Description of Change Model
Change model used is the John Hopkins Nursing Evidence-Based Practice Process (JHNEBP).
Model uses “three-step process called PET: practice question, evidence, and translation” (Schaffer, Sandau, & Diedrick, 2013, p. 1201):
- Practice question – what is the identified research question?
- Evidence – what is the available evidence from research and non-research sources?
- Translation – is it viable for the evidence-based practice team to translate the findings into nursing practice based on existing evidence?
PICO Question
PICO Question – Will the implementation of a fall program in the orthopedic unit decrease hospital admissions and healthcare costs?
PICO Elements:
- Population
- inpatient patients in orthopedic unit.
- Intervention
- increasing number of nurses;
- increasing number of daily ward rounds;
- using fall prevention signage;
- and placing gadgets close to beds to facilitate access.
- Comparison
- no changes will be made in the number of nurses;
- daily ward rounds,
- and proximity to gadgets in the comparison/control group;
- Outcomes
- reduced hospital falls;
- reduced hospital admissions;
- reduced healthcare costs (patient and hospital).
Scope of Problem
“Injurious falls are the most prevalent in-hospital adverse event, and hospitalized patients are at a greater risk of falling than the general population” (Tzeng & Yin, 2015, p.326).
“Inpatient falls can lead to injury, prolonged hospital stays, lack of patient independence, and additional resource expense” (Tzeng & Yin, 2015, p. 326).
“In U.S. hospitals, patients with fall injuries stay in hospital an average of 6.3 days longer and their care costs $13,000 more compared with patients who do not fall during hospital stays” (Tzeng & Yin, 2015, p. 326).
Those over 75 years of age are at the greatest risk of falling.
In the U.S., “a nonfatal injury due to an unintentional fall results in an average $19,672 in hospital medical costs, placing a significant burden on individuals and society” (Tzeng & Yin, 2015, p. 327).
Lack of adequate patient monitoring in hospital environments increases the risk of falling.
“By some estimates, one million or more patient falls occur annually during hospitalization in the United States, with one-quarter or more complicated by injury” (Staggs, Mion, & Shorr, 2015, p. 983).
Units with high patient volume reports more incidences of patient falls than units with low patient volumes.
Hospitals that report more patient falls fair poorly in patient care and satisfaction outcomes, which in turn affect their reputation and ranking index in care reimbursement.
Team/Stakeholders
Team leader (Myself)
Roles include:
- guiding team members through the process of collecting evidence/data;
- overseeing the implementation of change effort.
Team members (R/N nurses in orthopedic unit)
Roles include:
- Assisting in gathering evidence;
- providing useful feedback.
Nurse leader/supervisor (orthopedic unit)
Roles include:
- providing leadership and resources;
- knowledge transfer/resource person.
Evidence supporting need for Change
Causes of Hospital Falls
- “Falls arise from multiple factors, including impaired cognition, mobility, gait, and balance; a history of falling; and dependence in daily living activities” (Tzeng & Yin, 2015, p. 326).
- Heavy nursing workload at the unit and patient levels has been associated with poor patient safety outcomes, including hospital falls (Carayon & Gurses, 2008).
- Inconsistent care delivery models increase the risk of hospital falls and other adverse outcomes in healthcare settings (Carayon & Gurses, 2008).
- Human factors (e.g., inability of nurses to routinely check on their patients) can worsen hospital falls (Carayon & Gurses, 2008).
Consequences of Hospital Falls
- Research shows that hospital falls are associated with increased hospital admissions, particularly among the elderly (Tzeng & Yin, 2015);
- Fall-related injuries experienced by inpatients in healthcare settings have been directly associated with longer hospital stay (Staggs et al., 2015);
- Research shows that fall-related injuries experienced by inpatients in healthcare settings are directly associated with increased costs through litigation, direct care costs, and poor hospital image or reputation (Staggs et al., 2015);
- “Recurrent falls result in higher mortality and likelihood of admission to a nursing facility compared with single fall events” (Lam et al., 2016, p. 1);
- Increased hospital stay as a result of falls exposes patients to other nosocomial infections and functional decline, which in turn increase the cost burdens (implications) for patients, families, and hospitals (Dunne, Gaboury, & Ashe, 2014).
Preventing Hospital Falls
- Research is consistent that “implementing research-informed fall may reduce LOS and may result in reduced hospitalization cost and, importantly, reduced burdens for patients and their families” (Dunne et al., 2014, pp. 399-400);
- In their research, Lea et al. (2012) proposes the hiring of more nursing professionals to improve patient monitoring in ward settings
- Foisy (2013) argues that using age-specific fall prevention signage, standardizing processes of care, ensuring safety at the bedside, and engaging in patient and family education could be used as effective strategies to prevent hospital falls in orthopedic unit;
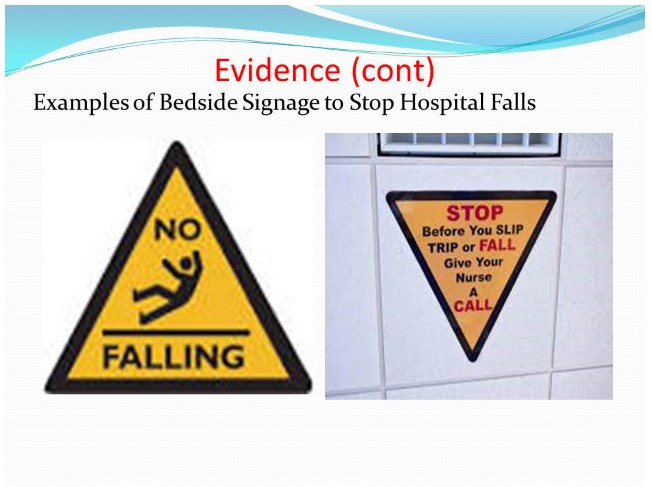
- Signage should be placed “at the head and foot of the bed to reinforce messaging for the patient, family, and staff” (Foisy, 2013, p. 248)
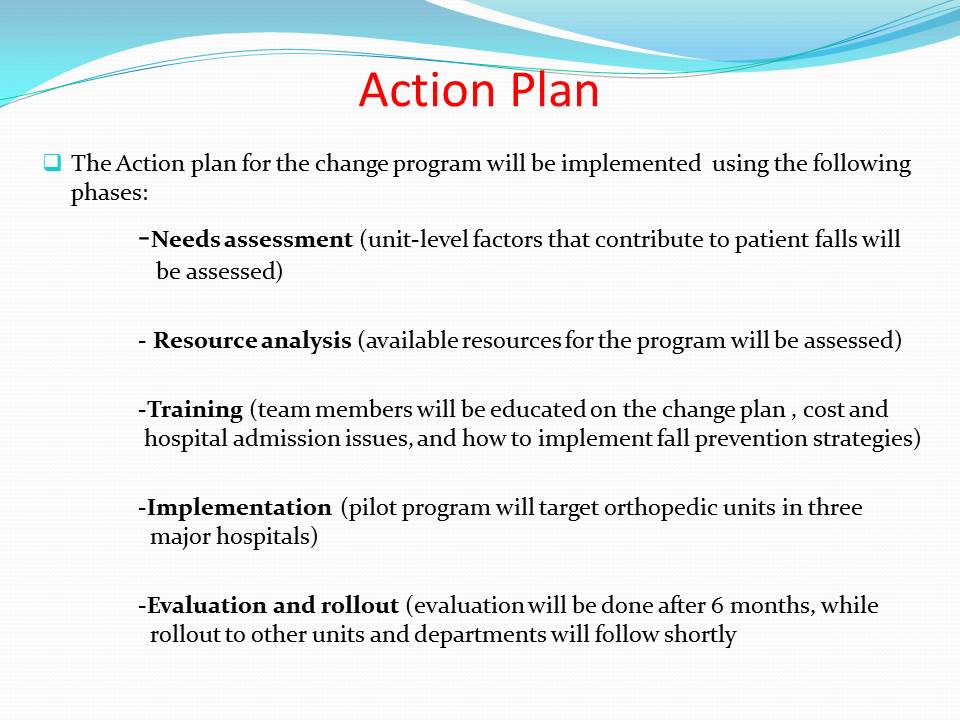
Action Plan
The Action plan for the change program will be implemented using the following phases:
- Needs assessment (unit-level factors that contribute to patient falls will be assessed);
- Resource analysis (available resources for the program will be assessed);
- Training (team members will be educated on the change plan , cost and hospital admission issues, and how to implement fall prevention strategies);
- Implementation (pilot program will target orthopedic units in three major hospitals);
- Evaluation and rollout (evaluation will be done after 6 months, while rollout to other units and departments will follow shortly.
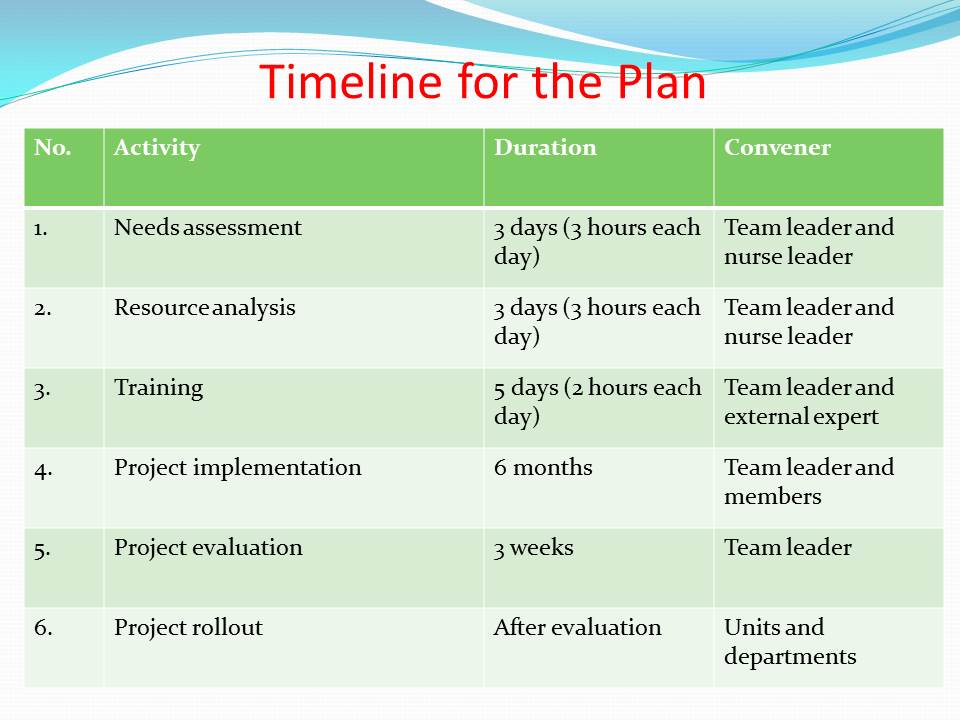
Timeline for the Plan
Nurse’s Role & Responsibility
- Guiding team members through the process of collecting evidence/data;
- Overseeing the implementation of the change plan;
- Ensuring that effective indicators are established to measure the effects of interventions;
- Liaising with nurse leader on logistical issues, funding, human resources, and other inputs;
- Ensuring that team members develop the adequate knowledge and skills needed to implement the project;
- Undertaking project evaluation to inform practice and future directions.
Procedures
- Increasing the number of nurses in selected orthopedic units to reduce nurse workload;
- Increasing the number of daily ward routines to reduce the possibility of human factors contributing to hospital falls;
- Placing gadgets close to patient beds to ensure easy access;
- Placing fall prevention signage on patient beds and other risky areas to caution patients, family members, and staff;
- Researcher will evaluate changes (pre- and post-intervention) in terms of the number of hospital admissions due to falls; amount of money paid by the patient due to patient falls; and amount of money paid by the hospital or unit due to patient falls.
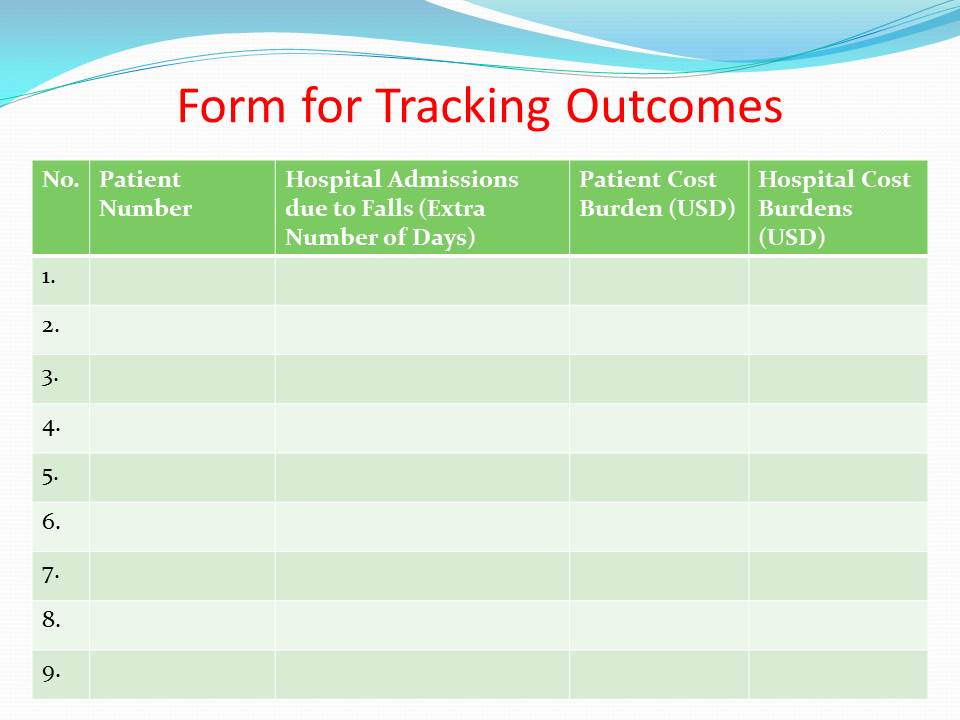
Form for Tracking Outcomes
Resources Available to Staff
- Human resources (team members) to undertake the change project;
- External expert on hospital falls prevention to train team members;
- Internet resources for ease of communication and to facilitate research;
- A van to transport team members to the selected orthopedic units;
- Nurse investigator (team leaders) to lead the change effort;
- Data analysis software to analyze and interpret intervention data.
Summary
Hospital falls continue to cause many adverse outcomes not only to patients, but also to healthcare organizations and other stakeholders in the health sector.
The main purpose of this change plan is to reduce fall-related hospital admissions and healthcare costs (patient and hospital by implementing the targeted interventions; the research question is whether the implementation of a fall program in the orthopedic unit will decrease hospital admissions and healthcare costs?
Planned interventions include:
- increasing number of nurses,
- increasing number of daily ward rounds,
- placing gadgets close to the bed to facilitate access,
- using fall prevention signage to caution patients, family members, and staff.
The measurable outcomes for the project include:
- rate of hospital admissions due to falls,
- patient cost burdens due to falls,
- hospital cost burdens due to falls.
References
Carayon, P., & Gurses, A.P. (2008). Nursing workload and patient safety – A human factors engineering perspective. In R.G. Hughes (Ed.), Patient safety and quality: An evidence-based handbook for nurses (pp. 322-357). Rockville, MD: Agency for Healthcare Research and Quality.
Dunne, T.J., Gaboury, I., & Ashe, M.C. (2014). Falls in hospital increase length of stay regardless of degree of harm. Journal of Evaluation in Clinical Practice, 20, 396-400.
Foisy, K. (2013). Though shalt not fall! Decreasing falls in the postoperative orthopedic patient with a femoral nerve block. MEDSURG Nursing, 22, 246-249. Web.
Lam, C., Kang, J.H., Lin, H.Y., Huang, H.C., Wu, C., & Chen, P.L. (2016). First fall-related injuries requiring hospitalization increase the risk of recurrent injurious falls: A nationwide cohort study in Taiwan. PLoS ONE, 11(2), 1-15.
Lea, E., Andrews, S., Hill, K., Haines, T., Nitz, J., Haralambous, B.,…Robinson, A. (2012). Beyond the ‘tick and flick’: Facilitating best practice falls prevention through an action research approach. Journal of Clinical Nursing, 21, 1896-1905.
Schaffer, M.A., Sandau, K.E., & Diedrick, L. (2013). Evidence-based practice models for organizational change: Overview and practical applications. Journal of Advanced Nursing, 69, 1197-1209.
Staggs, V.S., Mion, L.C., & Shorr, R.I. (2015). Consistent differences in medical unit fall rates: Implications for research and practice. Journal of the American Geriatrics Society, 63, 983-987.
Tzeng, H.M., & Yin, C.Y. (2015). Patient engagement in hospital fall prevention. Nursing Economic$, 33, 326-334. Web.