Coronary syndrome is a complex set of symptoms that appear when the coronary arteries narrow and myocardial circulation is disturbed. The cause of coronary syndrome can be angina pectoris, coronary heart disease, or myocardial infarction. It is manifested by severe chest pain, shortness of breath, dizziness, sudden sweating, etc. In all cases, the patient needs urgent medical attention. The coronary syndrome is not an exact diagnosis but a term that refers to the insufficient blood supply to the myocardium and its accompanying symptoms. It is used when a patient enters the clinic when the exact cause of the disease has not been established.
These patients first need emergency treatment to bring their situation under control, and after that, they have an electrocardiogram in addition to other exams. The next course of therapy will be determined by the findings of these tests as well as the patient’s health history. The coronary syndrome is brought on when the coronary arteries become constricted or obstructed; these are the vessels via which blood enters the myocardium, bringing with it the oxygen and nutrients that it needs to function properly. Atherosclerosis and coronary heart disease are two common conditions that may lead to the development of coronary syndrome. The constriction may result in a spasm of the arteries, the formation of an atherosclerotic plaque, or a clot in the circulation.
The coronary syndrome can be a manifestation of unstable angina or exacerbation of coronary heart disease, which develops when the coronary arteries narrow. It happens due to the deposition of atherosclerotic plaques in them, blockage by a thrombus or spasm, and the lanes narrowing by 50-70% (Chandra and Swamy, 2020). Or, it can be a myocardial infarction, namely, a critical violation of the blood supply to the myocardium, hypoxia, resulting in tissue death and the arteries narrowing by more than 70%. Insufficient blood supply to the myocardium leads to disruption of the heart and the appearance of related symptoms. If the lumen of the vessels is narrowed by more than 70%, myocardial cells gradually die off, and a heart attack develops.
In medicine, the term “acute coronary syndrome” is most often used, and it implies a condition in the development in which the patient needs emergency help. If it is not provided, serious complications can develop up to the cardiac arrest. Once diagnosed, acute coronary syndrome is classified as angina or myocardial infarction. Chronic coronary syndrome develops when the arteries narrow, usually due to atherosclerosis, namely deposits of cholesterol plaques on the walls of blood vessels. In this case, the diagnosis is coronary heart disease or angina pectoris.
The most common cause of coronary syndrome is severe chest pain, which can spread to other parts of the body, especially the left side. Signs of coronary syndrome may involve tightness in the chest, acute chest pain, a burning sensation, and pain spreading to the chin, shoulders, ribs, abdomen, or back (Chandra and Swamy, 2020). It may also include increased heart rate, shortness of breath, cold sweats, dizziness, fainting, nausea, vomiting, extreme fatigue, anxiety, confusion, and increased blood pressure. Besides, it may be characterized by shortness of breath and a feeling of lack of air. In some cases, the coronary syndrome symptoms are mild, the pain may be aching, and nausea and other signs may be absent. For mild angina attacks, these symptoms usually go away after 5 minutes of rest or after taking medications prescribed by the doctor. If symptoms persist, myocardial infarction may be the cause.
Occasionally, narrowing of the coronary arteries and heart attack are almost asymptomatic. There are also atypical manifestations, such as a feeling of suffocation without chest pain, reminiscent of an asthma attack. It also includes mild chest pain and severe pain in the shoulders or other areas of the trunk, and headache with high blood pressure. Moreover, the patient has a violation of the heart rhythm, swelling, difficulty other symptoms, and others. Coronary syndrome is a life-threatening condition, so if even a few symptoms appear, one should immediately call an ambulance.
Before the arrival of an ambulance, the following actions can be taken, namely, putting the patient on one’s back and raising one’s head and torso by 30-40 degrees. If a garment or belt is constricting the chest and making it difficult to breathe, unfasten it and ventilate the room so that the person has more oxygen. It is necessary to give the patient a crushed aspirin tablet or put it under the tongue if there are no contraindications to the drug. In addition, the patient is required to be provided with a nitroglycerin tablet under the tongue, and if the pain does not go away, repeat it after 5-10 minutes.
If the patient has lost consciousness, it is necessary to check the pulse and, in its absence, perform a heart massage and artificial respiration. If the pain has become less after taking nitroglycerin, one should not refuse the arrival of an ambulance and hospitalization. The drug reduces the symptoms but does not eliminate its cause. Therefore, it is vital to undergo early diagnosis and treatment. However, no more than three tablets can be given since nitroglycerin can reduce pressure to critical levels.
Patients are advised to eat a balanced diet and lead an active lifestyle for prevention. To reduce the likelihood of developing coronary syndrome and other cardiovascular diseases, one needs to reduce the influence of risk factors. These include overweight, malnutrition, low physical activity, high blood cholesterol, uncompensated diabetes mellitus, smoking, drinking alcohol, etc. After 40 years or in the presence of risk factors, one should visit a cardiologist annually and do an ECG, as well as, in case of cardiovascular diseases, undergo the necessary treatment in a timely manner. In addition, it is essential to maintain average body weight and stop. smoking, eating alcohol, and other bad habits.
A patient with acute coronary syndrome must be hospitalized. First, intensive therapy is performed, namely stabilization of the condition, relief of pain, and elimination of other symptoms. After that, a diagnosis is made and based on its results, treatment is selected. In most cases, long-term drug therapy is prescribed, and recommendations for lifestyle correction are given. Under atherosclerosis and coronary heart disease, drugs are used to lower cholesterol levels, expand and strengthen blood vessels, reduce blood clotting, and others. In some cases, complete blockage of the coronary arteries or treatment failure may require surgery. With a heart attack, drug treatment is also first used, aimed at restoring blood circulation and reducing the risk of complications. With an extensive heart attack or the presence of concomitant pathologies, an operation is likely to be performed – coronary stenting, bypass surgery, or the installation of a pacemaker.
The patient had hyperlipidemia, a state in which there is a surplus of certain fats in the blood, which is fraught with the growth of vascular complications and atherosclerosis. Finally, hyperlipidemia may cause ischemia, thrombosis, or even a heart attack (Chandra and Swamy, 2020). It is a good idea to start thinking about getting the cholesterol checked once a person reaches the age of 40, and in certain cases, one should start monitoring lipids even sooner than that (Chandra and Swamy, 2020). The problem of hyperlipidemia is relevant, and often it appears at a young age. When a patient’s atherosclerotic plaque ruptures inside a vessel, a protective mechanism is activated, and a blood clot begins to form inside the vessel. Ultimately, this thrombus can either completely or partially fill the vessel’s lumen. If this situation occurs in the vessel of the heart, then it can lead to a heart attack, and if it happens in the vessel of the brain to a stroke.
Further, the patient exhibited endothelial dysfunction, a systemic pathological condition. It primarily occurred due to decreased eNOS activity and NO bioavailability. In addition, it is manifested by an imbalance of paracrine factors secreted by the endothelium. It can lead to vasoconstriction, a pathological condition of blood vessels characterized by the narrowing of their lumen. In most cases, the cause of the development of the disease is atherosclerotic damage to the arteries, when cholesterol plaques are deposited on their walls. It may provoke hypertension, which is a persistent increase in blood pressure. Excitation of sympathetic nerves causes vasodilation of the brain, skin, and peripheral vessels as a consequence.
Bacteria belonging to the genus Streptococcus are found naturally inside the human body. More than 15 bacterial subgroups have been identified, with alpha, beta, and gamma being the vast majority. Streptococci with a healthy alpha and gamma count are non-pathogenic and found in every person’s natural microbiota, including the Gastrointestinal system, mouth, throat, and lungs. Diseases caused by beta streptococci are common and serious. Infection with streptococcus bacteria may lead to a wide variety of illnesses, including but not limited to pneumonia, glomerulonephritis, vasculitis, tonsillitis, rheumatism, erysipelas, scarlet fever, and many more (Hand et al., 2020). Affected areas include the upper chest, upper arms, and face.
The pathogenic bacteria may spread in three ways: via the air, through direct contact, and by the dissemination of infected saliva and mucus through sneezing, shouting, and coughing. The contact-household transmission mode requires close proximity to an infected person as well as direct interaction with the infected person (Hand et al., 2020). Diseases may be spread via inadvertent contact with common household goods, even in the absence of any outward symptoms. Streptococcus may spread quickly via the air and is most likely to infect a group of youngsters who are together, such as in a classroom setting (Hand et al., 2020). Most cases of streptococcal infection in children occur in the late fall and winter, although these infections may occur at any time of year since kids do not always practice good hand hygiene.
Streptococcus has the potential to invade cells and tissues, making it a common cause of infection in infants. The illness may be transmitted via the amniotic fluid at the moment of delivery (Hand et al., 2020). Symptoms of the illness, which may include pneumonia, sepsis, and meningitis, appear during the first few hours of a newborn’s existence (Hand et al., 2020). More than half of patients who experience this progression succumb to their illness (Chandra & Swamy, 2020). Streptococcus pneumonia is a common consequence of several infectious diseases in children ages 2-8, most often whooping cough, influenza, measles, and chicken pox (Althouse et al., 2017). Children with impaired immune systems, such as those caused by severe hypothermia, are also at risk of contracting this illness.
A streptococcal infection can cause a wide range of symptoms in the context of medically relevant diseases. This kind of pathogenic bacteria can cause a wide range of illnesses, so it is hard to say. Throat soreness, a high temperature, and a buildup of pus-filled plaques on the tonsils are symptoms of a variety of respiratory disorders. In addition, the patient may have lymph node hypertrophy. Inflammatory processes on the skin, itchiness, redness, the formation of vesicles and plaques on the skin, fever, chills, and weakness are all common symptoms of a streptococcal skin infection. The majority of people with hemolytic streptococcus-related genitourinary tract infections do not have any symptoms at all. Nevertheless, genitourinary discomfort, itching, and discharge are all symptoms that have been associated with a number of disorders.
When an infection enters the body, the immune system is activated. The cells of innate immunity capable of phagocytosis, namely the process of absorption and digestion of antigens, are the first to turn on. Thanks to receptors on their surface, cells recognize someone else’s and bind antigens. Receptors recognize common microbial antigens common to most microorganisms. These are lipopolysaccharides of gram-negative bacteria, peptidoglycans of gram-positive bacteria, viral RNA, and other structures. These receptors bind not only free antigens but are also located on the surface of infected cells of the body. In an ideal immune response, microorganisms, having bound antigens to the receptors of phagocytic cells, are quickly destroyed, but it happens rarely.
Some immune cells immediately die themselves or lose their ability to phagocytosis. To activate the acquired immune response, it is necessary that phagocytic cells, having digested antigens, present them on their surface for recognition by T-lymphocytes. Lymphocytes and some molecular components enhance phagocytosis and support phagocytic cells so that they have time to present antigens associated with specific receptors. Through them, T-lymphocytes recognize antigens and transmit information to B-lymphocytes for the formation of antibodies, so a humoral immune response is formed. Usually directed at toxins, bacteria, and fungi, some T-lymphocytes launch killer cells if intracellular pathogens need to be destroyed. It includes most viruses and damaged, infected, or tumor cells, forming a cellular immune response.
Finally, the patient’s immune system releases particular substances, including those which protect the body from the infection. Cytokines are activated cells of the immune system, providing intercellular interactions. Cytokines include interferons (IFN), interleukins (IL), chemokines, tumor necrosis factors (TNF), colony-stimulating factors (CSF), and growth factors. Cytokines act according to the relay principle; the effect of a cytokine on a cell causes the formation of other cytokines by. Pyrogens are substances that can cause an increase in body temperature. The pyrogenic reaction can cause substances of different natures and origins. Pyrogens include gram-negative bacteria and their toxins, gram-positive bacteria and toxins, viruses and waste products, and steroids.
References
Althouse, B. M., Hammitt, L. L., Grant, L., Wagner, B. G., Reid, R., Larzelere-Hinton, F., Weatherholtz, R., Klugman, K. P., Rodgers, G. L., O’brien, K. L., & Hu, H. (2017). Identifying transmission routes of streptococcus pneumoniae and sources of acquisitions in high transmission communities. Epidemiology and Infection, 145(13), 2750–2758. Web.
Asghari, E., Gholizadeh, L., Kazami, L., Taban Sadeghi, M., Separham, A., & Khezerloy-aghdam, N. (2022). Symptom recognition and treatment-seeking behaviors in women experiencing acute coronary syndrome for the first time: A qualitative study. BMC Cardiovascular Disorders, 22(1), 508. Web.
Bhatt, D. L., Lopes, R. D., & Harrington, R. A. (2022). Diagnosis and treatment of acute coronary syndromes. JAMA, 327(7), 662. Web.
Buja, L. M. (2022). Pathobiology of myocardial ischemia and reperfusion injury. Cardiology in Review, Publish Ahead of Print. Web.
Chandra, K. S., & Swamy, A. J. (2020). Acute coronary syndromes. CRC Press.
Gaubert, M., Marlinge, M., Alessandrini, M., Laine, M., Bonello, L., Fromonot, J., Cautela, J., Thuny, F., Barraud, J., Mottola, G., Rossi, P., Fenouillet, E., Ruf, J., Guieu, R., & Paganelli, F. (2018). Uric acid levels are associated with endothelial dysfunction and severity of coronary atherosclerosis during a first episode of acute coronary syndrome. Purinergic Signalling, 14(2), 191–199. Web.
Hand, R. M., Snelling, T. L., & Carapetis, J. R. (2020). Group A streptococcus. Hunter’s Tropical Medicine and Emerging Infectious Diseases, 429–438. Web.
Libby, P., Nahrendorf, M., & Swirski, F. K. (2016). Leukocytes link local and systemic inflammation in ischemic cardiovascular disease. Journal of the American College of Cardiology, 67(9), 1091–1103. Web.
Palur Ramakrishnan, A. V., Varghese, T. P., Vanapalli, S., Nair, N. K., & Mingate, M. D. (2016). Platelet activating factor: A potential biomarker in acute coronary syndrome?Cardiovascular Therapeutics, 35(1), 64–70. Web.
Swieringa, F., Spronk, H. M. H., Heemskerk, J. W. M., & van der Meijden, P. E. J. (2018). Integrating platelet and coagulation activation in Fibrin Clot Formation. Research and Practice in Thrombosis and Haemostasis, 2(3), 450–460. Web.
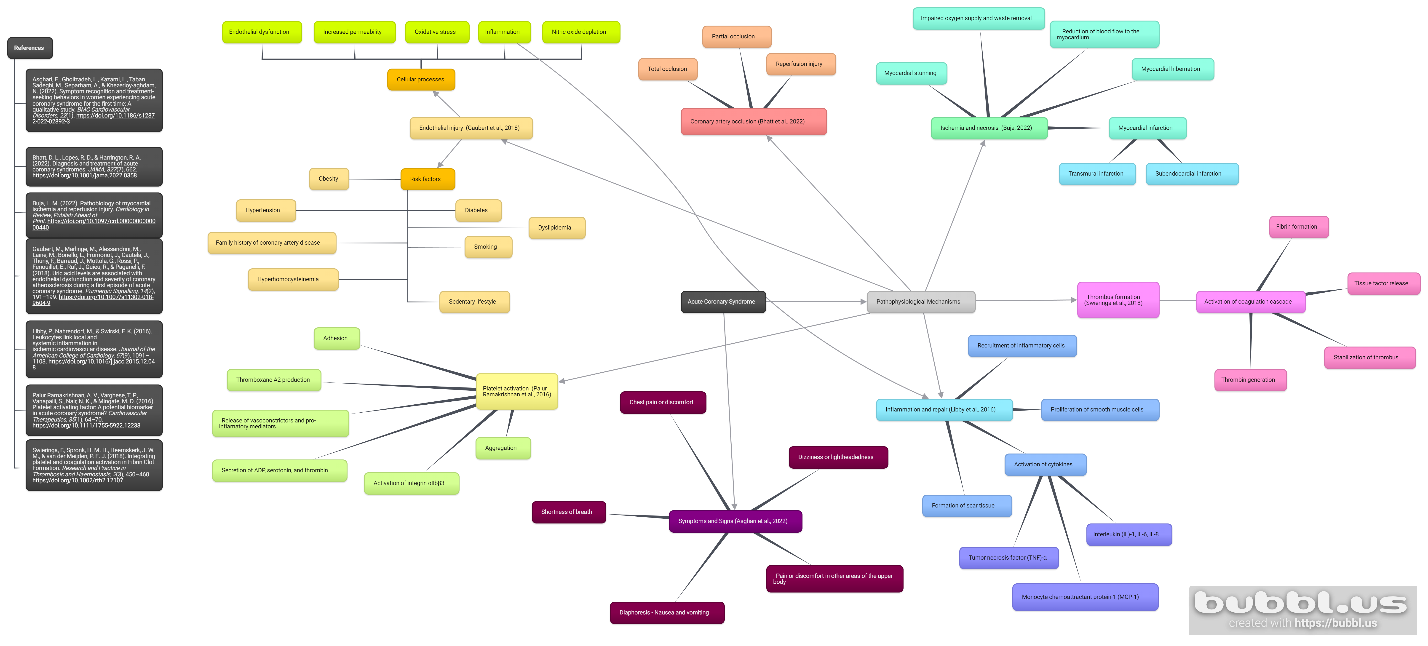
The Concept Map