Introduction
Ankylosing spondylitis (AS) is a chronic disease that damages axial joints adjacent to the midline in the spinal cord and those in the pelvis sacroiliac (Springhouse, 2006). The condition may lead to gradual fusion of the spine thereby damaging its integrity. Ankylosing spondylitis starts when the connective tissues (ligaments and tendons) get slotted into the bones through an inflammation process leading to spinal stiffness and irritation of the marginal joints (Springhouse, 2006). In addition, AS may cause irritation of the iris, bowel, and aorta. Moreover, it is associated with amyloidosis and fibrosis as well as various neurological disorders like spinal narrowing and dislocation of cervical vertebras one and two.
Epidemiological studies reveal that the disease is more regular in men than in women (Khan, 2009). Precisely, three males suffer from the condition per every one female. High incidences of the disease are recorded in men aged between fifteen to thirty years (Springhouse, 2006). However, there are concerns that the majority of females suffering from the disease are unrecognized as they express gentle symptoms.
Moreover, the disease can affect any individual aged between ten to forty years, and its overall prevalence is approximated at 1.4% and below with 0.13% of United States citizens being affected (Springhouse, 2006). Between 2002 and 2003, 0.013% of all hospital cases in the United Kingdom were AS conditions and ninety-six percent of them required hospital admission (Springhouse, 2006). Generally, it is approximated that five percent of AS disease cases arise during childhood with boys being at high risk when compared to girls.
Genetics seems to play a role since over ninety percent of patients suffering from the disease have relatives whoever experienced the same condition (Michael, John & Heijde, 2006). Furthermore, the majority of individuals possessing the Human Leukocyte Antigen B27 gene are attacked by AS. Besides, the disease is highly prevalent among Native Americans as compared to black Americans (Khan, 2009).
The cost of managing ankylosing spondylitis is high due to expensive chemotherapies, physiotherapies, and diagnostic tests (Springhouse, 2006). Ankylosing spondylitis can cause death although individuals suffering from it may have a normal lifespan. In the year 2003, 36 deaths were recorded in the US while two deaths occurred in the UK (Michael, John & Heijde, 2006). Thus, the disease is of great importance to human existence.
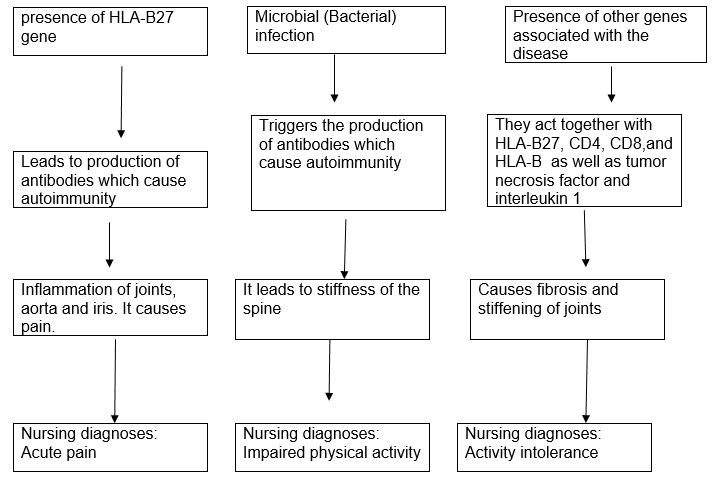
The main objective of this paper is to provide a detailed study of AS conditions so that medical trainees may understand them better. This goal is attained through explaining the disease process and thereafter, providing a typical case study on how to handle Ankylosing spondylitis patients. In addition, the paper provides a flow chart diagram for the disease process and nursing care plans relevant to AS disease.
Disease Process
Etiology
Various scholars including Springhouse and Khan acknowledge that the actual cause of the disease is not well known. However, they agree that genetic factors play an important role in the emergence of AS condition. Virtually all individuals (95%) suffering from AS disease have a genetic marker known as Human Leukocyte Antigen B27 (HLA-B27) produced by specific genes (Khan, 2009). Researchers believe that in addition to HLA-B27 markers, other genes and environmental factors like microbial (viral and bacterial) infections are required for the disease onset (Michael, John & Heijde, 2006).
Bacteria involved in this case are found in intestinal tracts and they include Shigella, Salmonella, and Klebsiella groups among others. Other genes involved in the development of this condition are the interleukin 23 receptor and the type 1 tumor necrosis factor receptor shedding aminopeptidase regulator” (ARTS-1) gene (Michael, John & Heijde, 2006). In total, around five to six genes are thought to be involved in the disease process.
It is supposed that these genes work hand in hand with B27 to comprise the integrity of the immune system (Springhouse, 2006). Various authors say that the condition starts when the body defense mechanisms attack the outer membrane of the ileum and permit bacteria to reach the blood vessel where they are carried to the joints. The microbes activate the immune system and lead to the development of an irreversible autoimmune condition.
Risk factors
One of the greatest risk factors for Ankylosing spondylitis disease is the possession of the HLA-B27 gene. Studies have shown that a great number of individuals (over 90%) who have HLA-B27 suffer from this disease (Springhouse, 2006). However, not all people having this gene get ill; it only increases the possibility of getting sick. Genes are inheritable and therefore individuals with relatives having a history of ankylosing spondylitis have a great chance of contracting the disease.
In addition, an individual’s gender may act as a risk factor (Michael, John & Heijde, 2006). Studies have shown that men are more prone to AS condition than women and that its symptoms are more severe in males than in females. Besides, the disease is more prevalent in young people aged between fifteen tofortyy years and thus, an individual’s age may act as a disease predisposing factor (Springhouse, 2006). MMoreover research has revealed that individuals belonging to some races are more prone to AS than others. The disease seems to affect white Americans more than black Americans (Khan, 2009).
Similarly, the condition is very frequent among people from China than with Japanese citizens. Also, earlier cases of arthritis (colitic and reactive arthritis) enhance chances of suffering from Ankylosing spondylitis. To some extent, this is attributed to genetic factors. Finally, it is argued that people with constant stress as well as gastrointestinal infections are at a greater risk of contacting the disease (Bos & Blobel, 2007).
Pathophysiology
The pathophysiology of this disease is still not clear (Springhouse, 2006). Ankylosing spondylitis is disease condition that can attack every part of human body. It is thought to start from the inflammation of the membranes (in the intestines) thereby allowing the bacteria to reach the blood vessels. Such bacterial cells may activate the immune system to produce antibodies which are intended to protect the body from invaders (Khan, 2009).
Nevertheless, the intestinal bacterial cells have HLA-B27 receptors which are also present on cells of ankylosing spondylitis susceptible individuals. The relationship between Ankylosing spondylitis and HLA-B27 require participation of CD8 T cells which act together with HLA-B (Michael, John & Heijde, 2006). Furthermore, it is supposed that CD4 cells are involved since HLA-B27 can abnormally bind with them in conjunction with human T cells.
There are opinions that self antigens as well as reactive arthritis are involved in the disease process. As such, the immune system is tricked to attack body cells and cause an autoimmune disease which leads to inflammation of the joints. The condition may spread to all body parts with time. However, the specific antibodies involved in this case have not been identified yet. In addition, tumor necrosis factor as well as interleukin 1 is thought to play some part in disease development (Michael, John & Heijde, 2006).
Clinical manifestations
The symptoms of the disease are at first manifested by intermittent pain on then lower side of the spinal chord (Springhouse, 2006). Backaches and stiffness are very common when a person is resting. They are more prominent early in the morning and during sleep hours. However, an individual gets relieved during the day due to high levels of activity. In the initial stages, aching is felt at sacroiliac joints and spreads to other parts of the spinal chord afterwards (Springhouse, 2006). In addition, the disease limits the movement of the spine and the chest as well. Additional clinical manifestations may include exhaustion, irritation of the eye and some aching in the heels. Other symptoms include joint swelling, slight raise in body temperature and loss of body strength (Khan, 2009).
Diagnosis
The first step involves accessing the patient’s family and medical history to ascertain any cases related to the disease (Springhouse, 2006). This is followed by assessing the patient’s neck movement to record the degree of pain while moving. The diagnostic laboratory test for ankylosing spondylitis may include C-reactive protein test, commonly known as CRP, Erythrocyte Sedimentation Rate (ESR) test and the Plasma Viscousity (PV) test (Springhouse, 2006). Other blood tests may be carried out to examine the presence of HLA-B27. Radiography and X-ray tests may also be carried out although they are not very effective during the early stages of disease development (Bos & Blobel, 2007).
Treatment
There is no drug that can entirely eliminate ankylosing spondylitis (Springhouse, 2006). However, chemotherapy, physical treatment and surgery can help to reduce symptoms and ensure uninterrupted movement of the spinal chord. Physical treatment involves maintenance of a good body posture and doing some exercises. Chemotherapy involves the use of pain killing drugs as well as those which prevent irritation. Surgery is needed only when joints are heavily damaged and there is a need to straighten them (Michael, John & Heijde, 2006).
Complications
A few individuals may have spinal fusion and it can lead to serious kyphosis and hampered movement of the spinal chord and the cervix (Michael, John & Heijde, 2006). The spine in this condition is very prone to breakages even after a slight shock. In addition, serious arthropathy may be witnessed in shoulder and hip joints. Moreover, AS may lead to frequent uveitis, amyloidosis and pulmonary as well as cardiovascular complications (Khan, 2009).
Case study
This is a real case involving a juvenile Ankylosing spondylitis patient which I cared for. However, some additional arguments have been added so as to clearly enlighten on the issue. The case involved a fifteen years old schoolboy who had regularly suffered from enthesitis and arthritis for a period of six years. The condition had persisted despite the use of chemotherapies like methotrexate and sulfasalazine. In addition, the patient had typical symptoms of AS and complained of pain in the spinal chord and sacroiliac joints. One of the boy’s parents suffered from psoriasis.
Assessment
The boy was seen to have typical symptoms of AS. The patient’s medical history indicated that disease symptoms started at the age of nine and it was characterized by knee and tarsus oligoarthritis. Three years later, the boy suffered from polyarthritis of the tarsi, hand joints, knees and the hips. Anti-inflammatory drugs like prednisone and diclofenac failed to control the condition. Moreover, the patient had severe joint pain in the vertebral column, chest and lumbar region. Further, the boy complained of pain in the plantar fascia and in the knees as well as in the ankles. It was reported that the pain and spinal stiffness was more severe at night than during the day.
Complications
Physical tests indicated that the patient had fourteen active joints. These included the knees, left metacarpophalangeals one, two and three, right and left proximal interphalangeal one and two as well as left wrist and right metatarsophalangeals two and three (Springhouse, 2006). In addition, the hips, tarsi and sacroiliac joints were affected. Furthermore, physical tests revealed that the patient had eight swollen joints and they included cervical spine two, three, four and seven, Achilles tendon, lumbar and thoracic spines one as well as plantar fascia. All the affected joints exhibited stiffness. Diagnostic results shown that lumbar anterior flexion was three centimeters instead of five and that chest expansion had increases to 5cm instead of 2.5cm (Springhouse, 2006).
Diagnostic tests
The boy’s recorded statistical rating gauge was 7.5 for AS condition and eight for pain using a scale of 0-10same. Further, child health assessment questionnaire was scored at 2.7 using a 0-3 scale while that of functional indexes was 7 using a scale of 0-10 (Michael, John & Heijde, 2006). The laboratory test results for ESR were 64mm/h and those of CRP were 42mg/l. Besides, the boy carried HLA-B27 gene. Finally, the patient was tested for Tuberculosis (TB).
Referrals
The nurse and the hematologist consulted with the patient and agreed to take a radiography test. It was shown that the boy had a rank three bilateral sacroilitis. The tarsus had some osteopenia and a minor space decrease. It should be noted that these tests were carried out as per the modern New York criterion for Ankylosing spondylitis.
Treatment
Previously, proper doses of anti-inflammatory drugs (methotrexate and sulfasalazine) had failed to work. The patient underwent chest X-ray in addition to TB test and he was given an intravenous injection of infliximab 5mg/kg. Then, the boy was put under the same dosage of anti-inflammatory drugs in the second and sixth week of injection and then after every eighth week. After two weeks of receiving the injection, the number of infected joints halved and disease symptoms diminished. Finally, both C-reactive protein and ESR levels normalized.
Nursing care plan for Ankylosing spondylitis patients
The following nursing care plan (tables 1-3) is appropriate for ensuring proper management of the AS condition. This plan was developed after deliberating on and assessing the patient’s condition. In addition, the patient’s views were put into consideration so as to offer better care.
Table 1: Nursing care plan 1.
Table 2: Nursing Care Plan 2.
Table 3: Nursing Care plan 3.
Flow chart diagram
The flow chart diagram below shows the relationship between the causes of AS condition and how each factor leads to pathophysiologic change, clinical manifestations and the nursing diagnoses.
Conclusion
It is believed that the occurrence of ankylosing spondylitis is influenced by the presence of HLA-B27 gene as well as favorable environmental factors and other genes as well. As indicated throughout the paper, this disease is not fully studied. More research needs to be conducted in order to establish ‘other genes’ involved. Research will also help to clearly understand the pathophysiology of the disease hence improved health care.
References
Ackley, B., J., & Ladwig, G., B. (2008). Nursing diagnosis handbook: An evidence- based guide to planning care (8th Ed.). St Louis: Mosby Elsevier.
Bos, L., & Blobel, B. (2007). Medical and Care Compunetics 4.USA:IOS Press.
Doenges, M., Moorhouse, M., & Murr, A. (2010). Nursing Care Plans: Guidelines for Individualizing Client Car across the Life Span. Philadelphia: F. A. Davis Company.
Khan, M., A. (2009). Ankylosing Spondylitis (Oxford American Respiratory Library). (1st Ed.). USA: Oxford University Press.
Michael, H., John, W., & Heijde, R. (2006). Ankylosing spondylitis and the spondyloarthropathies. United States of America: Elsevier Health Sciences.
Springhouse. (2006). Professional Guide to Signs & Symptoms. (5th Ed.). United States: Lippincott Williams & Wilkins.