Introduction
Historically, the issue of substance use addiction has been associated with younger adults rather than older population. This assumption applies to all types of substance abuse, including tobacco, alcohol, and various types of drugs. Statistically, older generations do not demonstrate high rates of substance abuse in comparison to young individuals. However, such misconception has altered the necessity to address the problem of substance abuse in the generation of baby-boomers (those born within 1946 and 1964), whose age-related health issues impose a significant concern related to addiction (European Monitoring Centre for Drugs and Drug Addiction [EMCDDA], 2008).
Due to the diminished attention to addiction problems in the elderly, this issue has been neglected and not addressed properly for decades. As a consequence, substance abuse-related problems in older adults are under-identified, under-diagnosed, and mistreated (Le Roux, Tang and Drexler, 2016).
Now that the numerous population of the baby boom generation is aging, the scope of their health issues extends, thus imposing an urgent need for both scholarly and health care circles to find effective solutions. Indeed, the demographic situation on a global scale demonstrates that the current number of individuals over 60 is the largest in history, comprising 11 per cent of the overall population of the world (Flint, Merali and Vaccarino, 2018). This group increases fast and is anticipated that “the number of individuals over the age of 60 worldwide will reach two billion by 2050, representing 22% of the overall population” (Flint, Merali and Vaccarino, 2018, p. 10).
Since the aging trend will be relevant for the next several decades, it is vitally important to attract professional communities’ attention to the specific features of the elderly. Such a significantly numerous population raises awareness concerning the dominating health care and lifestyle needs that have their particularities for aging individuals.
Importantly, the problem of addiction to substances in older populations is observed in two sets of individuals. They include early-onset users, who start consuming substances at an early age and continue to do so during their adulthood, and late-onset users, who begin using substances later in life. According to Leone, (no date, p. 14), one in three older adults suffering from substance abuse is a late-onset user. Therefore, it is vital to address the issues that the elderly face in their everyday life that might contribute to their overall predisposition to addictive use of alcohol, tobacco, drugs, and other substances.
Taking into account the globally rising tendencies specific to the elderly, an increase in substance abuse in this population is expected in the nearest future. The negative physical, mental, and emotional health outcomes of senior citizens associated with addiction might lead to substantial expenses (Flint, Merali and Vaccarino, 2018). Therefore, it is in the interest of national and global communities to prioritize the needs of the elderly and investigate the particularities of their addiction to substances.
In this paper, the importance of the topic of addiction in the elderly will be broadly addressed. The investigation will be carried out to identify the most commonly used substances among older people, the triggers that contribute to abuse, as well as the possible methods of managing and minimizing addiction in the target population. These ideas will be presented on the basis of an extensive literature review, which will be analyzed as per the strengths and weaknesses. Finally, possible academic implications and concluding statements will be presented.
Rationale for the subject and its importance in the field of addiction and healthcare
Addiction in the elderly should be considered a severe problem due to the growing rate of the prevalence of this population in the world. At present, only few studies are devoted to the investigation of practical solution of this issue. The number of people aged 60 and older increases on a global scale; and the future of global healthcare is anticipated to face an increased need to serve the elderly with addictions. As Flint, Merali and Vaccarino (2018) emphasize, the flow of patients with substance abuse-related morbidities will impose a burden of the national health care systems. Therefore, it is highly recommended to address the issue in a timely manner to ensure the relevant scope of knowledge and adequate preparedness to managing the health care issues of the designated patient group.
Moreover, an insufficient scope of currently available research on the topic diminishes the opportunities for developing necessary treatment and prevention interventions. At the same time, evidence demonstrates that there are significant implications of addiction that have a potential of obstructing the well-being and health of older people. Such adverse consequences of substance abuse include more frequent hospitalization, “death, falls, accidents, acute and chronic cognitive impairment, depression, suicide, and substance withdrawal” (Flint, Merali and Vaccarino, 2018, p. 56). Thus, the importance of the research in the field of addiction in the elderly cannot be overestimated. Additional research is required to understand how substance use impacts different subgroups of the older adults, including people with significant comorbidities and without them. Also, specific guidelines related to substance use need to be developed to help manage short- and long-term addiction.
Structured critical review
Neurobiology
Evidently, the human brain undergoes significant changes in its functioning patterns when one reaches a certain age. When stipulating the topic of addiction in the elderly, one should analyze the changes in brain processes related to aging to ultimately explain how substance abuse as an external factor may affect a human (Flint, Merali and Vaccarino, 2018). With age, older adults experience significant changes in their physical, emotional, and cognitive health domains. These changes make a person more susceptible to diseases and also more vulnerable to the effect of substances. The most vivid impact of substance use is observed within the frameworks of cognitive function, executive function, and brain structure.
Cognitive function
With aging, the quality of cognitive performance predominantly declines in average individuals. Under the conditions of normal aging, some cognitive functions weaken, while others stay stable or improve (Flint, Merali and Vaccarino, 2018). The cognitive processes include verbal communication, memory, perception, processing, and storage of information. However, when attributed with particular drugs, cognition patterns change.
According to Flint, Merali and Vaccarino (2018), alcohol and stimulants have an overall stimulating effect on vocabulary and verbal performance, while ketamine might cause problems with language and information processing. Unlike language, which usually does not worsen in the older age, such crucial cognitive functions as the speed of perception, memory, and reasoning have a tendency to weaken in healthy individuals (Flint, Merali and Vaccarino, 2018). Consequently, when altered by drugs or alcohol, a person fails to perform these functions, which play a crucial role in the overall functioning of the body.
Executive function
The brain of an older person tends to obtain difficulties in performing executive functions. They include “abstract thinking, planning, shifting tasks, reasoning, impulse control and problem-solving” (Flint, Merali and Vaccarino, 2018, p. 39). The aging changes cause cognitive malfunctioning and lead to significant impairments of brain performance. When attributed to substance abuse, the executive functions worsen even more, which has adverse implications for health outcomes and well-being. Indeed, it has been found that such drugs as cocaine, opioids, and cannabis have a negative influence on executive functions (Flint, Merali and Vaccarino, 2018). Therefore, the neurobiological aspect of substances’ effect on an older adult is of vital importance.
Brain structure
Alongside the changes in the brain’s functions, reaching the later stages of life is associated with structural changes in the brain that mediate the functional transformations. The overall worsening of cognitive and executive functions is based on the continuous decline of grey matter in the elderly. Such a change causes neuronal death and is closely related to impairments in pharmacodynamics and pharmacokinetics (Flint, Merali and Vaccarino, 2018).
From this perspective, substance abuse in the older age is very dangerous because it imposes additional challenges for a vulnerable aging brain. Indeed, the brain of the elderly loses the capacity to cope with changes, which is aggravated by the impact of alcohol or drugs and might lead to complete failure to deal with age-related change. In addition, the target population commonly has several illnesses and is prescribed multiple medications. According to Flint, Merali and Vaccarino, (2018), the interactions between several drugs might cause complications and lead to a further decline in brain functioning
Epidemiology
The epidemiological issues related to substance use disorders in the elderly are obstructed by the challenges of under-identification and misconception. The doctors who work with older adults commonly confuse the signs of substance use disorder with other age-related morbidities, such as dementia, diabetes or depression (Addiction in the elderly, no date). Centers for Disease Control and Prevention identified that as of 2015, the number of deaths caused by drug overdose increased for all age groups, including the elderly; “this group is expected to account for about 20 percent of the U.S. population by 2030” (Story 11: addiction in the elderly, 2020).
According to the statistical data presented by Mattson et al. (2017, para. 5), more than 1 million individuals aged 65 or older … had an SUD in 2014, including 978,000 older adults with an alcohol use disorder and 161,000” suffering from addiction to illicit drug use.
Also, the current epidemiologic situation might be characterized by the fact that more than 40 per cent of older adults (aged 65 and older) used four or five prescription drugs simultaneously between 2013 and 2014 (Story 11: addiction in the elderly, 2020). This statistics resembles a significant danger of longer intake of medications or confusion in dosage, which might lead to addiction in the future.
The epidemiologic concerns increase as the prognosis for the future enters the discussion. The implications of recent research show that with the aging of baby-boomers the number of older adults with substance use disorder will increase from approximately 2.8 million cases in 2002–2006 to 5.7 million by 2020 (Mattson et al. (2017, para. 1). It means than more people will encounter addiction and seek treatment.
Research and ethical subjects: the study by Le Roux, Tang and Drexler (2016)
The main objective of the research conducted by Le Roux, Tang and Drexler (2016) was to review the particularities of alcohol use disorder and opioid use disorder in older adults from a psychiatric perspective. The research relevance was justified by the complexity of the issue in the designated population due to health impairments and frequent comorbidities. While alcohol and opioid abuse are substantially researched for young adults, the study suggests a broad overview of the implications specific to older adults, including increased vulnerability and an array of complications (Le Roux, Tang and Drexler, 2016). The authors explain the difficulties in diagnosis and assessment of substance abuse in the elderly due to the complexity of DMS criteria and the inability to withdraw from medication intake for chronic pain. Therefore, a more attentive examination is necessary for professionals to recognize and address addictive behavior in geriatric psychiatry patients.
Despite obstacles and difficulties, substance use disorders in the elderly can be diagnosed, treated and prevented effectively. Le Roux, Tang and Drexler (2016) emphasize that it is vital to raise awareness about the issue, implement an age-specific diagnoses approach, and adhere to a two-fold treatment and preventative interventions system. It should incorporate the efforts “to educate patients about addiction and to motivate (inspire) them to engage a comprehensive program of recovery” (Le Roux, Tang and Drexler, 2016, p. 5). To succeed in the effective management of the issue, the understanding of most prevalent substances, triggers, and treatment methods is needed.
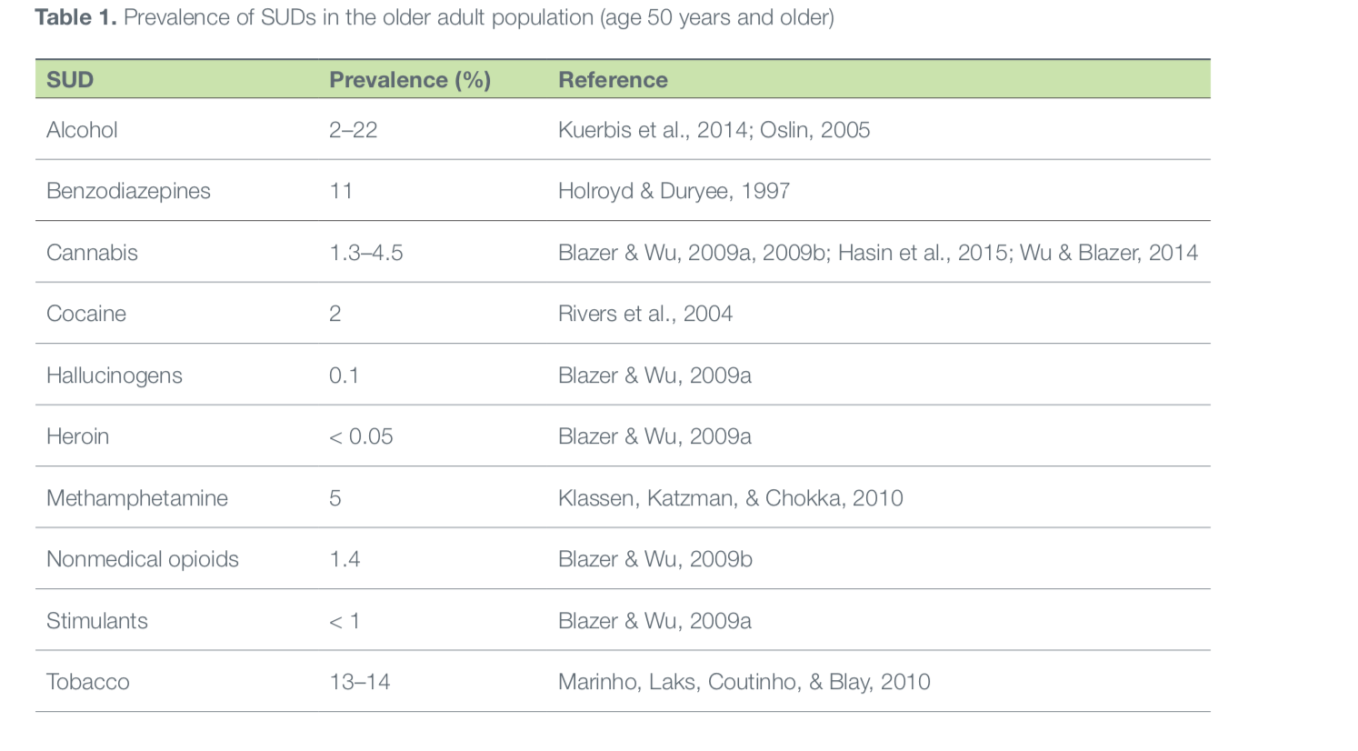
The inclination of the elderly to particular substances derives from their health needs and age-specific changes. Since older adults experience personal aging challenges, chronic illnesses, and extensive medication intake, there exists a high risk of drug overdoses or misuse. According to EMCDDA (2008), older adults are frequent consumers of opioid drugs and over-the-counter medications, which have a common predisposition for causing addiction. However, as Kuerbis et al. (2014) states, although older adults are disproportionately exposed to illicit drugs, alcohol is the prevalent substance frequently used by the population. The statistical depiction of most commonly abused substances presented by Flint, Merali and Vaccarino (2018) supports the observation of Kuerbis et al. (2014) and indicates that alcohol is the leading substance abused by the elderly. Figure 1 shows that in the population aged 50 years and older, alcohol prevalence varies between 2 and 20 per cent while both licit and illicit drugs also inflict a significant threat of addiction (Flint, Merali and Vaccarino, 2018, p. 78).
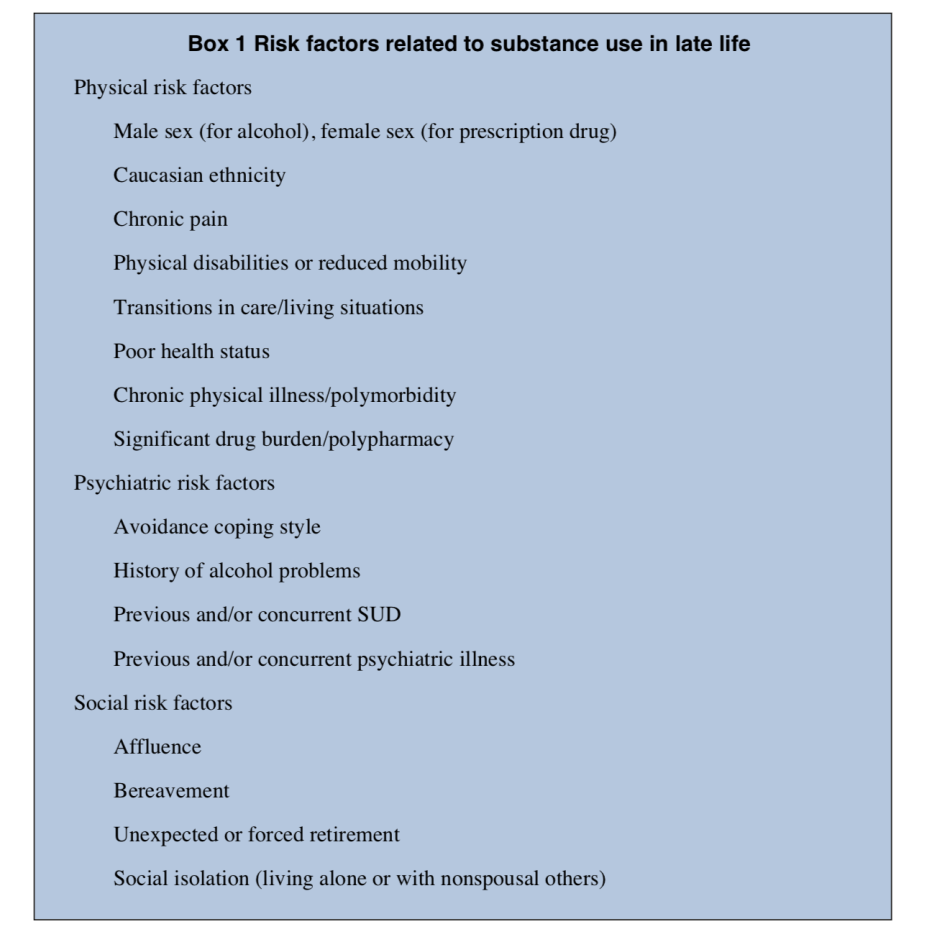
An important issue to consider within the framework of research and ethical considerations of addiction in the elderly is the triggers of substance use. Indeed, senior individuals experience diminished social and professional roles due to retirement, social isolation, and intensification of health problems (Flint, Merali and Vaccarino, 2018). Also, they face such difficulties as obstructed mobility, “death of a spouse, and loss of family support,” which become barriers to adequate health care, as well as impose a significant burden that might lead to substance abuse (Leone, no date, p. 8). It is only natural that older people living under such circumstances experience severe challenges adjusting to the problems, especially when they need to deal with them without adequate support.
Although there is an array of determinants contributing to the development of addictive behavioral patterns, the most generally applicable one is the need of senior citizens to use drugs as pain relief. Eighty per cent of adults aged 65 and older have chronic medical conditions and use drugs for treatment, as well as intake painkillers, tranquilizers, and sedatives (Dean, 2017). Thus, addiction might occur unexpectedly and innocently. Other risk factors that trigger substance abuse include psychological issues, physical characteristics, and social determinants. As seen from Figure 2, senior individuals are at a high level of risk of adopting addictive use of substances due to the inevitable changes in their lives with age (Kuerbis et al., 2014, p. 651).
Specific treatment measures need to be developed on the basis of prevalent substances and triggers. The currently used treatment fails to address the needs of aging population to the full extent (Ministry of Health, 2011). In the face of the complexity of the issue, effective management of substance use in older adults “requires continuing care and interaction across many disciplines, such as pharmacological, behavioral therapy and social support” (United Nations Office on Drugs and Crime, 2018, p. 51).
However, it has been found that older generation responds well to the treatment measures. Numerous facilities provide professional help for older patients to overcome the disease within multiple dimensions of care. The options of addiction management vary and include age-specific and general methods, as well as preventative, medical detox, residential care, and outpatient treatment (Kuerbis et al.,2014).
Importantly, a complex interdisciplinary approach is required to ensure the multifaceted management of the problem. For that matter, Leone (no date, p. 31) suggests that the implementation of “the bio-psycho-social-spiritual model of treatment” will provide the best results. Overall, the needs of particular subgroups of the target population must be addressed through a complex set of treatment interventions.
Strengths and weaknesses of the undertaken literature review
The main strength of the literature review is the ability of the studies to provide an extensive overview of the particularities of addiction in the elderly. Despite the fact that the issue has been actively discussed only within the past decade, most reports and studies provide sufficient data to build strategies for future research. The research by Le Roux, Tang and Drexler (2016) allowed for identifying the complexity of substance abuse in the elderly and obtain the insights as per the ways of treatment.
Some of the weaknesses include the tendency of most studies to address the challenges to diagnosis and treatment rather than finding ways to solve the problem. Limited attention is played to the successful cases of treatment that might be used as guidelines for future interventions. Moreover, a gap in studies on addiction in the elderly from the Arab countries was identified during the literature review.
Possible practical or academic implications for the review
The review provides thorough data on the causes of the problem and possible solutions. The study by Le Roux, Tang and Drexler (2016) introduces optimistic predictions as per the effectiveness of diagnosing, managing, and preventing substance use in older adults. The overall literature review contributes to the scope of investigation of this under-studied issue and might be used as a credible ground for both further academic research and intervention development.
To ensure timely identification of SUDs in the elderly, over-the-counter drug use and treatment response monitoring is required (EMCDDA, 2008). Health care system needs to prepare for the increase in the number of older patients with addictions. Psychological and social determinants need to be reviewed when assessing the elderly for SUDs. Improved age-specific screening measures must be implemented to identify both alcohol and drug addiction in senior citizens (EMCDDA, 2008). Finally, the modification of current SUDs treatment is imperative to ensure effective addressing of comorbidities and other age-specific particularities.
Summary/conclusion
People aged 65 and older are statistically more exposed to medication intake due to their age-related health changes. The majority of substance abuse treatment programs and research is devoted to younger adults rather than the elderly. The global growth of the older population is expected in the nearest future. Therefore, it is vital to incorporate the knowledge about the commonly abused substances, triggers or addiction, and the predispositions of senior citizens to drug misuse in order to develop an effective system of treatment and prevention methods.
Reference List
Addiction in the elderly (no date). Web.
Dean, O. (2017) ‘Prescription drug abuse among older adults’, AARP Public Policy Institute. Web.
European Monitoring Centre for Drugs and Drug Addiction (2008) ‘Substance use among older adults: a neglected problem’, Drug in Focus, 1, pp. 1-4.
Flint, A. J., Merali, Z. and Vaccarino, F. J. (2018) Improving quality of life: substance use and aging. Ottawa: Canadian Centre on Substance Use and Addiction.
Karlson, K. A. (1994) The prevention of substance abuse and misuse among the elderly. Web.
Kuerbis, A. et al. (2014) ‘Substance abuse among older adults’, Clinics in Geriatric Medicine, 30(3), pp. 629-654.
Leone, M. A. (no date) [PowerPoint Presentation]. Mental health, substance use, and aging: prescription abuse in our aging population. Web.
Le Roux, C., Tang, Y. and Drexler, K., (2016) ‘Alcohol and opioid use disorder in older adults: neglected and treatable illnesses’, Current Psychiatry Reports, 18(9), p. 1-11.
Mattson, M. et al. (2017) ‘A day in the life of older adults: substance use facts’, Substance Abuse and Mental Health Services Administration. Web.
Ministry of Health (2011) Mental health and addiction services for older people and dementia services: Guideline for district health boards on an integrated approach to mental health and addiction services for older people and dementia services for people of any age. Wellington: Ministry of Health.
Story 11: addiction in the elderly (2020). Web.
United Nations Office on Drugs and Crime (2018) Drugs and age drugs and associated issues among young people and older people. Web.