Shigellosis: Transmission
Shigellosis is a diarrheal disease caused by a group of bacteria called Shigella.
Types:
- Shigella sonnei (the most common in the US);
- Shigella flexneri;
- Shigella boydii;
- Shigella dysenteriae.
Shigella germs are found in infected stools of individuals.
Shigella is highly contagious – exposure to a minute contaminated fecal matter causes infection.
Transmitted when infected objects come into contact with the mouth or is swallowed:
- Contaminated hands touch food or mouth;
- Consuming food contaminated with Shigella;
- Swallowing recreational during swimming from any water source;
- Contact with feces through sexual contact.
(Centers for Disease Control and Prevention, 2015b).
Shigellosis: Signs/Symptoms
Symptoms of shigellosis are generally noted 1 to 2 days after exposure.
Causes gastroenteritis manifested through:
- Diarrhea (may be bloody);
- Fever;
- Abdominal pain;
- Tenesmus (a painful urge to pass stool but the bowel is empty).
For healthy persons, symptoms last about 5 to 7 days.
Reinfection with the similar types of Shigella is usually difficult and can take several years.
Shigellosis: Prevalence
Estimates
- About 500,000 cases of shigellosis reported the US annually;
- 5,400 hospitalizations and 38 deaths;
- Lacks definite seasonality thus reflects the significance of person-to-person transmission.
Incidence
- In 2013, the US reported 4.82 cases per 100,000 individuals.
Trends
- No significance decline in the last 10 years;
- Shigella sonnei infection rate declined between 2008 and 2011, but increased in 2012 (Centers for Disease Control and Prevention, 2015b).
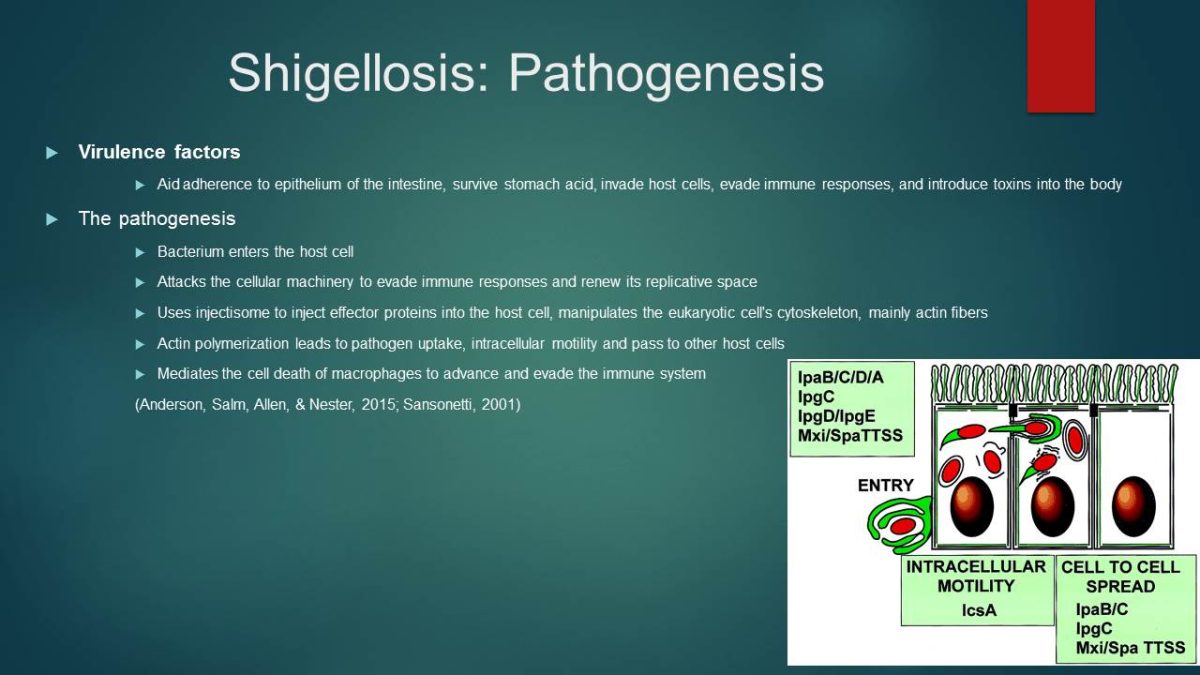
Shigellosis: Pathogenesis
Virulence factors
Aid adherence to epithelium of the intestine, survive stomach acid, invade host cells, evade immune responses, and introduce toxins into the body.
The pathogenesis
- Bacterium enters the host cell;
- Attacks the cellular machinery to evade immune responses and renew its replicative space;
- Uses injectisome to inject effector proteins into the host cell, manipulates the eukaryotic cell’s cytoskeleton, mainly actin fibers;
- Actin polymerization leads to pathogen uptake, intracellular motility and pass to other host cells;
- Mediates the cell death of macrophages to advance and evade the immune system (Anderson, Salm, Allen, & Nester, 2015; Sansonetti, 2001).
Shigellosis: Treatment
Treatment
- Diarrhea resolves alone without antibiotics after 5 to 7 days;
- Mild cases may require only fluids and rest;
- Bismuth subsalicylate – Pepto-Bismol® is necessary;
- Avoid loperamide and diphenoxylate (antidiarrheal medicines) because they cause slow down of the gut and worsen the condition;
- Severe cases require antibiotics to reduce the duration of symptoms;
- Use of bacteriophage.
Antibiotic Resistance
- Shigella is often resistant to antibiotics;
- Stool culture is necessary for effective antibiotics;
- Report outcomes within few days after antibiotics administration.
Shigellosis: Outcome
Positive treatment outcomes are expected with antibiotics.
However, antibiotic resistance often occurs:
- Report outcomes within few days after treatment;
- Further susceptibility tests will be conducted to determine the most effective antibiotics;
- Ampicillin may be replaced with flouroquinolones and azithromycin.
No licensed vaccine available for Shigella (Centers for Disease Control and Prevention, 2015b).
Shigellosis: Prevention
No licensed vaccine is currently available for Shigella.
Reduce risks of person-to-person through:
- frequent, thorough hand washing before eating and after changing diapers or helping other individuals who have defecated.
Handle infected feces carefully.
Do not drink or swallow water from ponds, lakes, rivers, or untreated swimming pools.
Adhere to strict guidelines on water and food hygiene.
Avoid sexual intercourse with persons who diarrhea or have recently recovered (Centers for Disease Control and Prevention, 2015b).
Typhoid Fever: Transmission
- Life-threatening, contagious illness caused by bacterium, SalmonellaTyphi;
- Salmonella Typhisurvives only in humans;
- Bacteria are found in the bloodstream and intestinal tract;
- Carriers usually recover from typhoid fever but still have the bacteria;
- Stools of infected persons carry bacteria;
- Eating food or drinking beverages contaminated by SalmonellaTyphi causes typhoid fever;
- Salmonella Typhibacteria multiply and move into the bloodstream (Centers for Disease Control and Prevention, 2013).
Typhoid Fever: Signs/Symptoms
- High sustained fever – as high as 103° to 104° F (39° to 40° C);
- Weaknesses;
- Stomach pains;
- Headache;
- Loss of appetite;
- A rash of flat, rose-colored spots;
- It is recommended to perform stool or blood test to determine the presence of Salmonella Typhi– the only sure way.
Typhoid Fever: Prevalence
Common in most parts of the underdeveloped world (about 21.5 million persons each year):
- Asia;
- Africa;
- Latin America.
Not so common in developed countries such as:
- The United States (5,700 cases occur annually, about 75% results from foreign travels);
- Canada;
- Western Europe;
- Australia;
- Japan.
Typhoid Fever: Pathogenesis
Salmonella Typhienters the mucosa of small and large bowel.
Stays intracellularly and proliferate.
Ulceration of lymphoid follicles may take place.
Initial developments occur in the second section of patches of the lower small intestine.
Systemic dissemination takes place to:
- Liver;
- Spleen;
- Reticuloendothelial system.
Between 1 to 3 weeks, the bacteria multiply in these organs.
Infected cells rupture.
Bacteria move to the bile and infect the lymphoid tissue of the small intestine, the ileum.
Heavy infection occurs.
Invasion of mucosa occurs.
The epithelial cells release various proinflammatory cytokines (Singh, 2001).
Typhoid Fever: Treatment
Individuals experiencing high fever and feel weak should see the doctor immediately.
Antibiotics are administered in confirmed cases.
Several cases of antibiotics have been reported:
- Reduced susceptibility to fluoroquinolones;
- The emergence of multidrug-resistance, particularly in South Asia.
Antibiotic susceptibility testing is recommended for effective treatment.
Antibiotic therapy include:
- Fluoroquinolones;
- Ceftriaxone;
- Azithromycin (Centers for Disease Control and Prevention, 2013).
Typhoid Fever: Outcome
- Administered antibiotics should have positive outcomes;
- Cases of resistance may complicate treatment;
- Individuals who fail to get treatment may still have the fever for months;
- About 20% die from typhoid fever complication;
- Symptoms may disappear but the person may still be carrying SalmonellaTyphi;
- Symptoms may recur;
- Infected persons may pass the disease to other individuals;
- It is recommended to complete the dose;
- Stool culture is necessary to determine that no Salmonella Typhi is left in the body.
Typhoid Fever: Prevention
Do not consume risky foods and drinks.
Vaccination is highly recommended:
- Ty21a (Vivotif Berna, Swiss Serum and Vaccine Institute);
- ViCPS (Typhim Vi, Pasteur Merieux);
- Note: Vaccines are not completely effective.
Maintain optimal hand hygiene.
Food should be:
- Thoroughly cooked;
- Peeled off;
- Washed;
- Do not consume foods and drinks from street vendors.
Cholera: Transmission
- Cholera is an acute intestinal infection caused by strains of the bacteria Vibrio cholerae;
- Cholera has a short incubation period and produces enterotoxin that causes watery diarrhea that lead to dehydration;
- Vibrio cholerae is present in stool or other effluent of an effected person;
- The bacteria seep into and contaminate waterways, soils, or sources of drinking water and food;
- On drinking or using infected water for washing, a healthy person can get infected by the bacteria;
- Hygiene plays a key role in cholera transmission and it is one measures of a country’s social development.
Cholera: Signs/Symptoms
Cholera symptoms may be manifested within two hours of infection.
Most cases may take 7-14 days before falling ill, although Vibrio cholerae is present in their feces.
The primary symptom is copious, painless, water rice diarrhea, that leads to dehydration manifested through:
- Rapid heart rate;
- Low blood pressure;
- Loss of skin elasticity;
- Muscle cramps;
- Thirst.
Vomiting is also common among many patients.
Cholera: Prevalence
Situation
In 2013, the WHO received 129, 064 cases from 47 countries globally (World Health Organization, 2016):
- Africa reported 43%;
- Americas reported 47%.
Cholera annual global burden is estimated 1.4 to 4.3 million cases and 28000 to 142000 deaths.
In 2015, WHO responded to multiple Cholera out breaks, especially in the Eastern Mediterranean and African regions.
Global reporting is not accurate due to fears of negative impact on travel and trade.
Trends
- Endemic countries include India, Indonesia, Zimbabwe, and other African and Southern Asia countries.
- Between 2001-2009, Africa reported 93% to 98% of total global cases.
- The increasing outbreak in the island of Hispaniola, Haiti and the Dominican Republic from 2010 and the decreasing cases from Africa since 2012 has drastically changed the proportion.
Cholera remains a significant public health problem, especially in Sub-Saharan Africa, Southern Asia and in Hispaniola (World Health Organization, 2016).
Cholera: Pathogenesis
- Approximately 2/3 of Vibrio cholerae survive the acidic condition of the host digestive tract;
- In the host small intestine, the bacteria produce long tail-like structures, flagella, that help them to propagate and move through intestinal mucus to the intestinal wall;
- In the intestinal wall, the bacteria produce figure like projections, frimbriae or pili, for attachment;
- The bacteria multiply necessitating more space and new hosts;
- They toxic protein to propel new multiplying bacteria to external environment for new hosts.
Cholera: Treatment/Outcome
- Rehydration therapy reduces fatalities to under 1% of all patients;
- Oral rehydration solution (ORS) , boiled salty water, breastfeeding for infants.
- Intravenous rehydration.
Antibiotic treatment is used as an adjunct to hydration treatment, especially for severely ill patients (Centers for Disease Control and Prevention, 2015a):
- Severe dehydration; Doxycycline, and Tetracycline: Erythromycin recommended for children;
- Moderate or severe dehydration; Doxycycline, Ciprofloxacin, Azithromycin: Erythromycin, Azithromycin for pregnant women and children.
Zinc treatment:
- Zinc supplements significantly reduces duration and severity of diarrhea, especially in children.
Cholera: Prevention
- Proper and regular washing of hands with soap and water, in absences of soap, sand or ash can be used;
- Proper feces disposal (use of latrine or chemical toilet);
- Avoiding defecating in water bodies;
- Toilets should be dug 30 meters from water bodies;
- Drinking and using safe water; bottled water with unbroken seals, boiled and chlorine treated water, and stored in clean covered containers;
- Food should be properly cooked, covered, and eaten while hot;
- Fruits must be cleaned and pealed;
- Vaccination recommended;
- Proper and thorough cleaning of kitchens, bathrooms and clothing.
References
Anderson, D., Salm, S., Allen, D., & Nester, E. (2015). Nester’s Microbiology: A Human Perspective (8th ed.). Whitby, ON: McGraw-Hill.
Centers for Disease Control and Prevention. (2013). Typhoid Fever. Web.
Centers for Disease Control and Prevention. (2015a). Cholera. Web.
Centers for Disease Control and Prevention. (2015b). Shigella – Shigellosis. Web.
Sansonetti, P. J. (2001). Shigellosis: from symptoms to molecular pathogenesis. American Journal of Physiology – Gastrointestinal and Liver Physiology, 280(3), G319-G323.
Singh, S. (2001). Typhoid Fever: Pathogenesis and Laboratory Diagnosis. Journal of Indian Academy of Clinical Medicine, 2(1), 17-20.
World Health Organization. (2016). Number of Reported Cholera Cases. Web.