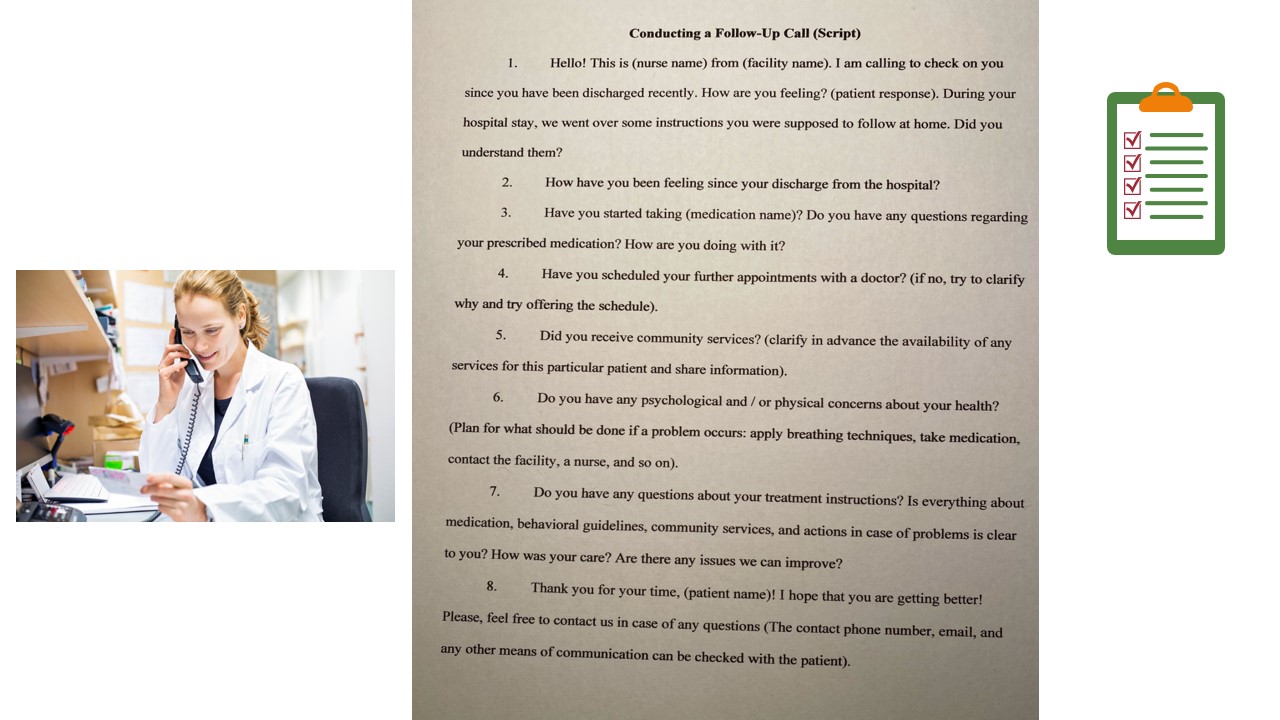
This is my capstone project that explores the Follow-Up Calls Post Discharge to Reduce Frequent Readmission in a Psychiatric Unit. The project includes the problem identification, critical literature review, and practical nursing intervention, which results in a unique questionnaire –guidance for nurses to make calls.
Introduction and Problem
- A lack of communication and poor discharge guidelines = hospital readmissions;
- 10-15% of patients are readmitted within 30 days, the majority of them return within 2-3 days;
- Average cost for readmission in 2016 -$14,400;
- The Newark Beth Israel Medical Center: rate of readmission:
- o2.5% (July 2018 – June 2019);
- o3.4% (July 2019 – January 2020).
A post-discharge period is the most threatening since high readmission rates can be listed among the most critical problems that are faced by psychiatric units. This problem is closely associated with poor discharge instructions, a lack of communication between care providers and patients, low awareness of available community services, and failure to follow the recommendations. The data presented on the slide shows that many patients have to return to the Newark Beth Israel Medical Center, which sets additional financial and healthcare burden.
Nature of the Project and Research Question
Purpose: To provide the foundation for implementing follow-up calls to the discharged patients.
Lewin’s change theory: Unfreezing, change, and refreezing.
Lewin’s theory: Explain implications, implement, and measure the results.
Research question: Will hospital readmission rates be reduced in patients who were discharged from a psychiatric unit after the implementation of follow-up calls as a part of outpatient care as opposed to those who did not receive calls?
This project aims to propose the implementation of follow-up calls to discharged patients, which are not conducted at the Newark Beth Israel Medical Center now. Lewin’s change theory is used as the theoretical framework to guide the literature review and make relevant conclusions. The research question is presented on the slide.
Literature Review: Historical Overview
The 1800s: Patients with mental disorders were isolated from society in asylums;
19th century: Emil Kraepelin introduced the concepts of neuropsycholo-gy and neurology;
1963: The deinstitutionali-zation of asylums and administration of the Community Mental Health Centers;
Since 2000: Reducing the number of hospital beds and promoting outpatient community services.
Historically, people having mental issues were to be isolated in asylums to hide them from society. With time, research and practice changes their treatment, and the Community Mental Health Centers appeared. However, no post-discharge services were provided to patients. Within the last two decades, the long-term rehabilitation of patients was regarded as the state-of-the-art approach to treating patients. The continuity of care was recognized as an essential change that could significantly improve patient outcomes.
Literature Review: Current Findings
- Patients try to manage post-discharge issues by social withdrawal, substance use, and self-injury;
- 59.1% of compulsory admission and 46.7% of voluntary admission patients were readmitted within a 7-year period;
- Follow-up calls = interpersonal support and assertive outpatient treatment.
The current evidence shows that patients need assistance to handle post-discharge problems, which especially pertinent to those who were admitted compulsorily. According to Bath et al. (2019), a callback program has a great potential to reduce readmission rates due to necessary guidance on medication and outpatient instructions in general. The use of call programs includes such advantages as interpersonal support provision, patient feedback, better understanding of psychiatric care drawbacks, and care continuity.
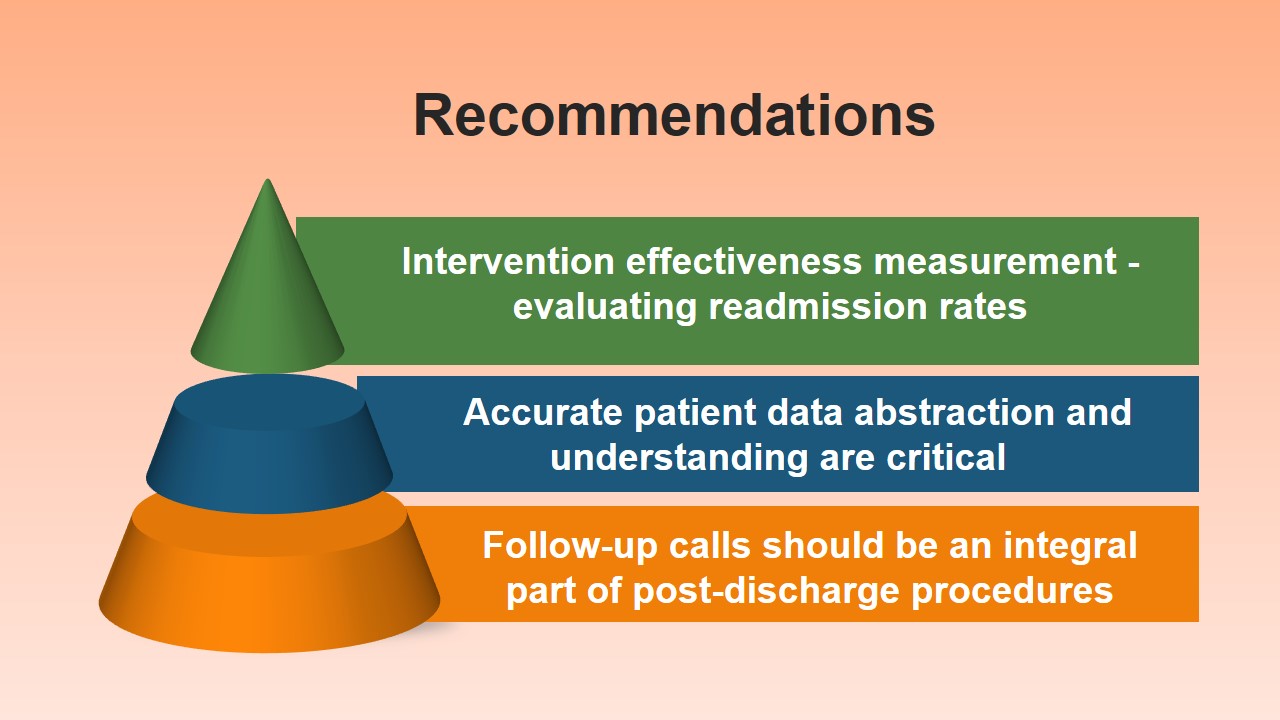
Recommendations
- Intervention effectiveness measurement -evaluating readmission rates;
- Accurate patient data abstraction and understanding are critical;
- Follow-up calls should be an integral part of post-discharge procedures.
Based on the literature review findings, the key recommendations is to integrate follow-up calls in post-discharge procedures. It is better to assign 2-3 nurses with the task of preparing and performing these calls. Also, readmission rates in pre- and post-intervention periods should be used as a measure of understanding the effectiveness of calls to patients.
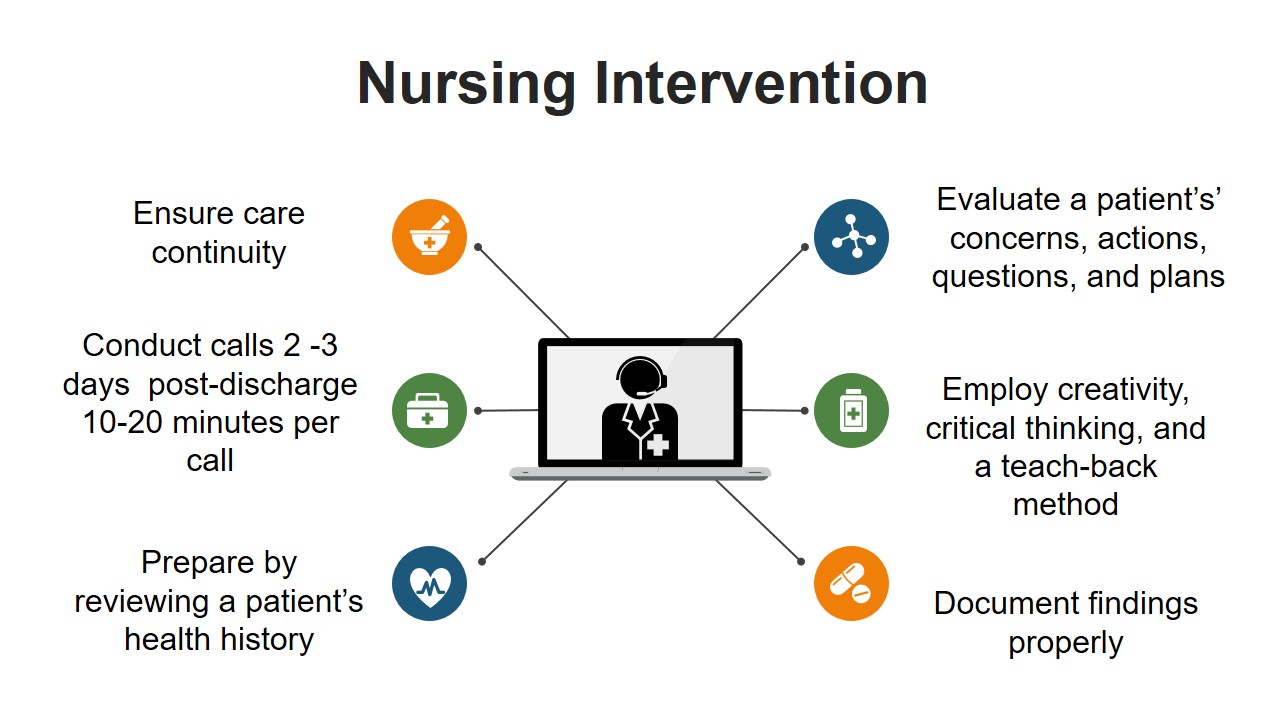
Nursing Intervention
- Ensure care continuity;
- Conduct calls 2 -3 days post-discharge 10-20 minutes per call;
- Prepare by reviewing a patient’s health history;
- Evaluate a patient’s’ concerns, actions, questions, and plans;
- Employ creativity, critical thinking, and a teach-back method;
- Document findings properly.
The first step of the nursing intervention is to review a patient’s health history and notice the key challenges that may be related to him or her. If necessary, the discharge team can be contacted and asked questions to clarify any inconsistencies. The second step is calling to a patient and making sure that he or she understands the questions, being aware of the need to follow the discharge instructions. The key aspects to ask about are a health status, appointments, medicine check, community service coordination, and further plans.
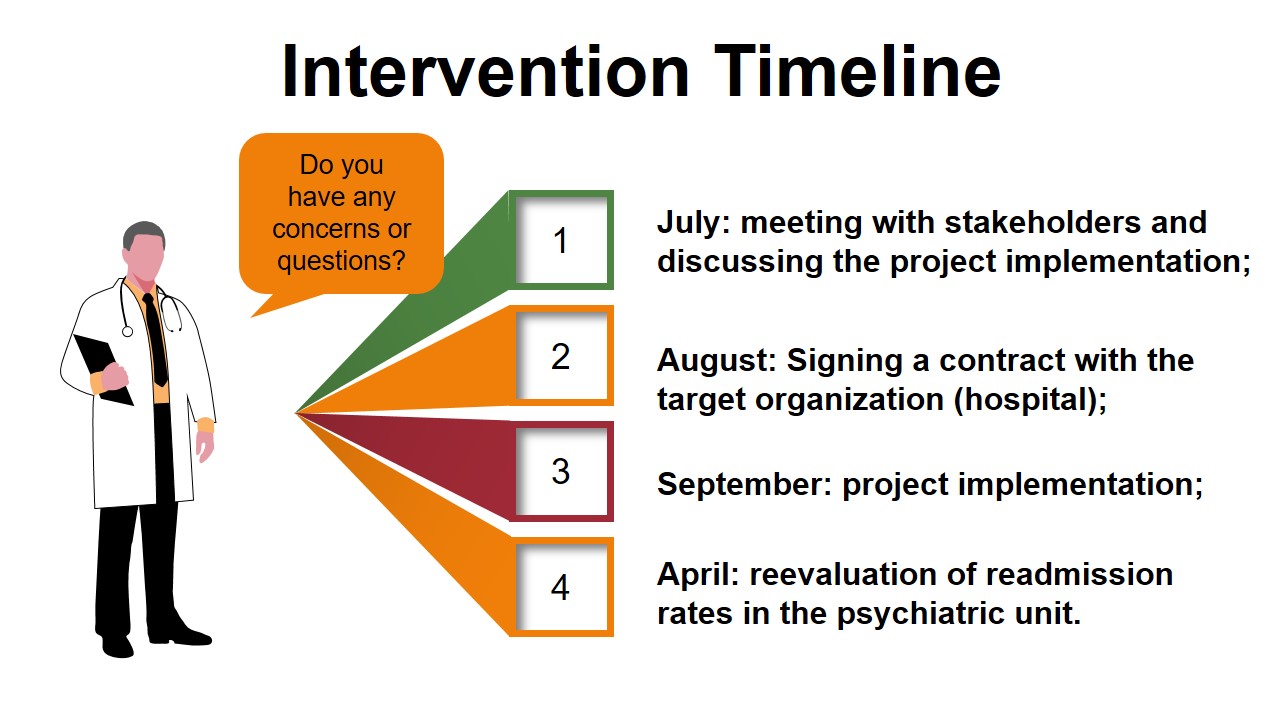
Intervention Timeline
- July: meeting with stakeholders and discussing the project implementation;
- August: Signing a contract with the target organization (hospital);
- September: project implementation;
- April: reevaluation of readmission rates in the psychiatric unit.
References
Barker, L. C., Gruneir, A., Fung, K., Herrmann, N., Kurdyak, P., Lin, E., & Vigod, S. N. (2018). Predicting psychiatric readmission: Sex-specific models to predict 30-day readmission following acute psychiatric hospitalization. Social Psychiatry and Psychiatric Epidemiology, 53(2), 139-149. Web.
Bath, J., Freeman, D., Salamoun, M., Harvey, E., Wright, A., Hamill, M., & Collier, B. (2019). Decreasing trauma readmission rates by implementing a callback program. Journal of Trauma Nursing, 26(1), 33-40. Web.
Duhig, M., Gunasekara, I., & Patterson, S. (2017). Understanding readmission to psychiatric hospital in Australia from the service users’ perspective: A qualitative study. Health & Social Care in the Community, 25(1), 75-82. Web.
Hengartner, M. P., Klauser, M., Heim, G., Passalacqua, S., Andreae, A., Rössler, W., & Von Wyle, A. (2017). Introduction of a psychosocial post‐discharge intervention program aimed at reducing psychiatric rehospitalization rates and at improving mental health and functioning. Perspectives in Psychiatric Care, 53(1), 10-15. Web.
Lin, C. E., Chung, C. H., Chen, L. F., Chen, P. C., Cheng, H. Y., & Chien, W. C. (2019). Compulsory admission is associated with an increased risk of readmission in patients with schizophrenia: A 7-year, population-based, retrospective cohort study. Social Psychiatry and Psychiatric Epidemiology, 54(2), 243-253. Web.
Peter, D., Robinson, P., Jordan, M., Lawrence, S., Casey, K., & Salas-Lopez, D. (2015). Reducing readmissions using teach-back: Enhancing patient and family education. JONA: The Journal of Nursing Administration, 45(1), 35-42. Web.
Wojciechowski, E., Pearsall, T., Murphy, P., & French, E. (2016). A case review: Integrating Lewin’s theory with lean’s system approach for change. Online Journal of Issues in Nursing, 21(2). Web.
Zheng, S., Hanchate, A., & Shwartz, M. (2019). One-year costs of medical admissions with and without a 30-day readmission and enhanced risk adjustment. BMC Health Services Research, 19(1), 155-165. Web.