Problem Statement
- 28.7% of older adults experience at lease one fall;
- At the national level, elderly people experience 29 million falls that result in 7 million injuries;
- The average cost of medical treatment for a fall is US$10,000;
- Negative consequences of falls include a temporary or permanent loss of independence and mortality;
- Since 2000, the rate of fall mortality has increased more than twofold and, today, over 27,000 of elderly individuals die every year due to a fall (Dellinger, 2017).
Falls and fall-related injuries are a common problem among elderly individuals. According to Dellinger (2017), over 1 in 4 adults, aged 65 and older, experience a fall, which equates to 28.7% of the overall older adult population. The total number of sustained falls at the country-wide level may reach up to 29 million and result in nearly 7 million injuries that require medical interventions (Dellinger, 2017). As noted by Dellinger (2017), by 2030, when the last Baby Boomers will turn 65, these numbers will increase significantly and, consequently, the healthcare costs associated with falls in the elderly will rise as well. It is also worth noticing that falls and related injuries frequently result in older adults’ loss of independence and, thus, negatively affect their quality of life. Moreover, recent statistics indicate that since 2000, the risk of mortality due to falls has increased (Dellinger, 2017). Therefore, it is essential to implement the right strategies aimed to prevent falls and fall-related injuries in the elderly and promote their well-being and longevity.
Clinical Setting Overview
GBMC manages 23,000 admissions and more than 52,000 emergency room visits every year;
- The medical center provides
- Primary/family care,
- Acute care,
- Therapy and support services,
- Cancer services,
- End-of-life care, and other services (GBMC Healthcare Inc., 2019).
Greater Baltimore Medical Center (GBMC) is a large medical center with the total number of 342 beds (GBMC Healthcare Inc., 2019). The setting renders high-quality services to diverse individuals of all ages, including older adults who may refer to GBMC’s various departments such as primary/family care, acute care, and sub-acute care. Moreover, as part of the medical center, Gilchrist works with elderly individuals who have serious illnesses, providing them with hospice care and counselling (GBMC Healthcare Inc., 2019). Considering that a significant portion of GBMC’s customers are over 65 or approaching this age, it is essential for the hospital to employ effective fall risk assessment and management techniques in order to meet the interests and needs of both hospitalized patients and those referring for outpatient treatment.
Development of a Prevention Plan
Fall Risk Factors
- Intrinsic factors:
- Advanced age;
- History of falls;
- Impaired gait, mobility, and balance;
- Impaired vision;
- Impaired cognition;
- History of stroke and Parkinson’s disease;
- Intake of psychoactive medication and polypharmacy;
- Extrinsic factors:
- Environmental hazards and risky activities (Kwan & Straus, 2014; Dellinger, 2017; Jennings et al., 2015 ).
In order to choose the right strategy for the prevention of falls in older adults, it is pivotal to understand why they occur in the first place. As stated by Kwan and Straus (2014), falls can be caused by my multiple factors at once. However, risks can be divided into two groups: extrinsic and intrinsic. The first category includes environmental conditions and activities the increase the risk of falls, whereas the second group comprises all individual characteristics including demographic features (history of falls and advanced age), sensory-neuromuscular features, balance and mobility, medications taken, and so forth (Kwan & Straus, 2014). To measure all of the described factors, practitioners should implement a set of evidence-based assessment tools.

Early Identification of Risks: Recommended Procedures
- Medical history review, patient interviews – to track history of falls and other health conditions;
- Timed Up and Go test – to asses gait and mobility;
- Functional Reach test – to assess balance;
- Medication history review, patient interviews – to track polypharmacy and use of psychoactive drugs;
- Melbourne Edge Test – to measure contrast sensitivity;
- Mental state examination – to detect cognitive impairments;
- Social history review, patient interviews – to identify any environmental hazards (Saftari & Kwon, 2018; Kwan & Straus, 2014).
Preferably, the risk assessment should address all intrinsic and extrinsic factors by using a plethora of tools, including patient history reviews, physical examinations, and other practices and tests identified on the slide. Nevertheless, it is valid to say that specific attention should be paid to the evaluation of gait and mobility. As mentioned by Kwan and Straus (2014), there are various methods to assess them, including the Timed Up and Go and the Functional Reach tests. Nevertheless, the results of a systematic review demonstrate, that the level of these tools’ predictive power may be insufficient (Kwan & Straus, 2014).
Standardized Screening Tools
- St. Thomas Risk Assessment Tool in Falling Elderly Inpatients:
- o91% sensitivity and 60% specificity;
- Prevention of Falls in the Elderly Trial:
- Comprehensive screening tools must be applied by competent practitioners who have knowledge and skills to assess all individual characteristics and combine them with appropriate methods aimed at the modification of risk factors (Kenny, Romero-Ortuno, & Kumar, 2017).
To increase risk assessment efficacy, it is recommended to utilize such standardized screening tools as the St. Thomas Risk Assessment Tool in Falling Elderly Inpatients (STRATIFY) and the Prevention of Falls in the Elderly Trial (PROFET) tool. The former test includes a range of questions aimed to evaluate a variety of risk factors, including in-hospital toileting behaviors of patients, and rate them on the scale from 0 to 10. In addition, it outlines basic actions that a nurse may undertake to reduce patients’ risks based on their assessment results. According to Kenny, Romero-Ortuno, and Kumar (2017), the STRATIFY shows 91% sensitivity and 60% specificity, which proves a significant advantage of using this instrument instead of single assessment procedures. The PROFET tool also comprises different screening components and is detailed enough. Nevertheless, it is worth noticing that “it is important that screening and assessment are applied by professionals who have the skills to deliver a comprehensive assessment coupled with modification of risk factors (i.e. cardiovascular assessment, modification of culprit medication)” (Kenny, Romero-Ortuno, & Kumar, 2017, p. 3).
Interventions for Fall Prevention
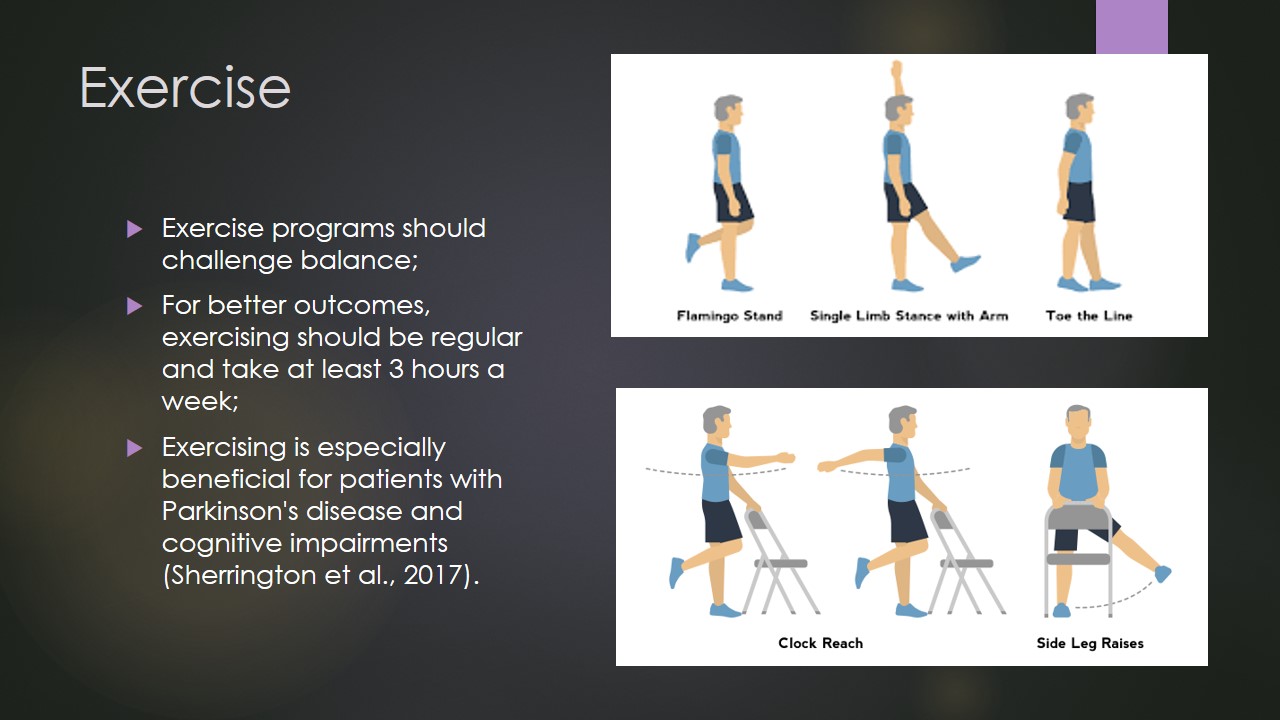
Exercise
- Exercise programs should challenge balance;
- For better outcomes, exercising should be regular and take at least 3 hours a week;
- Exercising is especially beneficial for patients with Parkinson’s disease and cognitive impairments (Sherrington et al., 2017).
Exercise programs are recognized as one of the most effective interventions for fall prevention. As the results of a systematic review by Sherrington et al. (2017) demonstrate, effective exercise programs safely involve such elements as “reducing the base of support,” “moving the centre of gravity and controlling body position while standing,” “standing without using the arms for support, or if this is not possible then aim to reduce reliance on the upper limbs” (p. 8). Noteworthily, it is observed that “exercise as a single intervention may prevent falls in people with Parkinson’s disease or cognitive impairment” (Sherrington et al., 2017, p. 8). Therefore, it may be recommended for GBMC to develop evidence-based group programs and refer to them those patients who can benefit from exercising most. For better and sustainable outcomes, patients must engage in exercising regularly (Sherrington et al., 2017). Thus, it is essential to educate patients properly regarding the benefits of physical activity.

Environment Modifications
The intervention includes:
- Personalized and contextualized assessment of injury hazards;
- Removal of tripping hazards,
- Installation of grab bars in bathrooms and toilets;
- Installation of hand rails on stairways,
- Improvement of home lighting (Wilson, Kvizhinadze, Pega, Nair, & Blakely, 2017).
Falls are likely to occur in environments that are unsafe and, thus, it is essential to remove all existing hazards. While GBMC already pays significant attention to this issue and has already installed grab bars in bathrooms and handrails on stairways, and continues to make the environment as safe as possible, similar interventions can be employed in at-risk patients’ homes. To exercise this intervention, the hospital must train occupational therapists who would carry out a personalized assessment of patients’ living areas. According to Wilson et al. (2017), environmental modifications are cost-efficient and effective in fall-related injury prevention.
Prevention of Falls in Acute Care Units
The intervention includes:
- Provision of bedside or wrist band alerts to inform healthcare practitioners about patients’ risk status;
- Patient and family education by using multiple media;
- Regular risk assessment and risk status updates;
- Provision of mobility, hearing, and vision aids to high-risk patients to minimize adverse impacts of environmental factors (Kobayashi et al., 2017; Morris & O’Riordan, 2017).
In order to increase the efficacy of fall prevention in GBMC, the following procedures should be implemented. Firstly, after the identification of a patient’s level of risks, they should be given a wrist band to alert medical staff members (Kobayashi et al., 2017). Additionally, bedside alerts/signs can be created for each patient at high risk of fall. According to Morris and O’Riordan (2017), high-risk individuals should be necessarily provided with mobility, hearing, and vision aids, such as walking frames, proper footwear, spectacles, and so forth. Such additional measures allow decreasing potential adverse effects of environmental factors.
Secondly, nurses should properly educate patients and their families and share multimedia information with them, including DVDs, pamphlets, and other handouts (Kobayashi et al., 2017). Thirdly, risk assessment for hospitalized patients must be conducted daily and changes in the status should be recorded. Moreover, it is recommended to provide patients with self-checklists and use it as an additional informational tool to track their behaviors.

Minimization of Injuries
- Vitamin D and calcium supplementation is recommended for individuals with low bone strength;
- Healthy and balanced diet is essential for maintaining bone and muscle strength;
- Hip protectors help reduce the incidence of fall-related fractures and decrease fear of falls, which allows increasing functionality and overall quality of life.
The risk of injury due to falls is elevated in individuals with such chronic conditions as osteoporosis and, therefore, vitamin D and calcium supplementation is considered to minimize the risk of fractures in them (Kwan & Straus, 2014; Kenny, Romero-Ortuno, & Kumar, 2017). Based on these findings, it is also valid to say that adequate nutrition is essential to maintain a proper level of bone strength and improve the overall physical performance of patients. Another potentially effective measure for the reduction of injuries is the use of hip protectors. As stated by Wu (n.d.), wearing hip protectors helps to reduce the fear of falling in elderly individuals, which results in improved quality of life.
Summary
Plan for falls prevention at GBMS:
- Risk assessment by using standardized, comprehensive screening tools;
- Development and implementation of personalized preventative interventions:
- Exercise programs,
- Environmental modifications,
- Patient and family education, and others;
- Injury minimization through sufficient intake of vitamins and minerals and the use of protective devices.
The plan for prevention of falls in elderly patients at GBMC includes three major steps: risk assessment, implementation of personalized interventions, and injury minimization. The utilization of standardized screening tools is preferable yet only competent nurses may use it effectively and, thus, practitioners must be either trained to provide comprehensive assessment and relevant risk factor modifications or should carry out simpler recommended procedures. Interventions suggested for both inpatient and outpatient interventions include exercise programs and environmental modifications, whereas, in the hospital, specific procedures including the creation of status alerts must be strictly followed. Lastly, in order to reduce the risk of fractures, patients should be educated to intake supplements, alter their diets, and use protective appliances. All these measures should be implemented in varying combinations to meet unique patient needs and interests.
References
Dellinger, A. (2017). Older adult falls: Effective approaches to prevention. Current Trauma Reports, 3(2), 118-123.
GBMC Healthcare Inc. (2019). About GBMC HealthCare. Web.
Jennings, L. A., Reuben, D. B., Kim, S. B., Keeler, E., Roth, C. P., Zingmond, D. S., … Ganz, D. A. (2015). Targeting a high-risk group for fall prevention: Strategies for health plans. American Journal of Managed Care, 21(9), e519-e526.
Kenny, R., Romero-Ortuno, R., & Kumar, P. (2017). Falls in older adults. Medicine, 45(1), 28-33.
Kobayashi, K., Ando, K., Inagaki, Y., Suzuki, Y., Nagao, Y., Ishiguro, N., & Imagama, S. (2017). Measures and effects on prevention of fall: The role of a fall working group at a university hospital. Nagoya Journal of Medical Science, 79(4), 497-504.
Kwan, E., & Straus, S. E. (2014). Assessment and management of falls in older people. Canadian Medical Association Journal, 186(16), E610-E621.
Morris, R., & O’Riordan, S. (2017). Prevention of falls in hospital. Clinical Medicine, 17(4), 360-362.
Saftari, L. N., & Kwon, O. S. (2018). Ageing vision and falls: A review. Journal of Physiological Anthropology, 37(1), 11.
Sherrington, C., Michaleff, Z., Fairhall, N., Tiedemann, A., Whitney, J., Cumming, R., . . . Lord, S. (2017). Exercise to prevent falls in older adults: An updated systematic review and meta-analysis. Innovation in Aging, 1(Suppl_1), 268-268.
Wilson, N., Kvizhinadze, G., Pega, F., Nair, N., & Blakely, T. (2017). Home modification to reduce falls at a health district level: Modeling health gain, health inequalities and health costs. PloS One, 12(9), e0184538.
Wu, X. (n.d.). Efficacy of hip protector in preventing fall-related hip fracture among elderly people: A literature review study. Web.