Summary
The Work Breakdown Structure (WBS) Checklist and the Gantt Chart are created for the Forest Hills Medical Services project. It presupposes the implementation of an early discharge education program for nurses to increase the quality of post-discharge care and reduce the number of post-operative calls. In general, timely and safe discharge indicates the quality of care in clinical settings (Coffey et al., 2019). The necessity of this intervention is determined by the fact that almost 70% of patients return to the medical facility after completing their treatment’s in-patient phase but before their next scheduled visit, even if their medical condition did not deteriorate (Liu et al., 2018). This disturbing tendency is primarily connected to a lack of information about the process of recovery provided by nurses. In addition, the combination of misinformation and anxiety typical for patients after surgical interventions leads to an increased number of post-ops calls and readmissions. In turn, when nurses occupy with patients’ calls that require the time-consuming provision of information, they cannot be appropriately involved in their main duties.
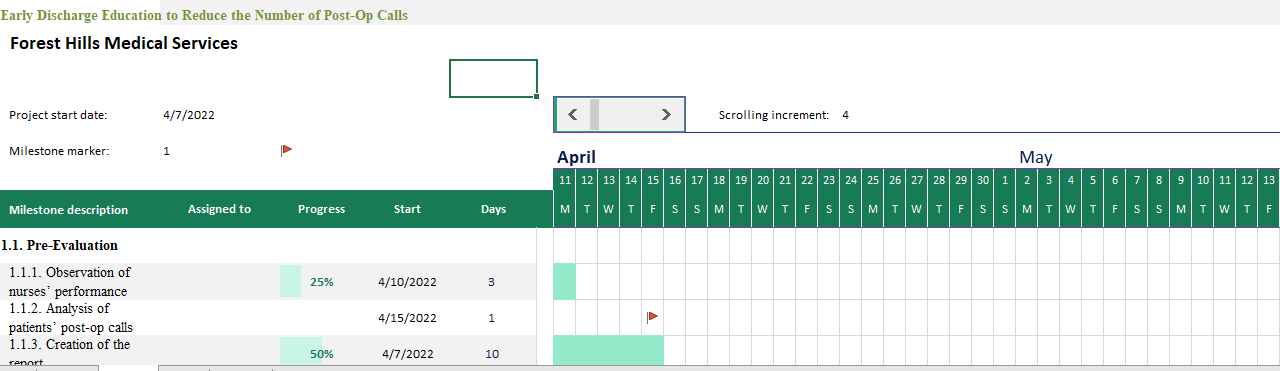
The duration of the whole project is from 3/2022 to 6/2022. The Director of Nursing, Nurse Managers, and pre-op and PACU nurses are directly involved in the intervention, while patients and their families play a supportive role. The location for the intervention is pre-op and PACU areas. Major tasks of the project include pre-evaluation, education, and post-evaluation. The duration of the first task is 30 days during 3/2022. The second task lasts 18 procedure days (Saturday and Sunday) between 4/2022 and 5/2022. The duration of the third task is 30 days, from 6/2022.
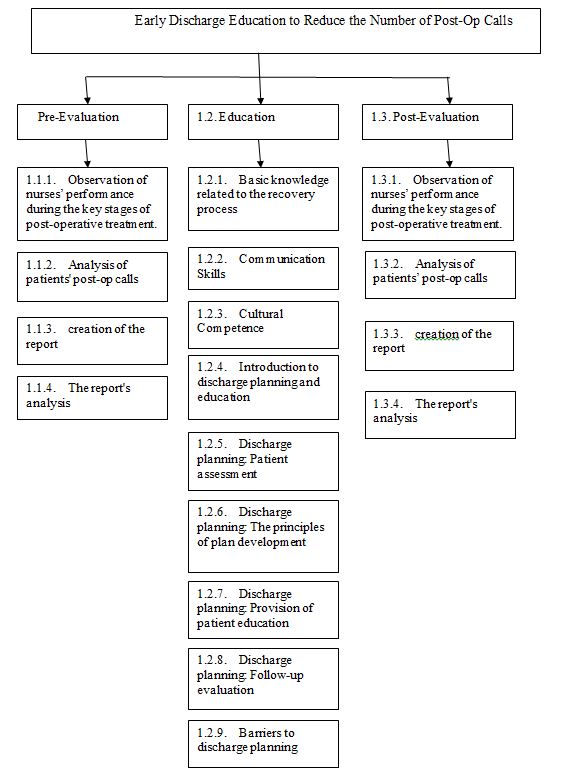
Work Breakdown Structure (WBS)
Early Discharge Education to Reduce the Number of Post-Op Calls
Pre-Evaluation
The pre-evaluation of nurses’ competencies, knowledge, and skills related to early discharge is essential for their education as it will help correct it based on initial results.
Observation of Nurses’ Performance During the Key Stages of Post-Operative Treatment
Nurse Managers are responsible for this subtask; for 25 days, they will observe nurses’ behavior during post-operative treatment. Major flaws, including poor or culturally incompetent communication, a lack or absence of information, incorrect information, and the absence of follow-up, should be identified and recorded for a final report of the intervention’s first stage.
Analysis of Patients’ Post-Op Calls
Pre- and PACU nurses should analyze post-op calls about their frequency and contents. Surgical interventions are traditionally associated with patients’ mental health issues, including stress and anxiety connected with their health, the consequences of treatment, and recovery. At the same time, it is essential to define the exact reasons that finally make the patient call the hospital. As a result, the initial factors of post-op calls will be distinguished to adapt education and increase its efficiency. The nurse will perform this subtask within 25 days when calls occur, along with the first subtask.
Creation of the Report
Nurse managers will be responsible for creating a specific report based on their observations and data collected from nurses related to post-op calls. The purpose of this report is to systematize the information available. From it, it will be clear what flaws are typical for nurses during post-operative treatment and how these flaws are subsequently reflected in patients’ concerns that lead to calls. The creation of the report should take three days.
The Report’s Analysis
During the next two days, the Director of Nursing should analyze the report and make the corrections to an educational program that is necessary to mitigate nurses’ flaws.
Education
Nurse managers will be responsible for information delivery to pre-op and PACU nurses. The program will be divided into nine parts in the format of lectures dedicated to different aspects of post-operative care. Every part will take two procedure days (Saturday and Sunday).
Basic Knowledge Related to the Recovery Process
As nurses should know how to address patients’ anxiety before they leave the premises of the hospital, they should be ready to provide reliable information related to recovery. To minimize patients’ concerns, nurses should be able to explain the difference between complications and normal post-surgical effects.
Communication Skills
Cultural Competence
These lectures will be dedicated to developing nurses’ communication skills and cultural competence that will help them provide discharge information to patients and their families more efficiently (Kang et al., 2020). Communication may be regarded as the foundation of patient discharge education.
- Introduction to discharge planning and education
- Discharge planning: Patient assessment
- Discharge planning: The principles of plan development
- Discharge planning: Provision of patient education
- Discharge planning: Follow-up evaluation
For nurses, it is essential to obtain skills related to discharge planning and education to be responsible for this process and adapt it according to a patient’s characteristics (Reddick & Holland, 2015). Pre-op and PACU nurses will learn how to communicate with patients and their families and assess their needs to mitigate concerns in the future. In addition, nurses will be provided with knowledge related to patient education techniques, including “teach-back” and the preparation of a discharge checklist for a patient (Bajorek & McElroy, 2020)
Barriers to discharge planning
Nurses will learn about major barriers to efficient discharge planning and education, including patients’ resistance, cultural differences, a lack of time or essential skills or knowledge, and ways to reduce them.
Post-Evaluation
Post-evaluation is essential for the assessment of the intervention’s efficiency, which should demonstrate the improvement of post-operative care and the reduction of the number of post-ops calls.
- Observation of nurses’ performance during the key stages of post-operative treatment.
- Analysis of patients’ post-op calls.
- Creation of the report.
- The report’s analysis.
After education, the same persons should perform the same subtasks of the pre-evaluation phase to evaluate its efficiency. Nurses’ flaws and the number of calls should be recorded for the analysis to indicate the presence or absence of positive changes.
References
Bajorek, S. A., & McElroy, V. (2020). Discharge planning and transitions of care. Patient Safety Network. Web.
Coffey, A., Leahy-Warren, P., Savage, E., Hegarty, J., Cornally, N., Day, M. R.,… & O’Caoimh, R. (2019). Interventions to promote early discharge and avoid inappropriate hospital (re) admission: A systematic review. International Journal of Environmental Research and Public Health, 16(14), 2457. Web.
Kang, E., Tobiano, G. A., Chaboyer, W., & Gillespie, B. M. (2020). Nurses’ role in delivering discharge education to general surgical patients: A qualitative study. Journal of Advanced Nursing, 76(7), 1698-1707.
Liu, X., Hu, M., Helm, J. E., Lavieri, M. S., & Skolarus, T. A. (2018). Missed opportunities in preventing hospital readmissions: Redesigning post-discharge checkup policies. Production and Operations Management, 27(12), 2226-2250.
Reddick, B., & Holland, C. (2015). Reinforcing discharge education and planning. Nursing Management, 46(5), 10-14. Web.