Introduction
The ability to classify unidentified microorganisms is a significant part of microbiology. Knowing which of these bacteria is dangerous or not to people depends on the human ability to identify them. In biological studies and pharmacology, differentiating microorganisms is crucial. It is vital to understand the sort of microorganisms that researchers are working with. Scientists can create particular drugs or antibiotics that kill the bacteria they have by understanding what type of microbe they have. The method of recognizing unidentified microbes gets better with time as technology advances. The classical and genomic techniques are the two methods used in the laboratory. Gram staining and biochemical testing are used in the classical approach. Utilizing DNA extraction, PCR, and sequencing is the genomic technique.
The detection of bacteria is a meticulous and methodical process employing various approaches. Hence, microorganism research benefits from it in various ways and aids in providing patients with the proper management care. Gram-positive bacteria are those that have thick cell walls since they are more likely to dye during a procedure termed the Gram stain (Erickson, 2017). The Gram stain is the initial test performed to categorize microorganisms. Gram-negative bacteria are those that do not capture the Gram stain dye, such as those with thinner or absent cell walls.
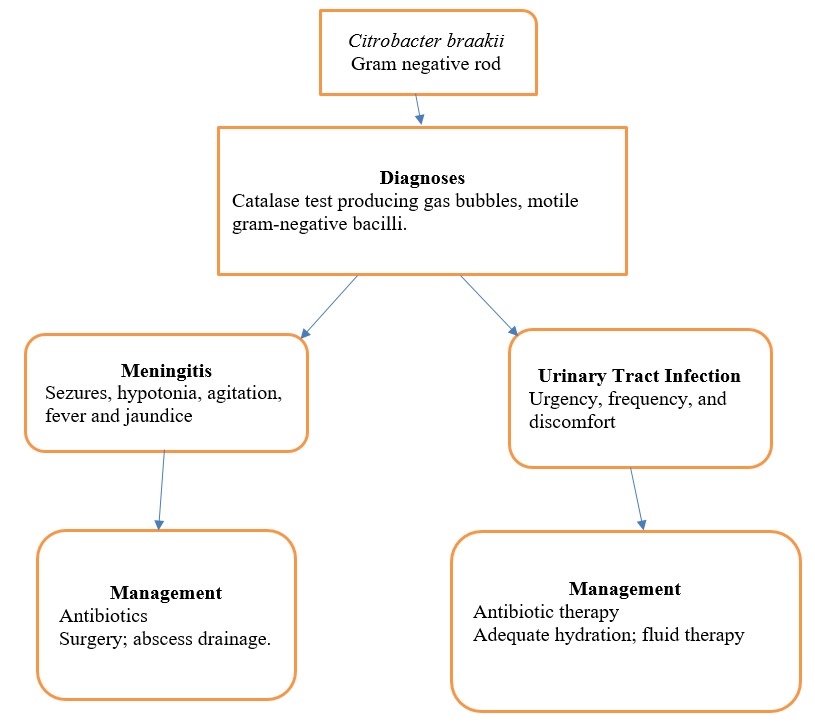
Microorganisms have distinctive traits and qualities that are used to make the most precise diagnoses. In a test, gas bubbles were seen during the catalase test, showing that the bacteria was catalase-positive. Flagella were identified to be used by the bacteria to move around. As a result, the bacteria were identified as gram-negative bacilli, with Citrobacter braakii being the most likely choice. This test shows that catalase, an enzyme that catalyzes the oxygen release from hydrogen peroxide (H2O2), is present. It is used to distinguish between bacteria that generate the catalase enzyme, like Citrobacter braakii, and those that do not, like streptococci. 15% H2O2 is typically used to identify catalase in anaerobes, whereas 3% H2O2 is generally done for the normal culture (Hossain et al., 2017). When a little inoculum of a bacterial isolate is added to hydrogen peroxide, and the quick production of oxygen bubbles takes place, it is clear that the enzyme is present.
The Organism: Citrobacter Braakii
The Enterobacteriaceae group of non-sporing rods includes members of the genus Citrobacter, which, as its name suggests, often uses citrate as its only carbon source. Gram-negative bacteria known as Citrobacter species have been linked to illnesses in immunocompromised individuals. Citrobacter species are frequently found in clinical samples from humans and animals as well as in water, food, soil, and the intestines of animals. Citrobacter infections can be acquired in the community, although most are nosocomially acquired. According to significant monitoring research, Citrobacter spp. is responsible for 0.8% of Gram-negative infections (Poonam, 2019). Citrobacter is most frequently cultured from the urinary system, frequently in conjunction with an indwelling urinary catheter, and it may be a common source of nosocomial Urinary tract infections (UTIs) and epidemics.
These pathogens may also be present in lung infections and intraabdominal diseases.
Citrobacter spp. is motile via their peritrichous flagella and emerges as rods or coccobacilli that are 0.3-1 m wide and 0.6-6 m long (Hossain et al., 2017). The genus can be split into 20 chemo groups based on the lipopolysaccharide (LPS’s) sugar content and 43 O-serogroups depending on the O antigen of the LPS. They may use citrate as their sole source of carbon and ferment mannitol to produce gaseous Hydrogen Sulfide (H2S).
Diseases
Citrobacter spp. is Gram-negative bacteria that primarily affect immunocompromised people suffering from illnesses including cancer, cirrhosis, congestive heart failure, and diabetes. They can lead to septicemia; according to prior work on the Citrobacter infections seen at a major university hospital, C. freundii (71.8%), C. koseri (23.1%), and C. braakii (3.8%) were the most frequent septicemia-causing organisms (Yumoto et al., 2017). It is known to trigger infections in the bloodstream, the respiratory system, the urinary tract, and other parts of the body that are typically healthy. The body’s functionality and poor immune system are the main causes. Sepsis, fever, seizures, lethargy, vomiting, agitation, bulging fontanelle, and jaundice are frequent presenting characteristics for newborns. Both leukocytosis and leukopenia may be visible in the white blood cell count. The majority of newborn bacterial meningitis results are associated with elevated polymorphonuclear cells in cerebrospinal fluid.
An immune system that is weak renders the body more susceptible to Citrobacter, which can lead to UTIs, intestinal infections, or meningitis. Individuals who are hospitalized, particularly those who stay there for an extended period, are much more prone to C. braakii and C. freundii infections. Respiratory tract infections (6.4%), skin and soft tissue (6.4%), surgical site (7.7%), intra-abdominal (14.1%), and urinary tract infections (52.6%), were the most prevalent forms of infection (Yumoto et al., 2017). Only three occurrences of septicemia caused by C. braakii have been documented: cervical cancer patients, peritoneal dialysis patients, and patients with lower extremity cellulitis who were all taking immunosuppressive medication.
Diagnosis
Only by culture is it possible to identify and verify people with Citrobacter infection. The species of Citrobacter may grow in a variety of culture media. All species that have been characterized as Citrobacter ferment glucose and produce gas through a catalase test. Most of the time, the microbes are mobile and use citrate. Biochemical testing can also be used to distinguish between distinct species. Antimicrobial susceptibility testing results are interpreted in accordance with the standards for Enterobacteriaceae.
Additionally, usual meningitis and sepsis signs and symptoms that also appear in other newborn infections relate to Citrobacter illness. These include fluctuating body temperature, agitation, decreased oral intake, epilepsy, jaundice, nausea, drowsiness, hypotonia, irregular gasping respirations, and a swollen fontanelle. A thorough assessment should be performed on infants who exhibit these, including blood culture, cytology, urine culture, gram staining, lumbar puncture for cerebrospinal fluid (CSF) chemistries, and culture signs and symptoms.
Treatment/Outcome
The ongoing global growth of a wide variety of -lactamases presents a challenge to successful antibiotic therapy for Citrobacter, just as it does for other Enterobacteriaceae species. B-lactam and aminoglycoside combination therapy are more effective than either drug alone in treating Citrobacter bacteremia. Only one (5.6%) of the 18 clients who got the aminoglycoside and b-lactam drug combination died, compared to five (45.5%) of the 11 clients who got third-generation cephalosporin monotherapy (Albasanz-Puig, 2021). In comparison to single-agent therapies, combined treatment was also more preventive. Thus, a b-lactam antibiotic and an aminoglycoside are chosen for the treatment of individuals with Citrobacter bacteremia. This might likely be used with additional patients with severe or intricate Citrobacter infections. Individuals with serious underlying illnesses or immunosuppressed patients with Citrobacter infestations should also consider combination therapy.
It has been observed that treating neonatal Citrobacter cerebral abscesses only with antibiotics is effective. More frequently, drainage of abscesses during surgery is combined with antibiotic therapy. Open drainage or single and multiple aspirations have been used during surgical procedures. Aspiration might not be possible if there are several abscesses present. Similar to this, conservative management might be taken into account when abscesses are difficult to extract or when they are mild and nonprogressive. When the CSF seems to be sterile, as is frequently the situation when antibiotics are administered prior to lumbar puncture, aspiration may occasionally fail to identify the causative agent.
The urinary tract system is among the most frequent sites for Citrobacter infections in adult patients. Urgency, frequency, and discomfort associated with UTI can seriously affect one’s health and may lead to dehydration. Therefore, in situations of extreme dehydration, intravenous fluids are recommended. Cotrimoxazole is the antibiotic of choice for treating UTIs since it works effectively against Citrobacter spp (Hrbacek et al., 2021). Contrary to cefotaxime, ceftazidime, and cefepime, cefuroxime is ineffective.
There are several compounds that are potent in vitro and could be utilized as alternative medicine. Fluoroquinolones may work well as an alternative to b-lactams in managing Citrobacter bacteremia in individuals who are allergic to them. Trimethoprim/sulfamethoxazole is efficient in treating meningitis brought on by Citrobacter (Hossain et al., 2017). This is a result of its intense central nervous system (CNS) penetration and enhanced intracellular phagocyte invasion. Even in individuals who did not react to prior antibiotic therapies, trimethoprim/sulfamethoxazole has been recommended as an alternate drug for managing Citrobacter meningitis/brain abscesses. Chloramphenicol has been utilized widely to treat Citrobacter meningitis and brain abscesses because it has strong CNS penetration and good action against Citrobacter (Pacifici & Marchini,2017). A newborn with Citrobacter meningitis has also been effectively treated with third-generation cephalosporins and imipenem. Surgery to drain or aspirate brain abscesses should be highly considered for people who have them.
Infants suffer substantial cerebral damage with marked retardation, hemiparesis, convulsions, and other CNS diseases. Regardless of the course of treatment, the prognosis for infants with CNS Citrobacter illness is still dismal. About one-third will die, while one-half will live but have mild to severe CNS aftereffects (Poonam et al., 2019). If outcomes are to be influenced, a considerable lot of knowledge concerning epidemiology, etiology, diagnosis, and therapeutic interventions will need to be clarified.
Conclusion
Although Citrobacter infestations are uncommon in newborns, they are strongly linked to CNS abscesses and meningitis. Infections that occur outside the CNS, excluding bacteremia or sepsis, are relatively rare. In several cases, the source of the bacteria is undetermined, although some occurrences have been proven to be nosocomial infections, while others have been demonstrated to be passed from mother to child. The latter takes place when hospital staff members have germs on their hands; in some instances, gastrointestinal tract infection has been shown. Only via culture can a person’s Citrobacter infection be detected and verified.
Citrobacter illness has same meningitis and sepsis signs and symptoms as other newborn infections. These include changes in body temperature, agitation, a reduction in oral intake, convulsions, and jaundice. Treatment for those with Citrobacter bacteremia involves a b-lactam antibiotic and an aminoglycoside. Given its potent ability to combat Citrobacter spp., cotrimoxazole is the antibiotic of preference for treating UTIs. Open drainage techniques or single- or multiple-aspiration aspirations of abscesses have been employed during surgical operations in instances of newborn meningitis.
References
Albasanz-Puig, A., Gudiol, C., Puerta-Alcalde, P., Ayaz, C. M., Machado, M., Herrera, F., Martín-Dávila P., Laporte-Amargós J., Cardozo C., Akova M., Álvarez-Uría A., Torres, D., Fortún J., García-Vidal C., Muñoz P., Bergas A., Pomares H., Mercadal S., Durà-Miralles X., García-Lerma E., Pallarès N., & Carratalà, J. (2021). Impact of the inclusion of an aminoglycoside to the initial empirical antibiotic therapy for Gram-negative bloodstream infections in hematological neutropenic patients: A propensity-matched cohort study.Antimicrobial Agents and Chemotherapy, 65(8), 1- 21.
Erickson, H. P. (2017). How bacterial cell division might cheat turgor pressure – a unified mechanism of septal division in Gram-positive and Gram-negative bacteria.BioEssays, 39(8), 1-10.
Hossain, S., Wimalasena, S. H. M. P., De Zoysa, M., & Heo, G.-J. (2017). Prevalence of Citrobacter spp. From Pet Turtles and Their Environment. Journal of Exotic Pet Medicine, 26(1), 7–12.
Hrbacek, J., Cermak, P., & Zachoval, R. (2021). Current antibiotic resistance patterns of rare uropathogens: Survey from Central European Urology Department 2011–2019. BMC Urology, 21(1), 1-10.
Pacifici, G., & Marchini, G. (2017). Clinical pharmacology of cefotaxime in neonates and infants: Effects and pharmacokinetics. International Journal of Pediatrics, 5(11), 6111-6138.
Poonam, A. R., Bilolikar, A. K., & Reddy, S. G. (2019). Prevalence and antimicrobial susceptibility pattern of Citrobacter species in various clinical samples in a tertiary care hospital.Journal of Medical and Scientific Research, 7(4), 103-108.
Yumoto, T., Kono, Y., Kawano, S., Kamoi, C., Iida, A., Nose, M., Sato, K., Ugawa, T., Okada, H., Ujike, Y., & Nakao, A. (2017). Citrobacter braakii bacteremia-induced septic shock after colonoscopy preparation with polyethylene glycol in a critically ill patient: a case report.Annals of Clinical Microbiology and Antimicrobials, 16(1), 1-4.