Introduction
The thyroid gland is one of the most important glands in the body. It is positioned at the front side of the neck. It is made up of two lobes which are found on either side of the trachea. Normally the gland is not externally noticeable or felt with a finger pressed on the neck. It produces two hormones that control the most metabolic processes in the body, which include energy provision and growth. The hormones produced are tetraiodothyronine (T4 or thyroxine) and triiodothyronine (T3). These hormones differ in their iodine molecule abundance. T4 is the inactive form of the hormone. It comprises 90 percent of the hormones produced by this gland. T3 is the active hormone with three iodine molecules (Maggi et al., 2013).
The thyroid hormones are made in the colloidal follicles. Plasma iodine is taken up in the follicular cells using a sodium pump and into the colloidal follicles. A protein known as thyroglobulin is made by the follicular cells through the cellular mechanisms and released into the colloidal follicles. Four Iodine molecules are then linked into the thyroglobulin and tyrosine residues to form the precursor of T4 and three molecules of iodine are linked to form the precursor of T3. On stimulation with thyroid-stimulating hormone (TSH), the follicular cells engulf parts of the colloid and phagocytose it. The thyroglobulin is then cleaved and T3 and T4 are liberated (Visser et al., 2013).
In addition to T3 and T4, the thyroid has cells known as parathyroid cells that are involved in the production and hormone known as calcitonin.
Regulation of T3 and T4 is through negative feedback mechanism of the players of the hypothalamus-pituitary – thyroid axis. Excessive production of thyroid hormones leads to signals that will reduce stimulation of thyroid hormone formation. That is the cancelation of TSH and Thyrotropin Release Hormone (TRH) produced by the hypothalamus.
Disorders of the thyroid
There are two classes of disorders of the thyroid gland: hyperthyroidism and hypothyroidism. These are the two extremes of the thyroid gland. Hyperthyroidism is the condition where there are too much of thyroid hormones whereas hypothyroidism is the opposite.
Hyperthyroidism
This is a disorder characterized by the overproduction of thyroid hormones by the thyroid gland. These hormones in turn cause negative feedback to reduce the production of TSH. Hyperthyroidism may be caused by various elements and present with symptoms such as restlessness, palpitations, tremors, diarrhea, shortness of breath, skin thinning, eye problems, frequent light menstruation, swollen thyroid gland, and hair thinning. The patterns of hyperthyroidism may be influenced by patients’ factors, such as genetics, age, and gender, depending on the cause of the condition.
There are several causes of hyperthyroidism. Grave’s disease is the major cause. This is whereby the body produces antibodies that are targeted to own thyroid gland.
These antibodies bind to the TSH receptors constitutively stimulating the follicular cells to produce more of the thyroid hormones. The symptoms include swelling of the thyroid and protrusion of the eyes (proptosis). These antibodies also attack the tissue behind the eyes to loosen the eye muscle leading to double vision (Grave’s ophthalmopathy). In addition, the skin is also attacked by these antibodies leading to Grave’s dermopathy. It commonly attacks women. The age that is mostly affected is between twenty to fifty years of age. The disease can affect anyone but it mostly dwells along some familial lines thus genetics play a hand in it.
Diagnosis of grave’s disease is by use of a blood sample to test for TSH and T4. It is expected that TSH will be decreased and T4 will be elevated. The treatment includes the use of antithyroid drugs such as carbimazole and methimazole; the use of radioiodine; and thyroidectomy (Aydogan, et al, 2013).
Hyperthyroidism is also initiated by thyroid nodules. These are overgrown thyroid cells that form nodules within the gland. They do not cause serious symptoms and are mostly diagnosed accidentally. The nodules in most cases are benign in nature. Women are three times more prone to be diagnosed with these than men.
The diagnosis for thyroid nodules may either be by use of ultrasound, a blood sample to check for TSH, T4, and T3, or a fine needle aspirate (FNA). Treatment is by use of levothyroxine.
Thyroid adenoma is another cause of hyperthyroidism. This is the situation where there is neoplasm in the colloidal follicles secondary o mutation. FNA is the most efficient diagnosis of thyroid adenoma. Treatment may be surgical
Hyperthyroidism can cause adverse effects on other body systems. In the cardiovascular system, it causes increased activity such as palpitations and high oxygen use and therefore it may expose some silent disorders such as coronary heart disease.
Apart from this, hyperthyroidism can cause arterial fibrillation may occur in up to 15 % of the patients with hyperthyroidism. Here there is an enlargement of the ventricles due to hyperactivity of the heart. Hypertension occurs in one-third of elderly patients. Heart failure is also seen in most patients with hyperthyroidism.
Thyrotoxic myopathy is a disorder of the neuromuscular system that is caused by hyperthyroidism, mostly grave disease. It is a condition whereby there is general muscle weakness and breakdown of muscle tissue.
Hypothyroidism
This is a disorder characterized by little or no production of thyroid hormones. through the negative feedback mechanism, there is overproduction of TSH.
Hypothyroidism presents with symptoms such as weight gain, inability to tolerate cold, heavy irregular menses, general laziness, fatigue, memory loss, hair loss, and constipation.
The chief cause of hypothyroidism is a deficiency of iodine in the regime. This type of hypothyroidism is also known as endemic goiter and it is mainly prevalent in certain regions where the mineral is absent. In addition, an autoimmune disorder known as Hashimoto’s disease causes an influx of lymphocytes into the thyroid gland which degrades the cells. Other causes include a thyroidectomy done previously, administration of radioiodine, and neck radiotherapy. The predisposition of hypothyroidism is not inclined to any sex or age but research has shown genetics play a role in the onset of hypothyroidism.
Hypothyroidism presents with symptoms such as weight gain, inability to tolerate cold, heavy irregular menses, general laziness, fatigue, memory loss, hair loss, and constipation.
The leading cause of hypothyroidism is the absence of iodine in nutrition. This type of hypothyroidism is also known as endemic goiter and it is mainly prevalent in certain regions where the mineral is absent. In addition, an autoimmune disorder known as Hashimoto’s disease causes an influx of lymphocytes into the thyroid gland which degrades the cells. Other causes include a thyroidectomy done previously, administration of radioiodine, and neck radiotherapy. The predisposition of hypothyroidism is not inclined to any sex or age but research has shown genetics play a role in the onset of hypothyroidism. The condition can be diagnosed by the use of a blood sample whereby T3 and T4 are reduced and TSH is elevated.
Persistent hypothyroidism leads to the heart muscle filaments becoming diseased and the development of a weak heart causing heart failure. Fluid collects around the heart, a phenomenon known as pericardial effusion but seldom creates symptoms. With time this fluid causes tension in the heart leading to heart failure (Raterman et al., 2013).
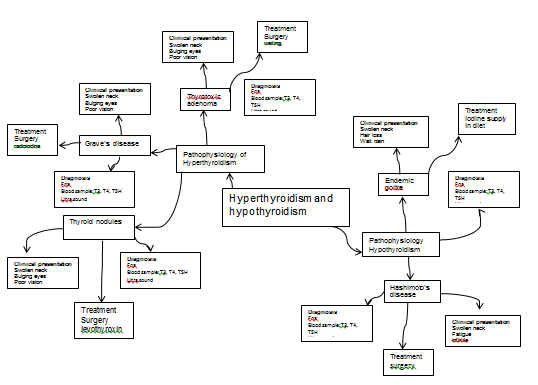
Mind map
References
Aydogan, F., Tuzcu, E. A., Aydogan, A., Akkucuk, S., Coskun, M., Ustun, I., & Gökçe, C. (2013). Effect of Radioactive Iodine Therapy on Lacrimal Gland Functions in Patients With Hyperthyroidism. Clinical nuclear medicine.
Maggi, M., Buvat, J., Corona, G., Guay, A., & Torres, L. O. (2013). Hormonal causes of male sexual dysfunctions and their management (hyperprolactinemia, thyroid disorders, GH disorders, and DHEA). The journal of sexual medicine, 10(3), 661-677.
Raterman, H. G., van Halm, V. P., Voskuyl, A. E., Simsek, S., Dijkmans, B. A. C., & Nurmohamed, M. T. (2013). Hypothyroidism and cardiovascular diseases in rheumatoid arthritis. Teva Nederland bv and UCB Pharma bv., 67(2), 229-32.
Visser, W. E., Visser, T. J., & Peeters, R. P. (2013). Thyroid disorders in older adults. Endocrinology and metabolism clinics of North America, 42(2), 287-303.