Introduction
Bloodstream infections (BSIs) are common and life-threatening despite being preventable. BSI’s, also known as sepsis, are associated with many morbidities and mortalities amongst patients. Yearly, a third of all mortalities that occur amongst patients can be related to BSIs. They lead to far-reaching effects on patient care (Aliyu et al., 2018). Some of the effects include prolonged hospital stay, high hospital costs, poor clinical outcomes, and reduced patient satisfaction (Viscoli, 2016). The implications are profound in patients with low immunity, such as newborns, the elderly, and immunocompromised due to other underlying conditions. BSI is extensively experienced by patients whose skin integrity is impaired, such as those suffering from chronic dermatitis, renal failure, and malignancies.
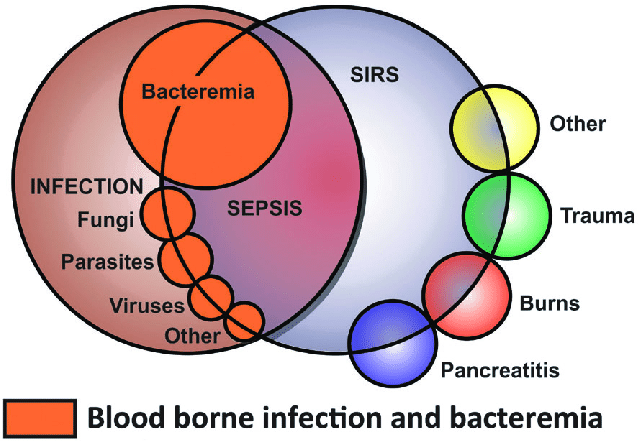
Bloodstream infections can occur due to the spread of local disease or the introduction of microorganisms into the blood system (Banik et al., 2018). As showed in Figure 1 above, bacteria play a significant role in the causation of blood steam infections as compared to other organisms such as fungi, viruses, and bacteria. Interference with skin integrity through trauma or burns creates the microorganisms that can get into the body’s blood system. Clinical activities, including the use of invasive devices during patient care, can develop through which microorganisms get into the blood system leading to BSIs.
.
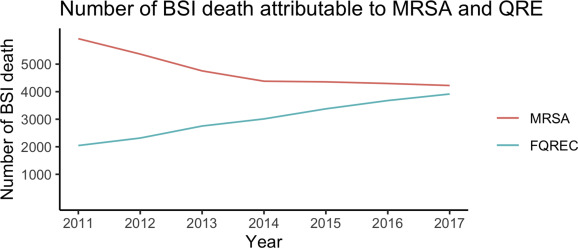
Blood stream infections form a significant percentage of the acquired infections in the hospital settings. According to Franco-Paredes (2016), BSIs account for up to 15% of real cases. Most poof, the affected patients are admitted staying more than 48 hours in the hospital setting. BSI’s that are community-acquired can also occur as shown in Figure 1, which highlights various risk factors that could predispose an individual to acquiring BSIs. Some of the issues that can contribute to contracting of BSIs include old age, low immunity, hospitalization, improper practices during catheter use, during dialysis if aseptic technique is not followed, among many others. Usually, the prognosis for individuals with bloodstream infections is poor (Hallam et al., 2018). As shown in Figure 2, mortalities have been reported amongst patients related to BSIs. The outcomes are worse in case of late diagnosis, wrong interventions, underlying conditions. BSIs can lead to systems making the individual situation critical to be managed in regular wards. Most patients admitted to the ICU have community-acquired infections, especially bacteremia.
Data Presentation
The data will be presented to the rest of the class physically through a class video conferencing. Additionally, a softcopy material will be shared on the classroom online forum. The presentation can also be transferred to other class members through the class official email before the actual presentation. The class members will be expected to participate in the presentation actively and react by seeking clarification, asking questions, and/or commenting on the presentation’s findings.
Improvement of Proposed Solutions
Sepsis can be a threat to an individual’s life, hence, it requires early recognition and appropriate intervention. Despite it being common amongst patients, it is preventable with right precautions (Bell & O’Grady, 2017). BSIs are caused by either localized spread of infections or introduction of microorganisms into the surrounding blood system. Mostly, invasive devices such as intravenous cannulas, central lines, urinary catheters, and hemodialysis catheters can be the infection source. The use of invasive devices contributes to a larger percentage of BSI experienced by patients, especially in the clinical setting. Septic procedures during insertion and maintenance of the instruments lead to allowing microorganisms to access the blood system, hence causing infection.
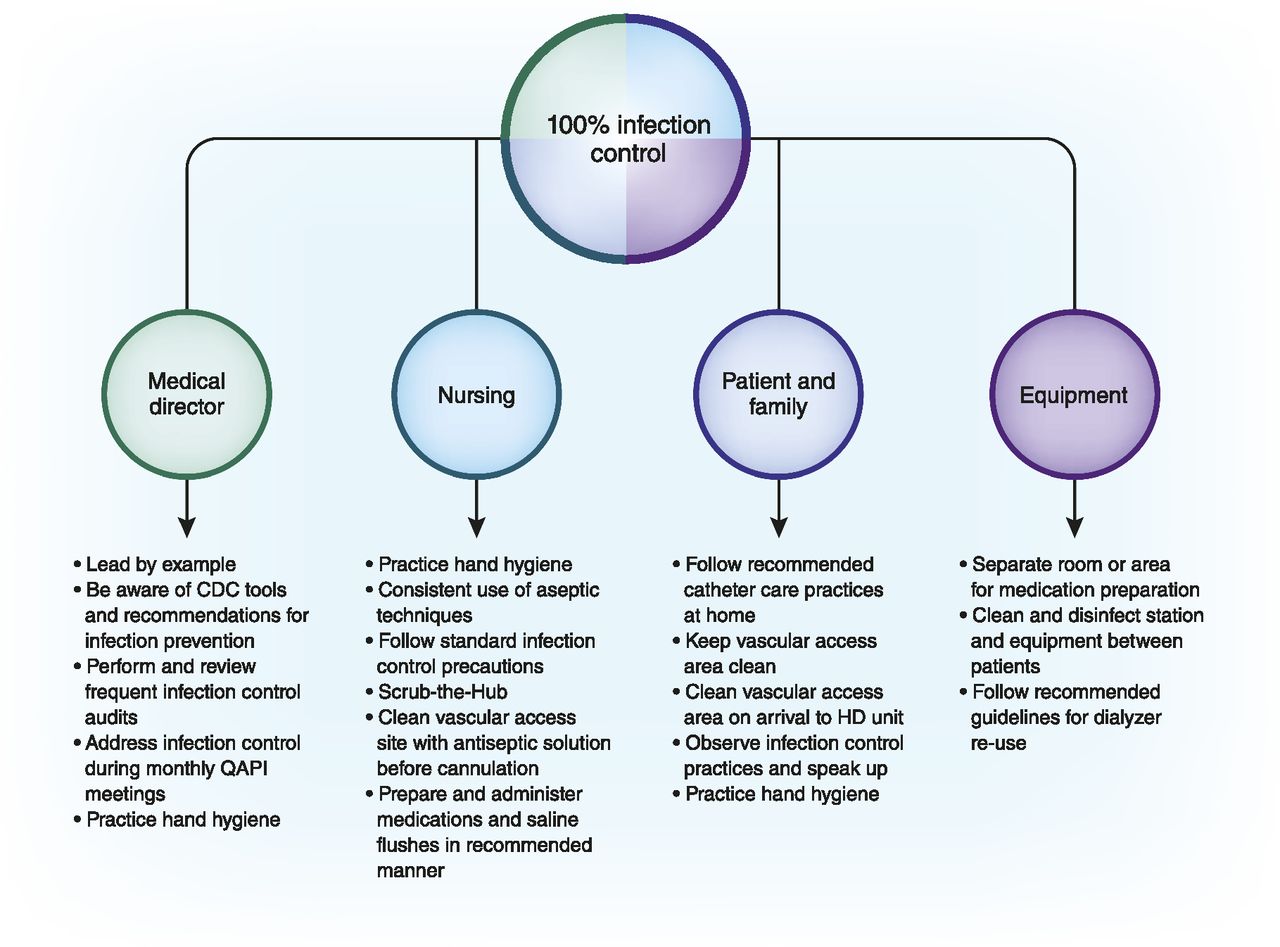
Prevention of BSIs is a teamwork process, which requires educating the care providers and patients on marinating aseptic surroundings while handling invasive devices is necessary to prevent blood system infections. According to Bell and O’Grady (2017), whenever an invasive device is involved in patient care, the spread of sepsis increases. Therefore, training individuals on invasive devices to reduce blood infections will work efficiently towards achieving the mission (Vijayan & Boyce, 2018). The concerned members will ensure appropriate precautions are put in place to prevent occurrence of the infections.
Most of the infections are related to exposure to unsafe clinical environment and physiological factors. According to Franco-Paredes (2016), sepsis occurs as a result of underlying complications. Usually, it originates from other conditions, mostly localized infections within the body systems, such as the urinary tract, skin, lungs, or abdomen. Once the infection spreads, the immune system responds by activating septic reaction, which is life-threatening. Various microbes, such as fungi, viruses, and bacteria, can cause sepsis, but bacteria are the common cause. This aspect makes early recognition and treatment of infections essential in avoiding BSIs.
Setting up rules and regulations that govern the avoidance and provision of standard guidelines on BSIs can work well towards the reduction of BSIs. Some health care facilities across the nation have developed, adopted, and even implemented quality practices geared towards reducing BSIs (Viscoli, 2016). Evidence-based practices, such as suitable training, provision of required equipment and resources have positively helped achieve the goal. Additionally, research activities based on BSIs also improve the quality of care (Hallam et al., 2018). Through studies, real situations are visualized forming the basis for evaluation and change. The findings are also used in making crucial decisions regarding acquisition of the appropriate resources and equipment for reducing BSIs.
Preferred Solution
Based on the impact on the desired outcome, solutions are prioritized. In this situation of BSIs, research activities are given more credit. The corresponding insights before implementation of the interventions are crucial in addressing the functional challenges. It also assists in determining the root cause of the problem and the most appropriate solution. Research findings also form the basis for evaluation after a specified period. Therefore, one can identify resources needed for completion of the mission, BSIs reduction. Therefore, it is through exploration that one can determine which strategy can be applied to yield the nest results as expected. Evidence-based practices on the prevention and management of BSLs cases will be acquired and adopted through research activities.
How Will the Change Be Sustained?
For the change to be sustained, it has to be part of the corporate culture. The change can be included in the organizational policies and guidelines of practice making it compulsory for individuals practicing under the umbrella of those policies to follow. Therefore, the organization administrative personnel, departmental leaders, and any other team that may be appointed to oversee the change will be responsible for reinforcement of set rules and regulations. In this case, conducting research activities pertaining to BSIs, implementation of findings, and evaluation will be a culture for care providers. Cooperation, teamwork, and commitment from every member will be ultimate expectations, as the whole team remains focused on the betterment of practices, especially about BSIs.
Conclusion
Blood Stream infections are one of the common epidemiological burdens to the health care system. The conditions are expected with poor medical prognosis despite being preventable. BSIs have to increase morbidities, mortalities, prolonged hospital stay, and increased medical costs. The quality of life is reduced, and some factors associated with BSIs include old age, hospital, ratio, use of invasive devices during patient care, and lost skin integrity. Ensuring sterility when handling invasive devices, provision of education on BSIs, and conduction research activities are some of the identified ways to reduce BSIs.
References
Aliyu, S., Cohen, B., Liu, J., & Larson, E. (2018). Prevalence and risk factors for bloodstream infection present on hospital admission. Journal of Infection Prevention, 19(1), 37– 42. Web.
Banik, A., Bhat, S. H., Kumar, A., Palit, A., & Snehaa, K. (2018). Bloodstream infections and trends of antimicrobial sensitivity patterns at Port Blair. Journal of laboratory physicians, 10(3), 332. Web.
Bell, T., & O’Grady, N. (2017). Prevention of central line–associated bloodstream infections. Infectious Disease Clinics of North America, 31(3), 551-559. Web.
Franco- Paredes, C. (2016). Core concepts in clinical infectious diseases (CCCID) (1st ed.). Elsevier Science.
Hallam, C., Jackson, T., Rajgopal, A., & Russell, B. (2018). Establishing catheter-related bloodstream infection surveillance to drive improvement. Journal of infection prevention, 19(4), 160 — 66. Web.
Kell, D. B., & Pretorius, E. (2015). On the translocation of bacteria and their lipopolysaccharides between blood and peripheral locations in chronic, inflammatory diseases: The central roles of LPS and LPS-induced cell death. Integrative Biology, 7(11), 1339-1377. Web.
Tsuzuki, S., Matsunaga, N., Yahara, K., Gu, Y., Hayakawa, K., Hirabayashi, A., & Ohmagari, N. (2020). National trend of blood-stream infection attributable deaths caused by Staphylococcus aureus and Escherichia coli in Japan. Journal of Infection and Chemotherapy, 26(4), 367-371. Web.
Vijayan, A., & Boyce, J. M. (2018). 100% use of infection control procedures in hemodialysis facilities: Call to action. Clinical Journal of the American Society of Nephrology, 13(4), 671-673.
Viscoli, C. (2016). Bloodstream infections: The peak of the iceberg. Virulence, 7(3), 248-251. Web.