Introduction
Workflow, loosely considered, is a series of assignments chronologically clustered into various processes and personnel and other resources required for those roles identified, which are vital to accomplish specific objectives. In hospitals, for instance, a workflow normally reflects various processes needed to realize care delivery goals. In this case, healthcare providers and other resources must be present to perform these processes and facilitate interactions for desired outcomes. The primary role of workflow analysis in healthcare settings is to enhance efficiency. The purpose of this research paper is to assess workflow analysis for advance directives. It presents a workflow issues analysis, diagram, method of analysis, evidence-based recommendations and conclusion.
Workflow Issues Analysis
Health information technology, if executed well, can enhance efficiency and organizational workflow. Documented advance directives (ADs) can significantly curtail notable discrepancies between care delivery preferred and the actual care delivered to a patient. It is estimated that about 43% of senior citizens in the US would require critical healthcare decision related to near the end-of-life (Gabler et al., 2016). However, about 70% of these patients cannot take part in decision-making processes and, therefore, rely on others to make decisions for them (Gabler et al., 2016).ADs, which generally consist of the patient’s living will and the power of attorney designation – useful for enhancing the quality of advance care planning for patients.
Studies have suggested that both academic medical setting and inpatient setting are not ideal for discussing end-of-life issues with patients (Allen et al., 2015; Gabler et al., 2016). On this note, outpatient setting offers an ideal opportunity for ADs but with some limitations (Gabler et al., 2016). In outpatient settings, poor outcomes are noted in about 5% to 30% cases based on the definition adopted, the population, and the clinical setting. Specifically, physicians have reported challenges associated with inadequate time, poor accessibility of AD in the medical record, and a lack of prior discussion about the end-of-life care with the patient and family (Hayek et al., 2014).
In addition, it is also observed that in healthcare settings, there are instances of creating and collecting redundant information about patients. Consequently, nurses, physicians, and other care providers spend much time in attempts to reconcile information obtained from disparate sources. Health IT solutions offer workflow integration opportunities across different departments to curtail redundancy. Nevertheless, if workflow processes are not accounted for and IT platform is not carefully executed, then no hospitals can truly realized the intended outcomes. Effective use of IT in healthcare settings can only be realized through transformed care delivery. In addition, interactions that are more complex have also been noted among healthcare providers, which could hinder documentation.
It is noteworthy that the introduction of health information technology driven by informatics and the mass adoption of electronic health medical records (EMRs) have introduced innovative approaches for streamlining care delivery, documentation and care improvement as components of quality improvement initiatives.
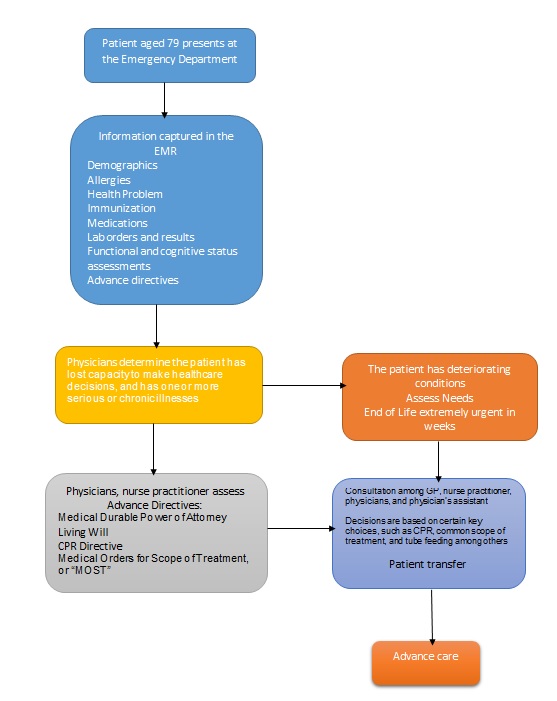
Diagram
Method of Analysis
An interview was used to track the flow of information across various units of care provision. The interviewee acknowledged that accurate information was required to deliver quality care to patients. Hence, too much, missing, or too little information was ineffective. The aim of the information collection was to ensure that care providers did not miss vital quality and safety issues. It was emphasized that minor details were critical for patient populations whose recovery and progress were generally gradual and challenging. Minor delays, for instance, could lead to missed therapies, medications, and treatments that could have adverse outcomes.
The interviewee identified demographic, allergies, vital signs, problem lists, medications, advance directives, functional and cognitive status, immunization, and laboratory request and result data as extremely important in the workflow to ensure uninterrupted care.
The major advantage of the interview was that the flow of information was presented from a practitioner’s point of view. Thus, intricate, task-specific works, communications, data capture and other processes were presented in simple terms. These tasks and processes are difficult to understand, especially for individuals not familiar with data capture and transfer in healthcare settings.
From this interview on the flow of information, it was difficult to assess the accuracy of data captured and entered into the EMR, interactions with patients, and information retrieval, as well as insights obtained after analysis. In addition, it was also not clear if all data were captured at the right points and put into the workflow. The interview could have possibly suffered from interviewee’s bias, especially in collaboration, communications, information sharing and transfer among others.
To this end, it is suggested that a combination of structured survey, observation, and review of EMRs on ADs should be conducted to obtain reliable outcomes on information flow.
Evidenced-based Recommendations
One common concept supported by literature is collaboration. The relevance of interdisciplinary team involvement in all areas of workflow analysis remains vital for nurses and physicians who wish to realize goals of their organizations. As previously noted, workflow analysis experiences the greater challenge of capturing all data into the workflow. Collaboration presents a better opportunity to overcome such a challenge. Nurse informatics, IT departments, physicians, and nurses often work in isolation. It is imperative for nurse informatics, IT, and physicians to work collaboratively to ensure that the IT platform can enhance system implementation and meet needs of end users, including workflow data retrieval (Jones, Sabin, & Torma, 2016). Consequently, all stakeholders in the workflow analysis can benefit through enhanced efficiency and effectiveness noted in design workflow, processes, and deployment.
It is also imperative to recognize that EMRs still require nursing informatics solutions to achieve the desired care outcomes. That is, the IT department should engage other stakeholders for insights and solutions to their challenges to compliment EMR tasks. On this note, inter-professional collaboration is vital for workflow analysis (Christopherson, Troseth, & Clingerman, 2015).
Further, it has been observed that a good workflow design ultimately improves healthcare delivery. Interactions that are more complex are often observed in the workflow analysis. For instance, physicians are expected to perform most tasks before nurses can gain access to conduct their roles. Medication, for example, requires physicians’ inputs first. In such cases, nurses cannot immediately perform their roles. Therefore, healthcare IT may fail to support some roles and ultimately lessen the intended outcomes. In addition, poor coordination, nurse performing other roles during busy periods and handoffs approaches lead to degradation of information.
Further, complexity in the workflow analysis could compel some nurses to adopt informal practices, lack of sufficient documentation, and failure to provide all data to other nurses during shifts. Once collaboration has been attained, it is necessary for nurses to adopt formal information transfer tools and practices to support workflow activities (Singh & Sittig, 2015). This approach can also assist them to eliminate challenges associated with work interruptions, which ultimately affect documentation and information transfer.
Nurses and physicians should appreciate the relevance of technology to improve major constructs of nursing roles (Whittenburg, 2010). Nursing workflow analysis should present the evolution of practices and workflow concepts based on management and health IT perspectives adopted in electronic health records and EMRs. According to Whittenburg (2010), effective comprehension of workflow models in the health information perspectives could enhance the model of nursing workflow essential for the implementation of the HER systems.
Interaction with patients is also extremely important. Nurse and physician training and workflow alterations improve patient-resident engagement based on end-of-life issues. Interaction helps to overcome one major challenge related to engaging patients. Educating nurses and physicians presents an opportunity for patients and care providers to broach the end-of-life subject. In fact, patients can understand and appreciate the relevance of the Patient Self-Determination Act of 1990, which has continued to receive enhanced attention as care providers strive to ensure that patients’ end-of-life requests are captured and stored in the workflow analysis (Hayek et al., 2014).
While such efforts have improved, they still do not reflect accurate needs of patients because of poor communication between care providers and patients. It is imperative to recognize that patients may wish to engage their care providers on such issues, but they do not understand how to initiate such conversations. Hence, many nurses may not address them adequately, leading to poor or wrong data captured (Allen et al., 2015). In addition, patients may also want to address these issues, but a busy clinical setting does not provide the right environment. Thus, nurses and physicians should ensure that such discussions take place because patients introduced to outpatient hospice discussions, for instance, had a shorter length of stay and increased utilization of palliative care resources (Doll et al., 2013).
Conclusion
Workflow analysis reflects a set of tasks that nurses should observe when executing advance directives as required under the Patient Self-Determination Act. It is intended to improve efficiency of care and outcomes. Nevertheless, advance directives could be difficult to execute if critical information is missing or not provided in the workflow. Moreover, once captured in the system, end users are most likely to encounter some challenges related to retrieval, analysis, and use. It is recommended that enhanced collaboration and communication among care providers, patient discussions, and inter-professional engagements can address some of these obstacles. Further, nurse education on end-of-life issues can help in broaching the subject and obtaining the necessary information for workflow analysis from patients.
References
Allen, S. L., Davis, K. S., Rousseau, P. C., Iverson, P. J., Mauldin, P. D., & Moran, W. P. (2015). Advanced care directives: overcoming the obstacles. Journal of Graduate Medical Education, 7(1), 91–94. Web.
Christopherson, T. A., Troseth, M. R., & Clingerman, E. M. (2015). Informatics-enabled interprofessional education and collaborative practice: A framework-driven approach.Journal of Interprofessional Education & Practice, 1(1), 10–15. Web.
Doll, K. M., Stine, J. E., Moore, D. T., Bae-Jump, V., Brewster, W. R., Soper, J. T.,… Kim, K. (2013). Outpatient end of life discussions shorten hospital admissions in gynecologic oncology patients. Gynecologic Oncology, 130(1), 152-5. Web.
Gabler, N. B., Cooney, E., Small, D. S., Troxel, A. B., Arnold, R. M., White, D. B.,… Volpp, K. G. (2016). Default options in advance directives: study protocol for a randomised clinical trial. BMJ Open, 6(6), e010628. Web.
Hayek, S., Nieva, R., Corrigan, F., Zhou, A., Mudaliar, U., Mays, D.,… Ilksoy, N. (2014). End-of-life care planning: improving documentation of advance directives in the outpatient clinic using electronic medical records. Journal of Palliative Medicine, 17(12), 1348-1352. Web.
Jones, F. M., Sabin, T. L., & Torma, L. M. (2016). Improving the advance directive request and retrieval process in critical access hospitals.Journal of Nursing Care Quality, 31(3), 275-281. Web.
Singh, H., & Sittig, D. F. (2015). Measuring and improving patient safety through health information technology: The Health IT Safety Framework. BMJ Quality & Safety, 1-7. Web.
Whittenburg, L. (2010). Workflow viewpoints: Analysis of nursing workflow documentation in the electronic health record. Journal of Healthcare Information Management, 24(3), 71-5.