Hepatitis C affects the liver in humans and it is caused by Hepatitis C Virus (HCV) which has an RNA structure (World Gastroenterology Organisation, 2013). According to the National Institute of Health (2010) in the United Kingdom, individuals acquire the infection through percutaneous exposure to infected blood. Additionally, 30 percent of the infected people develop acute Hepatitis C (Goldberg & Anderson, 2004). In the event that the virus is not cleared after treatment, about 80 percent of individuals develop the chronic form of the infection (National Institute for Health and Clinical Excellence, 2010). The department of Public Health England (2013) estimates that 215,000 patients are infected with the chronic form of the disease in the United Kingdom; the prevalence of the infection in England is about 40 cases per 10,000 populations. There are variations in the ethnicity of the individuals that are infected as most infections have been reported among people of South Asian origin (Public Health England, 2013). The prevention and control strategies in England focus on the populations at-risk of the infection and majorly target injecting drug users (Public Health England, 2013). Although these strategies have been effective in the past, the cases of HVC in England are still high (Health Protection Agency, 2012). According to the Health Protection Agency (2012), the disease is projected to cause 15,840 cases of liver cancer and cirrhosis by 2020 if majority of the cases continue to be untreated. The trends between 1997 and 2008 showed that the number of patients with cancer and other HCV related complications had been increasing over the years as shown in the figure (2) below;
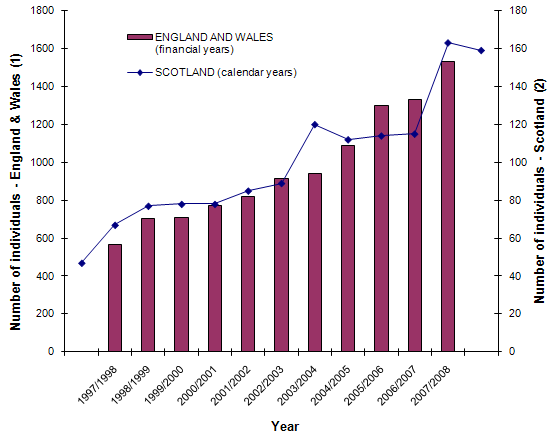
The increase in number of cases of liver cancer and cirrhosis may elicit a huge burden on the health care system in the United Kingdom and may result in many deaths (Health Protection Agency, 2012). The England Action Plan for Hepatitis C (2004) indicates that the testing should focus on the people who are most susceptible to the infection especially intravenous drug users. Based on a report by the Public Health England (2013), the prevalence of the disease among injecting drug users ranges from 17 to 82 percent and it varies across different regions in the United Kingdom.
Current prevention and control strategy in England and its effectiveness
The Public Heath England (2013), reports that England has continued to upgrade the prevention and control mechanisms that regard to hepatitis C infections. Since the control and prevention of HCV in the United Kingdom target on the susceptible populations, England has invested in effective community drug treatments that are accessible to the most-at-risk populations (Public Health England, 2013). There was an escalation of 114,855 individuals that received medication among those that abused injectable drugs between 2010 and 2011. The Drug Action Teams in the country have also developed other mechanisms for hepatitis C prevention that focus on drug misuse and sexual health (Health Protection Agency, 2012). One of the widely used control and prevention strategies is the provision of clean needles to the populations suspected of injecting drugs. This has been done through the Needle and Syringe Programmes (NSP) and it has proven to be successful over the years. In the duration between 2011 and 2012, a total of 25, 530 needles were supplied to the drug users (Health Protection Agency, 2012).
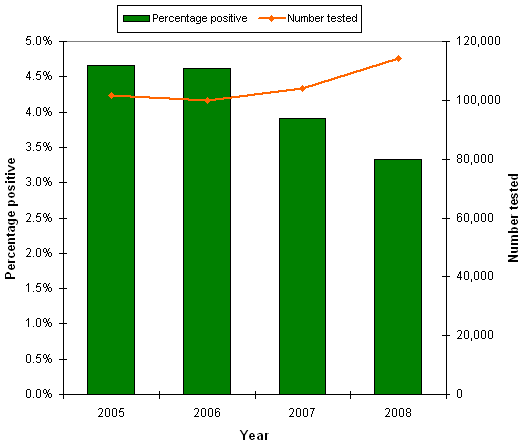
The drug users are also trained on proper use and disposal of the needles and syringes. In an effort to ensure that the Needle and Syringe Programmes are effective, peer education and outreach services are provided across the population. According to the Health Protection Agency (2012), these services are aimed at increasing the awareness of the public on hepatitis C infections. Moreover, the programmes target the populations at risk of infections with special focus on individuals of South Asian ethnicity. Another control and prevention mechanism that is in place in England is the monitoring of the testing and diagnosis patterns of the population (Public Health England, 2013). This enables the Department of Health to determine the effectiveness of the awareness campaigns and other prevention strategies that focus on the populations at risk of the infection as well as the low-risk population. In reference to the department of Public Health England (2013), there have been sentinel surveillance programs conducted to determine the number of patients tested and diagnosed with Hepatitis C throughout the country. The level of awareness on the disease has been on an increasing trend based on surveillance reports conducted between 2008 and 2012. The increasing trend was similar in the period between 2005 and 2008 as shown in figure (2).
According to the Department of Health (2004), the prevention and control strategies also include the provision of drug treatment services and drug adherence advice by specialists. These strategies also focus on the prison populations through the provision of disinfecting tablets (Department of Health, 2004). In addition to the prevention and control mechanisms that focus on the groups at risk of infections, the testing of blood donors has also been incorporated to target the low-risk population. This is important as it acts as a marker of the prevalence of Hepatitis C in the wider population. In reference to the department of Public Health England (2013), the current treatment regimens incorporate Interferon and Ribavirin which are the licensed treatments regimens in the United Kingdom. The drugs are either given in combination or as a monotherapy depending on the extent of infection and their contraindication (Public Health England, 2013).
Current challenges in the control and prevention of HCV in England
A decade after the development of Hepatitis C action plan in England, there are still several challenges that are associated with the control and prevention of the disease. According to a report by the Health Protection Agency (2012), there have been financial challenges in the procurement of the drugs used in hepatitis C treatment as they are very expensive. This incurs a high cost on both the patients and the government. Depending on the duration of the treatment required by the patients, the cost of treatment ranges from 6,246 to 12,741 pounds (Health Protection Agency, 2012). The treatment is usually prescribed for duration of 24 weeks for the genotypes 2 and 3 and 48 weeks for genotype 1 (Patruni & Nolte, 2013). This is due to the high prevalence of the infection that is still present in the population. Moreover, statistical modelling in England have projected that the number of people living with illnesses associated with lack of HCV treatment will rise to 15,840 if majority of the cases continue to be untreated (Public Health England, 2013). This is a signal that more money will be required for the management of complications such as cirrhosis and liver cancer. Additionally, the public health awareness programs in England do not seem to be 100 percent effective as the incidence of the disease continue to rise.
The lack of adherence to the drugs is another major challenge that is facing England and the rest of the United Kingdom (Hawkes, 2012). In a report commissioned by the Hepatitis C Trust in England, Hawkers (2012), indicates that the current treatment regimens are expensive and complex. Moreover, they have various side-effects that are associated with their intake such as depression, flu, and fatigue. Therefore, majority of the drug users are not well suited to such side effects and end up not following the recommended instructions when taking the treatment. More recently, protease inhibitors have been incorporated to the treatment regimens and this has made the treatment more complex and hence lack of adherence. According to the department of Public Health England (2013), lack of adherence has additional cost implication to the prevention and control of HCV as more people are likely to get infected.
Based on the report by Hawker (2012), there is also lack of consistency in the adoption of the guidelines outlined in the Hepatitis C Action Plan for England and this has had negative implication on the prevention and control strategies. The same report states that only a third of the health care providers implement the Hepatitis C guidelines to the letter. Moreover, the hospitals are characterized by delays in initiating the treatment to the patients (Hawkes, 2012). These challenges could explain why the incidence and prevalence of the disease is still high despite the prevention and control measures that are in place. In a report by the Hepatitis C trust in England, the authors note that the current control and prevention strategies are characterized by inequalities in focusing on the socially deprived population (Hepatitis C Trust, 2013). These populations include; homosexuals, the homeless, and first generation immigrants. Such inequalities are projected to cost England an additional 31 to 33 pounds annually.
Rationale for or against Introducing the New Strategy versus Relying on Current Prevention Methods
According to a report by the Health Protection Agency (2013), the current prevalence of hepatitis is estimated to be 0.5 percent which is high considering the control and prevention strategies that are currently in place. The introduction of new control and prevention strategies would require additional funding from the government (Royal College of General Practitioners, 2005). As a result, there will be additional burdens on the already strained health sector. Moreover, there have been challenges due to poor coordination among the different organs involved in the prevention and control of Hepatitis C. The current prevention strategies could be effective if there was proper coordination between the various agencies involved (Hepatitis C Trust, 2013). Therefore the government should avail more funds to ensure that the current control and prevention mechanisms are carried out efficiently. There has been a remarkable decline in the number of HCV cases in England since the implementation of the Hepatitis C Action Plan (Public Health England, 2013). This is a sign that the interventions in place have been effective and hence require additional funding to be completely effective.
The Hepatitis C Action Plan has well-defined guidelines on the conduct of public health awareness campaigns. However, the campaigns have not been effective enough to reach the overall target population (Hawkes, 2012). More comprehensive public awareness should be incorporated into the current prevention measures (Hepatitis C Trust, 2013). This would enhance the uptake of the testing programs and reduce the occurrence of the risky behaviors that act as predisposing factors to HCV. Moreover, the challenges that regard to discrimination of some populations could be solved through enhanced public awareness and re-training the health service providers (Hawkes, 2012). The comprehensive awareness campaigns should target prisoners and South Asian populations and other immigrants that comprise the at-risk population. The department of Public Health England should ensure that these campaigns are better coordinated and also target the low-risk populations (Advisory Council on the Misuse of Drugs, 2009).
The control and prevention strategy for Hepatitis C consists of guidelines that should be followed by the health service providers. However, the Hepatitis C Trust (2013) program reports that there is lack of coordination between the health workers. Some appear to follow the stipulated guidelines while others do not follow them fully (Hepatitis C Trust, 2013). The policy makers should consider re-educating all the health care providers on the treatment guidelines that are already set for HCV prevention (Health Protection Agency, 2012).This would also reduce the delays that characterize the hospitals in initiating the treatment regimes. In summary, the current Hepatitis C Action Plan for England is effective in guiding the prevention and control of HCV in England (Public Health England, 2013). Since the introduction of new preventive measures requires additional funds from the government, it is not a feasible alternative. Therefore, the current prevention strategy should be improved to make sure that the current challenges are addressed.
Perceived challenges in introducing new prevention strategies for HCV
According to the department of Public Health England (2013), it is important to review the current strategies in the prevention of HCV. Despite the guidelines outlined in the Hepatitis C Action plan, the number of cases in the country is still high (Public Health England, 2013). Additionally, the Advisory Council on the Misuse of Drugs (2009) indicates that there is a fundamental disconnect in England with regard to the effectiveness of the prevention and control of HCV and the strategies that the policy makers would like put in place. The major cause of such disconnect is the financial implications that disease has and it is projected to result in higher financial burden if more intervention strategies are incorporated. The Public Health England (2013) states that the health services in England are already financially restricted. Therefore the introduction of new preventive strategies would not be a feasible option. Moreover, introducing new prevention strategies would quadruple the current treatment costs incurred by the government at 43 million pounds per year. Therefore, the government should focus on improving the prevention and control strategies that are already in place. Additionally, there would be less people who progress to the advanced stages of the disease if effective strategies are put in place. If the government improves on the current prevention strategies, the number of patients that progress to advanced disease will be reduced to 12,000 from the current 17,000 (Hawkes, 2012). This has a likelihood of reducing the future burden of the disease in England. In summary, majority of the challenges on the introduction of new prevention strategies identify the financial burden that this would cause. Therefore, modification of the current prevention strategies would be a better option.
Resources
Advisory Council on the Misuse of Drugs. (2009). The Primary Prevention of Hepatitis C Injecting Drug Users. Web.
Department of Health. (2004). Hepatitis C Action Plan for England. London: Department of Health.
Goldberg, D., & Anderson, E. (2004). Hepatitis C: who is at risk and how do we identify them? Journal of Viral Hepatitis, 11(1), 12–18.
Hawkes, N. (2012). Confronting the Silent Epidemic: a Critical Review of Hepatitis C Management in the UK. Web.
Health Protection Agency. (2009). Health Protection Report. Web.
Health Protection Agency. (2012). Hepatitis C in the UK: 2012 Report. United Kingdom: Health Protection Agency.
Hepatitis C Trust. (2013). Hepatitis C in England: The State of the Nation. Web.
National Institute for Health and Clinical Excellence. (2010). Peginterferon Alfa and Ribavirin for the Treatment of Chronic Hepatitis C. London: National Institute for Health and Clinical Excellence.
Patruni, B., & Nolte, E. (2013). Hepatitis C: A Projection of the Healthcare and Economic Burden in the UK. Web.
Public Health England. (2013). Hepatitis C in the UK: 2013 Report. London: Public Health England.
Royal College of General Practitioners. (2005). Guidance for the Prevention, Testing, and Management of Hepatitis C in Primary Care. London: Royal College of General Practitioners.
World Gastroenterology Organisation. (2013). Diagnosis, Management and Prevention of Hepatitis C. World Gastroenterology Organisation.