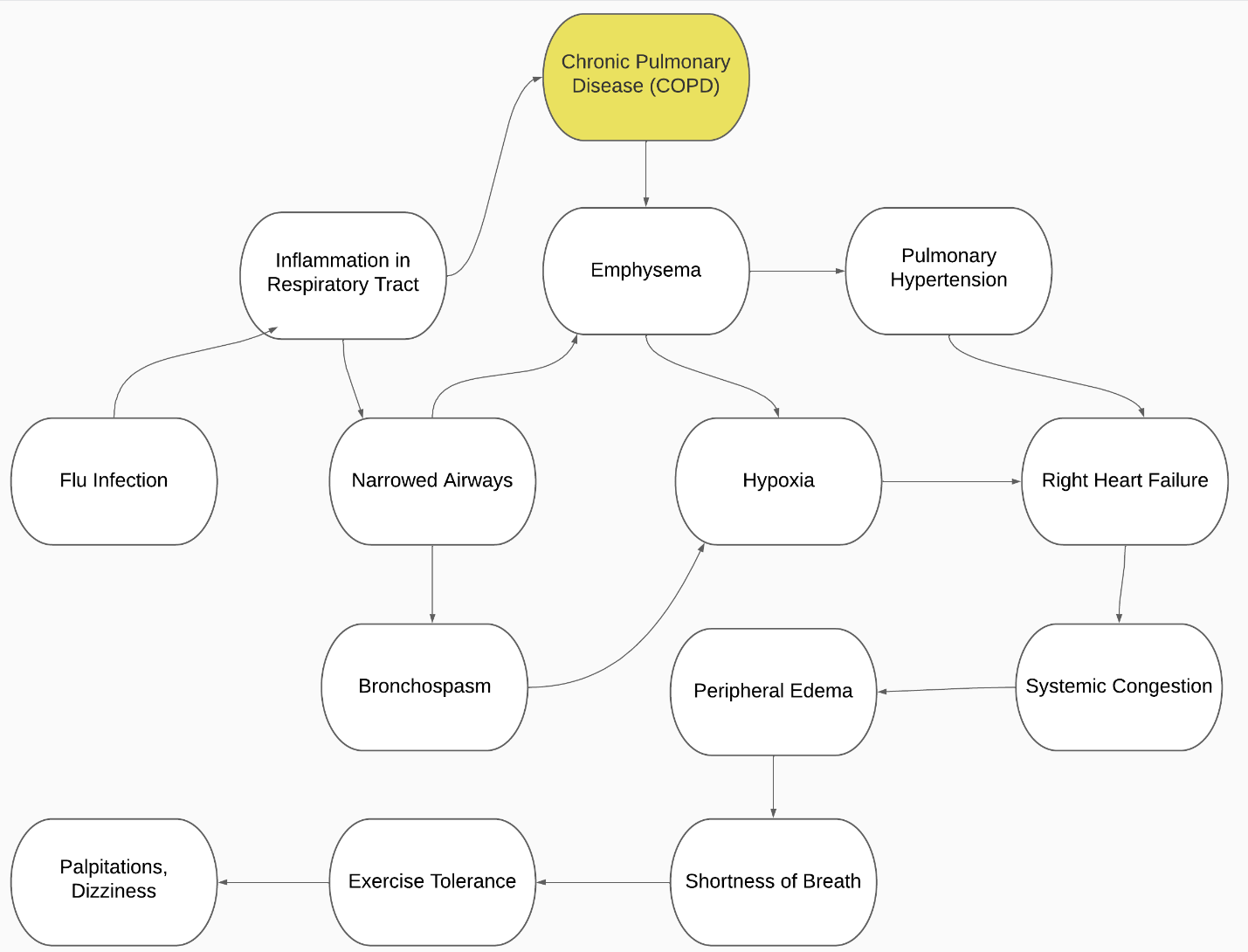
Concept Map
Elderly people have a far greater incidence of chronic obstructive pulmonary disease than people of other ages. Every year, it approaches 5-6% of the entire population over 65. (Lamb and Thomas, 2021). At the same time, negligent care, which is frequently seen at home when senior care facilities are ignored, and delayed access to medical facilities result in major consequences, including fatalities. Chronic obstructive pulmonary disease can be an indication of an innate and adaptive immunological response to repeated exposure to toxic substances, particularly cigarette smoke (Pranata et al., 2020). The degenerative alterations identified in COPD are caused by the aforementioned pathogenic processes. Physiological abnormalities are thus caused, including mucosal hypersecretion, ciliary dysfunction, airflow obstruction, hyperinflation, disorders of gas exchange, pulmonary hypertension, and systemic consequences (Lamb and Thomas, 2021).
Many facets of Beryl’s life are significantly impacted by chronic obstructive pulmonary disease, which can also lead to new illnesses (Celli & Wedzicha, 2019). Consequently, it is important to avoid long-term neglect of the primary symptoms to prevent the condition from getting worse (Duffy & Criner, 2019). Shortness of breath, coughing, wheezing, and increased mucus production became the consequences of the pathophysiological process underlying Beryl’s medical condition. Thus, lung function was impacted by such consequences, while dyspnea during exercise gradually developed into an advanced form during leisurely walking and at rest (Pranata et al., 2020). This factor has a detrimental effect on physical activity and lowers quality of life.
Case Study
In this assessment, a 65-year-old Beryl lady with chronic obstructive lung illness will be profiled (COPD). The goal of the study is to examine the issue in light of the patient’s other illnesses. When assessing the significant indicators shown in this case, the context of the newly emerging illness will be taken into consideration. Beryl’s physical condition was worsening and she was developing cardiac pathology, which is what caused her to get an acute type of pneumonia, according to an analysis of the patient’s health that took into account all of the issues. Overall, Beryl’s past medical history and current symptoms can be explained by the pathological processes that occur in the lungs, as well as the effects on the heart and systemic circulation.
The patient submitted personal information after being assessed by therapists, which may have an impact on the diagnosis and therapy. It is worthwhile to make an observation for a more thorough investigation of the disease’s course in order to weigh potential risk factors with long-term health implications. The test results revealed that the patient had a blood pressure of 163/92 and a pulse rate of 108–130 beats per minute. These out-of-the-ordinary numbers might be a sign of developing cardiac problems since they are unique (Dunican et al., 2021). No symptoms of myocardial ischemia were present. The physicians ordered an X-ray after hearing the patient’s lungs and wheezing, and they determined it was required. The patient’s lung capacity as well as inspiration and expiration, were evaluated. The breathing rate is 28 cycles per minute, which is typical.
The patient is also more susceptible to infection since she has a chronic, life-threatening form of heart disease. Due to the high burden on the heart, it can also result in early exhaustion and low activity levels in a person. Moreover, elderly individuals frequently experience immune system issues, meaning that their systems cannot carry infections like those of younger individuals (Brashers & Huether, 2019). The patient expresses worry about the progression of her lung condition and her health during conversations with doctors. The inability to spend time properly and actively due to chronic weariness considerably affects this illness. Referral to a lung support group is one sort of assistance that could be given to the patient at this time (McDonald et al., 2019). This will assist her in accepting her condition and treating it seriously as she waits for treatments.
Berry had emphysema for seven years, as can be seen from her medical background, and this has had an impact on her present situation. Reduced lung elastic recoil provides the best explanation for the pathophysiology of emphysema. Moreover, the dynamic compression of the airways during expiration is made possible by the changing connection between pleural and alveolar pressure (Duffy and Criner, 2019). During forced expiration and, in extreme circumstances, during tidal expiration, this compression limits the passage of air. Airway illness, both severe and mild, is another condition that limits airflow. Gases in the blood typically stay within the normal range or very near to it in individuals with pretty clear emphysema until the very late stages of the illness (Kumar et al., 2022). In this situation, an arterial blood gas test can assess how well her lungs remove carbon dioxide and transport oxygen into the circulation.
Uncontrolled atrial fibrillation was a crucial element in the patient’s medical history. An aberrant atrial tissue substrate that may support the arrhythmia interacts with starting stimuli, frequently quickly flaming ectopic lesions found inside one or more pulmonary veins, to cause atrial fibrillation (McDonald et al., 2021). Although many occurrences of atrial fibrillation are caused by structural heart disease, little is known about the pathophysiology of atrial fibrillation in hearts that appear to be healthy. Those who have structural heart illness and chronic or permanent atrial fibrillation may have an increased importance of abnormal substrate from atrial tissue (Brashers and Huether, 2019). To determine if additional therapy is required, a patient should have an ECG, which is the primary diagnostic for the diagnosis of atrial fibrillation.
Another symptom in Beryl’s case was bilateral pitting oedema. Its pathophysiology stems from either an increase in the intravascular space’s fluid flow into the interstitial space or a reduction in the interstitium’s water flow into capillaries or lymphatic arteries (Dunican et al., 2021). The intravascular volume reduces when fluid enters the interstitial space. The renin-angiotensin-aldosterone-vasopressin (ADH) system is triggered when intravascular volume decreases, which causes salt retention in the kidneys (Kumar et al., 2022). Sodium retention in the kidneys induces water retention and aids in maintaining plasma volume by raising osmolality. Fluid overload and edema can both be significantly attributed to increased salt retention in the kidneys (Cazzola et al., 2022). Exogenous sodium consumption in excess might potentially contribute to this. Less frequently, edema develops when there is insufficient plasma oncotic pressure, which can happen in conditions like nephrotic syndrome, protein-losing enteropathy, liver failure, or malnutrition.
Infections and damage to the capillary walls from toxins or inflammation can increase capillary permeability. Focused edema is brought on by mediators, such as bradykinin and mediators produced from complement, as well as mediators originating from mast cells (such as histamine, leukotrienes, and prostaglandins) (Anzueto & Miravitlles, 2020). White blood cells, protein, and some water are expelled from the interstitium through the lymphatic system. These chemicals build up in the interstitium as a result of lymphatic blockage. Inhibitors of sodium-glucose cotransporter 2 (SGLT2), such as canagliflozin, dapagliflozin, and empagliflozin, reduce blood sugar levels in diabetic patients while simultaneously causing diuresis by raising natriuresis without having an impact on serum electrolytes (Christenson et al., 2022). With Beryl’s additional circumstances, they are applicable to her situation.
The primary result of chronic obstructive lung disease was wheezing on expiration. From a pathophysiological standpoint, it occurs more frequently during exhale because the airways are constricted due to the higher intrathoracic pressure during this phase, and the airways are narrowed as lung capacity declines (Kumar et al., 2022). Just wheezing during expiration implies a weaker blockage. During inhaling, a whistling sound is produced by the turbulent airflow across a restricted area of the big extrathoracic airways (McDonald et al., 2019). Inhaled bronchodilators can be used to treat dyspnea on its own, such as albuterol 2.5 mg spray or 108 mcg metered dose inhalation (Anzueto & Miravitlles, 2020). In this instance, treating concomitant illnesses like chronic obstructive pulmonary disease serves as the sole effective therapy for wheezing.
Regardless of the occurrence of hyperinflation at rest, dynamic hyperinflation is frequent in the late stages of COPD and also occurs in many people with moderate illness. Because to the dyspnea, exercise intolerance, skeletal muscle limits, morbidity, and reduced levels of physical activity that are associated with COPD, hyperinflation is clinically relevant in individuals with the condition (Anzueto & Miravitlles, 2020). It has been demonstrated that a variety of pharmaceutical and non-pharmacological therapies can help COPD patients minimize hyperinflation and postpone the development of breathing limitations (Christenson et al., 2022). In order to fulfill the increased ventilation demands brought on by exercise hyperpnea, both tidal volume (VT) and respiratory rate rise.
As a result, raising pleural and alveolar pressures, increasing expiratory flow, and ensuring that the higher VT is fully expelled before the next inspiration are all necessary for maintaining stable lung volumes. Leg blood flow and physical performance during prolonged, high-intensity exercise in healthy, trained cyclists are improved by unloading the respiratory muscles with proportionate aided ventilation, demonstrating competition for blood flow between the respiratory muscles and limb muscles.
Pneumonia in older individuals frequently affects significant portions of the lungs, and many have bilateral infections as a result of a challenging diagnosis and delayed presentation to the doctor. When there are complications, total bilateral pneumonia is very deadly. Age-related oxygen deficiency increases the stress on the heart, which can cause myocarditis, arrhythmias, and acute heart failure. Pneumonia can also cause major side effects, including pulmonary edema, asthma, pleurisy, breathing issues, and persistent chest discomfort.
Antimuscarinic (anticholinergic) medicines relax bronchial smooth muscle cells by inhibiting muscarinic receptors competitively (M1, M2 and M3). Ipratropium is a short-acting anticholinergic that is administered every 4-6 hours by 2-4 injections (17 mcg/breath) (Kumar et al., 2021). Because ipratropium takes up to two hours to reach its peak impact, beta-adrenergic agonists are frequently administered alongside ipratropium in a single inhaler (Cropper et al., 2020). Alternatively, they can be administered separately as a releasing agent as necessary.
Long-acting quaternary anticholinergic tiotropium can be inhaled as a liquid inhaler (2.5 mcg/dose) or a powder inhaler (18 mcg/dose). The dosage is two inhalations (5 g) of an aerosol and one inhalation (18 g) of dry powder once day (Anzueto & Miravitlles, 2020). Aclidinium bromide is offered as a powder inhaler with several doses. Dose: 400 mcg each breath, taken once every two hours. Inhaling dry powder may work well for long-term usage when combined with aclidinium. Umeclidinium and vilanterol may be used once daily in a dry powder inhaler (a long-acting beta-agonist). Once day, revefenacin is administered using a nebulizer.
Beta-adrenergic agonists could be a better course of treatment for persons who don’t want to use powerful medications and whose symptoms largely manifest at night. Available choices are: Olodaterol, two puffs once daily at the same time each day; indacaterol, one puff (75 mcg) once per day, and salmeterol powder, one puff (50 mcg) twice daily (Cazzola et al., 2022). When used in conjunction with long-acting inhalers, vilanterol will be more efficient. For patients who have trouble using dry formulations, there are inhaled versions of arformoterol and formoterol. Analogs with a powder mode of action might be a helpful replacement when a person is unable to utilize a metered dosage inhaler adequately.
Anticholinergic medications or inhalers may help if Beryl continues to regularly have episodes of intense coughing and symptom aggravation. Unfortunately, bronchodilators may not always be able to successfully arrest the worsening of lung function and the decrease of their capacity to store air (Duffy and Kriner, 2019). The majority of the time, patients make their decision on the expense of the therapy rather than the drug’s efficacy.
To increase efficacy, Berly must be educated on how to use inhalers properly. Exercise can help her to perform better. As an illustration, she can take a deep breath in slowly and steadily until her lungs are totally filled and then hold it. 2-3 doses should be discharged prior to utilizing newly purchased or infrequently used metered dosage inhalers (Duffy and Criner, 2019). The period of usage for an inhaler can range from 3 to 14 days, and various manufacturers have varied guidelines for which inhalers can be regarded “long out of use.”
References
Anzueto, A., & Miravitlles, M. (2020). Tiotropium in chronic obstructive pulmonary disease – a review of clinical development. Respiratory Research, 21(1), 1-16. Web.
Brashers, V. & Huether, S. (2019). Alterations of pulmonary function in children. In K. McCance & S. Huether (Eds.) Pathophysiology: the biologic basis for disease in adults and children, (8th ed., pp. 1212 – 1214). Philadelphia, PA: Elsevier.
Dunican, E. M., Elicker, B. M., Henry, T., Gierada, D. S., Schiebler, M. L., Anderson, W., Barjaktarevic, I., Barr, R. G., Bleecker, E. R., Boucher, R. C., Bowler, R., Christenson, S. A., Comellas, A., Cooper, C. B., Couper, D., Criner, G. J., Dransfield, M., Doerschuk, C. M., Drummond, M. B., Hansel, N. N. & Fahy, J. V. (2021). Mucus plugs and emphysema in the pathophysiology of airflow obstruction and hypoxemia in smokers. American Journal of Respiratory and Critical Care Medicine, 203(8), 957–968. Web.
Cazzola, M., Rogliani, P., Calzetta, L., Ora, J., & Matera, M. G. (2022). A single inhaler triple therapy fluticasone furoate/umeclidinium/vilanterol for the treatment of COPD. Expert Review of Clinical Pharmacology, 15(3), 269-283. Web.
Christenson, S. A., Smith, B. M., Bafadhel, M., & Putcha, N. (2022). Chronic obstructive pulmonary disease. Lancet, 399(10342), 2227–2242. Web.
Cropper, K. J., Davis, B. E., & Cockcroft, D. W. (2020). Regular use effect of inhaled ipratropium bromide and methacholine responsiveness in well-controlled asthma. Canadian Journal of Respiratory, Critical Care, and Sleep Medicine, 5(6), 374–379. Web.
Duffy, S. P., & Criner, G. J. (2019). Chronic obstructive pulmonary disease: Evaluation and management. The Medical Clinics of North America, 103(3), 453–461. Web.
Kumar, V., Abbas, A & Aster, J. (2021). Cell injury, cell death and adaptations. In V. Kumar, A. Abbas, & J. Aster. (Eds.), Robbins and Cotran Pathologic Basis of Disease (10th ed., p. 55- 57). Philadelphia, PA: Elsevier/Saunders.
Kumar, R., Denning, D. W., & Chowdhary, A. (2022). Chronic respiratory diseases burden and healthcare facilities. Respiratory Research, 23(268), 1-12. Web.
McDonald, V. M., Maltby, S., & Penola, D. (2019). Alterations of pulmonary function across the lifespan. In J. Craft & C. Gordon (Eds.), Understanding pathophysiology – ANZ adaptation (3rd ed., pp. 743-746). Chatswood, NSW: Elsevier.
Concept Map References
Agustí, A., & Hogg, J. C. (2019). Update on the pathogenesis of chronic obstructive pulmonary disease. New England Journal of Medicine, 381(13), 1248-1256. Web.
Celli, B. R., & Wedzicha, J. A. (2019). Update on clinical aspects of chronic obstructive pulmonary disease. New England Journal of Medicine, 381(13), 1257-1266. Web.
Lumb, A., & Thomas, C. (2021). Nunn’s applied respiratory physiology (9th ed). Edinburgh: Churchill Livingstone.
Pranata, R., Soeroto, A. Y., Huang, I., Lim, M. A., Santoso, P., Permana, H., & Lukito, A. A. (2020). Effect of chronic obstructive pulmonary disease and smoking on the outcome of COVID-19. The International Journal of Tuberculosis and Lung Disease, 24(8), 838-843. Web.
Ritchie, A. I., & Wedzicha, J. A. (2020). Definition, causes, pathogenesis, and consequences of chronic obstructive pulmonary disease exacerbations. Clinics in Chest Medicine, 41(3), 421-438. Web.