Clinically Based Patient Problem
The patient’s problem for this paper is Candida Auris. It is a yeast that causes severe illnesses among hospitalized patients. It is particularly dangerous because it is often resistant to common antifungal drugs (Centers for Disease Control and Prevention, 2017). Moreover, it can enter the patient’s bloodstream and become a reason for invasive infections. Other reasons why Candida Auris is a burden of contemporary healthcare providers is the difficulty in identifying it with the help of standard laboratory tests because it is similar to other Candida species, and, due to its multidrug resistance, it leads to outbreaks in healthcare facilities (Centers for Disease Control and Prevention, 2017). Therefore, it is important to identify Candida Auris quickly and prevent its further development within or outside healthcare settings.
Candida Auris can contaminate the surrounding surfaces within healthcare facilities (Sears & Schwarts, 2017). Therefore, it is necessary to control the infection and prevent its spreading. One of the opportunities for infection control is the use of a database management approach. Data of patients with Candida Auris are recorded in EHRs that are available throughout the facility. Such an application of EHRs is expected to inform healthcare professionals and allow them to avoid unnecessary unprotected contacts with the infected patients and thus limit the spread of infection. Moreover, since EHR keeps the information about all manipulations with patients, it can allow revealing the source of infection.
A Database to Assist the Problem
Information from the electronic health record can assist in the identification and prevention of the infection (Lee, 2017). Previous studies provide evidence of the efficiency of EHR for identifying risk factors for Clostridium difficile infection relapse in hospital settings (Hebert, Du, Peterson, & Robicsek, 2013). Consequently, similar methods can be applied to identify patients at risk of Candida Auris and define the source of infection. According to the Centers for Disease Control and Prevention (2017), risk factors for Candida Auris are similar to those typical of other types of Candida infections. Thus, “recent surgery, diabetes, a broad-spectrum antibiotic, and antifungal use” are the risk factors to consider (Centers for Disease Control and Prevention, 2017, para. 7). Moreover, patients of nursing homes and those having breathing tubes, feeding tubes, and central venous catheters are at higher risk for Candida Auris infection compared to other patients. At the same time, age is not a meaningful factor for this infection.
Thus, a database that can assist the solution of the Candida Auris problem should contain the following patient data extracted from EHR. First of all, it is important to include patients’ personal data, such as their name, date of birth, and gender. They are necessary for further identification of the patient. Also, the patient’s address is included in case it is necessary to check their family. The most informative data that can help identify risk groups for Candida Auris include patient history and the list of recent manipulations provided in or outside the current healthcare setting. These data are significant because they allow the identification of patients at risk and also provide an opportunity for determining the source of infection.
Patient Problem Description
The clinical patient problem under consideration is Candida Auris, which is a pathogen that has spread over five continents and resulted in outbreaks of infection in diverse healthcare settings (Jeffery-Smith et al., 2017). Since Candida Auris is difficult to identify due to its similarity to other Candida types, the infection can spread quickly and result in negative patient outcomes. Therefore, it is necessary to develop tools that empower the identification of risk groups and can prevent the spread of infection within healthcare settings.
To manage a patient’s condition, information about patient history is necessary. It is important to know the reasons for hospitalization, comorbid conditions such as diabetes that increase the risk of Candida Auris, recent surgeries, intake of prescribed broad-spectrum antibiotics, and antifungal medication. Moreover, the history of such manipulations as the insertion of tubes or catheters should be recorded since they also increase the risk of getting Candida Auris. Timely detection of this pathogen allows placing patients in private rooms to avoid the further spread of infection. Moreover, the availability of information about patients with Candida Auris through a database comprising data from EHR is an opportunity for healthcare providers to use protective measures when contacting a patient. Also, it makes environmental control interventions possible. For the patient to manage Candida Auris, it is necessary to provide information about safety measures. Also, hygiene guidelines are significant both to patients and healthcare providers to prevent the spread of infection. An important aspect is the choice of medication to treat the patient. Since Candida Auris is not sensitive to many commonly applied medications, additional tests can be needed to define an effective drug. Moreover, patients should be informed about the peculiarities of medicine intake to ensure the effectiveness of treatment.
Identification of EHR-Supplied Data
EHR-supplied data used in a database will be structured. According to Ateya, Delaney, and Speedie (2015), structured data are preferable for electronic health records because they facilitate the inclusion of patient information into the clinical process and simplify the use of these data. Still, some unstructured data will be used, such as the patient’s name and address. Thus, for the clinical problem under consideration, the following entities can be included in the database. First of all, personal patient data with attributes will be added: name (unstructured entity), gender (male or female), age (selected from the list), date of birth (selected in the calendar), address (unstructured data). The second block of information will include patient history.
Previous hospitalizations (dates and reasons for them) are all cases of the patient being administered to a hospital. Medications taken during the past month (names, doses) are the substances taken by the patient within a month before the health record is completed. Current medications (names, doses) are the substances that the patient takes at the moment the health record is completed. Chronic diseases (type, if applicable, for how long the patient has been ill) are the conditions the patient experiences for some period of time that were diagnosed as chronic. Recent surgeries (reason, date) are all surgery interventions experienced by the patient within the period of two previous months. The experience of lines and tubes (type, for how long they were applied) are the interventions that demanded the use of these appliances, both in hospital and long-term care settings.
Description of Data Entities
To develop an efficient database, it is important to extract the necessary data with all attributes from the patient’s EHR (Lee, 2017). The following structure can be used to assist the development of a database that comprises all important aspects necessary for identifying patients at risk of being infected with Candida Auris (See Figure 1).
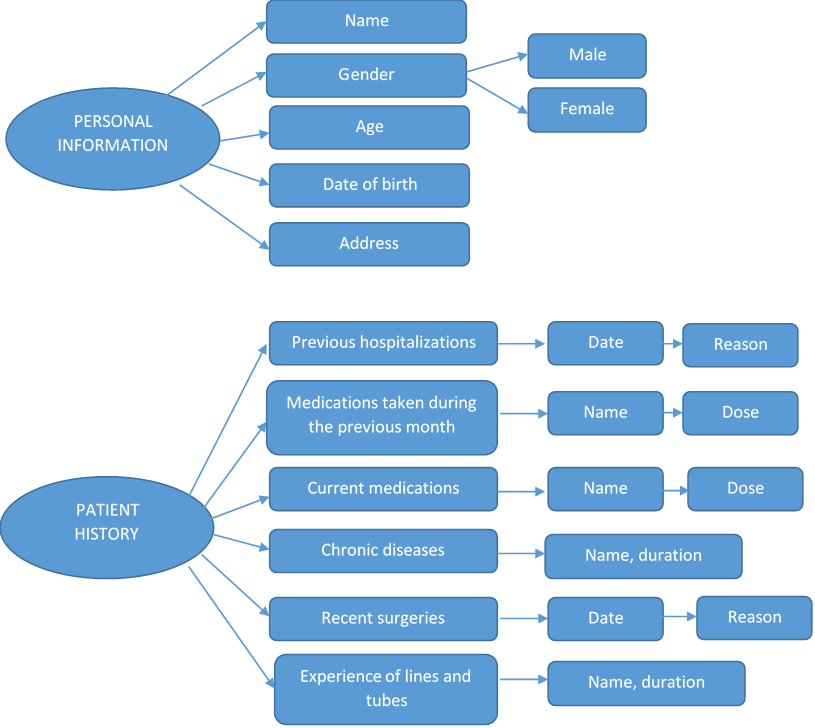
While the section with personal information is standard, the one with patient history details necessary for determining patients at risk of Candida Auris infection or defining the source of infection needs an explanation. Thus, information about previous hospitalizations and recent surgeries allows assessing one of the risk factors for Candida Auris because this infection develops in the hospital setting. Recent and current medications are needed to identify if there are or were any broad-spectrum antibiotic or antifungal medications used by the patient, which is another risk factor. Moreover, in case the patient took certain antibiotics, there can be problems with the choice of treatment strategies. The knowledge about the patient’s chronic diseases is also important because some of them, such as diabetes, can increase the risk of getting infected by Candida Auris. Finally, the insertion of lines and tubes during hospitalizations and surgeries should be considered since it is one of the ways of getting infected.
References
Ateya, M., Delaney, B., & Speedie, S. (2015). The value of structured data elements from electronic health records for identifying subjects for primary care clinical trials. BMC Medical Informatics and Decision Making, 16(1). Web.
Centers for Disease Control and Prevention. (2017). General information about Candida auris. (2017). Web.
Hebert, C., Du, H., Peterson, L., & Robicsek, A. (2013). Electronic health record–based detection of risk factors for Clostridium difficile infection relapse. Infection Control & Hospital Epidemiology, 34(04), 407-414. Web.
Jeffery-Smith, A., Taori, S., Schelenz, S., Jeffery, K., Johnson, E., Borman, A., … Brown, C S. (2017). Candida auris: A review of the literature. Clinical Microbiology Reviews, 31(1), e00029-17. Web.
Lee, K. (2017). Benefits of EHRs include tracking the spread of infection in hospitals. SearchHealthIT. Web.
Sears, D., & Schwartz, B. (2017). Candida auris: An emerging multidrug-resistant pathogen. International Journal of Infectious Diseases, 63, 95-98. Web.