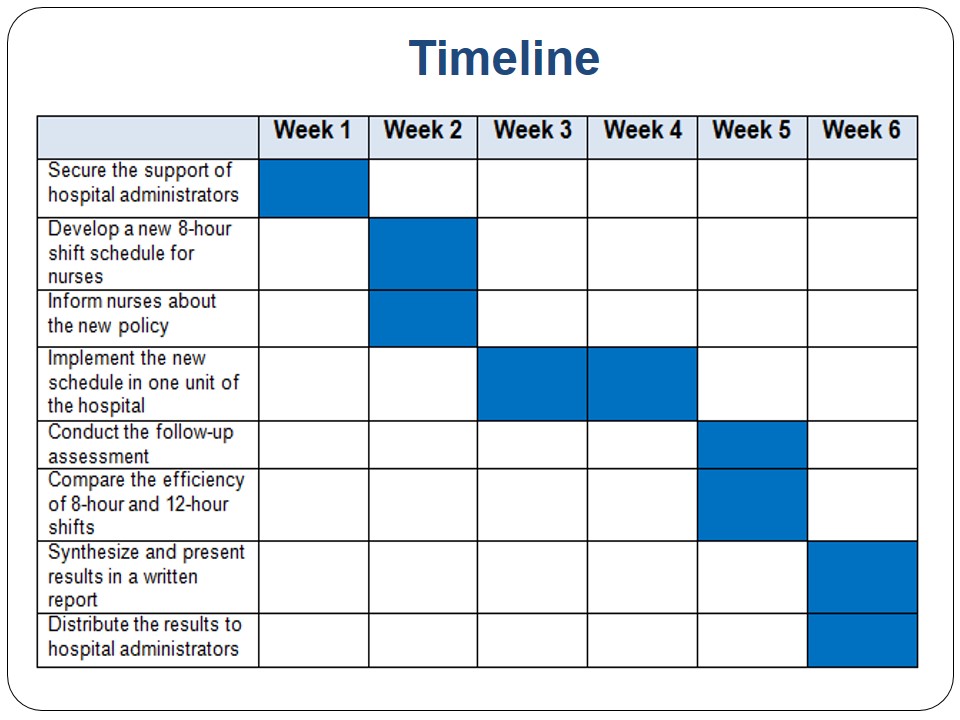
Action Plan
- Secure the support of hospital administrators informing them about the 8-hour shift benefits.
- Develop a new 8-hour shift schedule for nurses.
- Inform nurses about the new policy.
- Implement the new schedule in one unit of the hospital.
- Conduct the follow-up assessment surveying nurses and patients in two units.
- Compare the efficiency of 8-hour and 12-hour shifts and scheduling methods.
- Synthesize and present results in a written report.
- Distribute the results to hospital administrators.
The Nurse’s Role
- The nurse’s role is to:
- contact stakeholders;
- coordinate the work of the project team;
- coordinate the development of the new schedule;
- inform the staff on the policy implementation;
- monitor the action plan activities;
- adjust the activities to the plan;
- address the unexpected challenges;
- coordinate the program implementation process;
- assess the program results;
- analyze and compare the results;
- present the written report on the completed project.
Procedures
- Contact the hospital administrators and develop the cooperation.
- Organize the team for working on the project.
- Conduct scheduled meetings.
- Develop the project plan timeline.
- Analyze strategies to developing nursing schedules in terms of influencing fatigue, quality of work, and patient outcomes.
- Choose the appropriate strategy to integrate the schedule with an 8-hour shift.
- Develop a new 8-hour shift schedule for nurses.
- Approve the project plan and the new schedule.
- Inform nurses about the new policy.
- Implement the new schedule in one unit of the hospital.
- Conduct the survey for nurses working 12-hour and 8-hour shifts.
- Conduct the survey for patients in two units.
- Assess the results regarding fatigue, quality of work, and patient outcomes.
- Compare the efficiency of 8-hour and 12-hour shifts and scheduling methods.
- Synthesize and present results in a written report.
- Inform hospital administrators and nurses on results.
Forms to Be Used
- Maslach Burnout Inventory assess the level of nurses’ fatigue and burnout (Sloan, 2006, p. 21).
- The questionnaire created by the researcher is helpful to determine if patients are satisfied with medical services.
Resources
- The nurse investigator;
- The team;
- Internet resources;
- Assessment tools;
- Analysis tools.
Summary
- Problem:
- The increased level of fatigue in nurses working 12-hour shifts.
- The decreased quality of care.
- The negative effects on the patient satisfaction.
- Purpose:
- To propose the effective scheduling scheme based on the 8-hour shifts for nurses.
- Goal:
- By the end of the project, to demonstrate that the level of fatigue typical for nurses working 12-hour shifts is higher than the level of fatigue typical for nurses working 8-hour shifts leading to the increased quality of work and patient satisfaction.
References
Chen, J., Davis, K., Daraiseh, N., Pan, W., & Davis, L. (2014). Fatigue and recovery in 12-hour dayshift hospital nurses. Journal of Nursing Management,22(5), 593-603.
Clark, A. R., & Walker, H. (2011). Nurse rescheduling with shift preferences and minimal disruption. Journal of Applied Operational Research, 3(3), 148-162.
Dearholt, S., & Dang, D. (2012). Johns Hopkins Nursing Evidence-based Practice: Models and Guidelines. New York, NY: Sigma Theta Tau.
Griffiths, P., Dall’Ora, C., Simon, M., Ball, J., Lindqvist, R., Rafferty, A. M., … & Aiken, L. H. (2014). Nurses’ shift length and overtime working in 12 European countries: The association with perceived quality of care and patient safety. Medical Care, 52(11), 975-981.
Lin, C. C., Kang, J. R., Chiang, D. J., & Chen, C. L. (2015). Nurse scheduling with joint normalized shift and day-off preference satisfaction using a genetic algorithm with immigrant scheme. International Journal of Distributed Sensor Networks, 501(1), 595-419.
Melnyk, B., & Fineout-Overholt, E. (2011). John Hopkins Nursing Evidence-Based Practice Process. New York, NY: Lippincott Williams & Wilkins.
Sloan, G. (2006). Clinical Supervision in Mental Health Nursing. New York, NY: John Wiley & Sons.
Stimpfel, A., Sloane, D., & Aiken, L. (2012). The longer the shifts for hospital nurses, the higher the levels of burnout and patient dissatisfaction. HealthAffairs, 31(11), 2501-2509.
Trinkoff, A., Johantgen, M., Storr, C., Gurses, A., Liang, Y., & Han, K. (2011). Nurses’ work schedule characteristics, nurse staffing, and patient mortality. Nursing Research, 60(1), 1-8.