Background on Frontotemporal Dementia
Frontotemporal Dementia is characterized by degeneration of the frontal lobe which lead to behavior and executive function changes. Researchers consider that hereditary factors are important in the etiology of Frontotemporal Dementia. The matter has been continuously investigated ever since. These investigations showed that children adopted away from their biological parents at birth are at significantly greater risk of later developing Frontotemporal Dementia if there is dementia among their biological relatives, but not if it is present among their adoptive relatives (Baddeley et al, p. 98). These findings demonstrate that the enhanced tendency to develop Frontotemporal Dementia in these people is not due to a shared environment but to shared genetic material. “One of the major criteria used for distinguishing frontal variant dementia is the existence of executive deficits as shown by performance on frontal tasks” (Ward, p. 120). The boundary between normality and Frontotemporal Dementia is not clear-cut. It has been known for a long time that abnormal features can be observed before the onset of a clear-cut psychotic episode, and so it has generally been assumed that these transient or partial forms would always evolve into clear-cut and sustained psychotic features. However, this is not always the case.
The theme of the relationship of mental disorder to brain abnormality (neuropathology) was pursued in a particularly successful way in relation to what we would now recognize as neurosyphilis (then termed general paralysis of the insane). This was shown to be a single disease that presented as a sequence of clinical syndromes. “Recent studies in the literature claim to meet this criteria if performance is impaired on several such tasks, e.g. Trails version B and the Stroop. Lough, Gregory, and Hodges (2001) presumably defined their sample of frontal variant patients some other way since they were described as having intact performance on executive tasks but an inability to perform “theory of mind” problems” (Ward, p. 120). The order of appearance of these syndromes depended on the progress of lesions in the brain. Neuropathological approaches to dementia were also successful. Dementia praecox had a specific pathology in the brain and a specific cause, even though essentially nothing was known of either the pathology or the cause during his lifetime. The symptoms that he emphasized included auditory and tactile hallucinations, delusions, incoherent speech, blunted emotions, negativism (resisting suggestions and doing the opposite), stereotyped behavior, and lack of insight. Nonetheless, he appreciated that the condition was diverse and difficult to classify (Baddeley et al, p.98).
Overall Question
The question is whether executive deficits are the main signs and medical manifestations of Frontotemporal Dementia. The goals of the experiment is to extend the studies and differentiate between Alzheimer’s disease and Frontotemporal Dementia.
Alternatives and Logic
The hypothesis to be tested is based on the idea that executive deficits is a remarkable feature of Frontotemporal Dementia rather than Alzheimer’s disease. The concept of Frontotemporal Dementia as an essentially psychological and physical disorder, possibly with a psychogenic basis, rather than a pathological condition of the nervous system is attractive to psychiatrists. This view fitted in well with the psychoanalytical tradition that prevailed. As a result, psychiatrists had a very broad concept of Frontotemporal Dementia, one that included patients who would have been regarded as having depressive or manic psychoses, or even as suffering from non-psychotic neurotic states (Garrison, p. 781).
Method
The theory of mind will be used to test the hypothesis. It is assumed that some events happen to one person remain unaware for another person during the experiment. Theory of mind suggests that patients with Frontotemporal Dementia will be unable to perceive and understand events while another person (a testee) will be able to identify and explain the event. It is suggested that executive functions are distinct and disconnected but in some patients they can be associated with adjacent parts of the frontal lobes. From within the broad class of illnesses not associated with a demonstrable underlying brain lesion, he had set out to define a cluster of symptoms and signs that predicted a characteristically poor outcome. It is expected to test 25 patients (20-50 years old) with Frontotemporal Dementia. A special attention and care will be paid to possible cases of Alzheimer’s disease. The control group will consist of 25 people (from 20—50 years) without psychological problems.
Anticipated Results
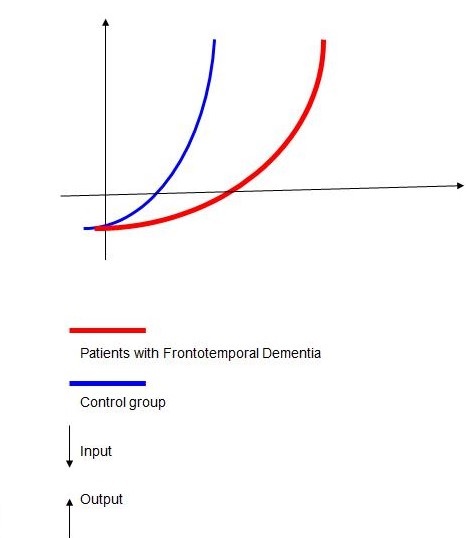
One test of executive function on which patients with Frontotemporal Dementia often perform badly is ‘verbal fluency’, particularly in the form where the patient has to give all the words she can think of beginning with the letter A (or S, or F). the executive processes located in the prefrontal cortex can be seen as being near the top of a hierarchy of control. The executive processes control the function of lower centers located in posterior regions of the brain. The researcher will present a list of words and then asking patients to repeat back the words a few minutes later. This is a typical memory test. Researchers could just listen passively to the words and hope that we will remember them. Researchers could repeat the words over and over in our heads, but the psychologist will probably prevent this by giving another task to distract us. The best way to remember a list of words is to think about what the words mean. The patient with ‘executive problems’ fails to use strategies like this when trying to remember a list of words, and as a result, her memory for the words is poor. If she is specifically instructed to use a good strategy, her memory improves (Stuss and Levine, p. 401).
It is clear that problems with executive functions will have a pervasive effect on the performance of a whole range of tasks. For almost any task there will be an optimum strategy that could be adopted, including, of course, the strategy of abandoning the task altogether because enough time has been spent on it or it is too difficult. Tasks that depend least on executive functions are those that have been well practiced so that optimum strategy is adopted as a matter of routine. Alternatively, the need for executive functions is minimized if the experimenter tells the subject precisely how the task should be performed and which strategy should be adopted. On tasks like this patients with Frontotemporal Dementia perform reasonably well. The results obtained from the experimental and control groups will be compared (Stuss and Levine 401). It is also suggested that these ‘lesser’ executive functions superficially resembling Frontotemporal Dementia but with a good outcome should be considered ‘psychological’ rather than ‘physical’ disorders – in other words, these disorders do not have abnormalities in the brain and are appropriately treated with psychotherapy.
Inferences
The obtained results will prove that executive functions depend upon the prefrontal cortex. Different aspects of executive functioning probably rely upon different regions of prefrontal cortex, although precise relationships are yet to be determined (Selkoe, p. 58). Once a suitable strategy has been selected by processes acting in the prefrontal cortex, it will be implemented in posterior parts of the brain. For example, the word store that must be accessed in a verbal fluency task is probably located in the left temporal cortex. Thus, the executive processes located in the prefrontal cortex can be seen as being near the top of a hierarchy of control. The executive processes control the function of lower centers located in posterior regions of the brain. In patients with known brain lesions, impairment of executive function is associated with lesions in the frontal lobe, although these often have to be quite large for the impairment to be detected using standard neuropsychological tests. If executive function depends not only on the prefrontal cortex but also on interactions between the prefrontal cortex and other brain regions, then problems could arise if something went wrong with these interactions (Maj and Sartorius 109). The interactions depend upon long-range connections between brain regions and also on loops involving structures beneath the cortex, such as the basal ganglia. This problem frequently occurs with patients who are seriously ill, since a severe mental illness can cause a breakdown in family relationships. Sometimes, for reasons related to stigma, family history is concealed from doctors, and indeed we have come across cases where the family history is concealed from some family members. Since modern methods of genetic research were developed, these have been applied with enthusiasm to the study of psychiatric disorders (Garrison, p. 781).
Works Cited
- Baddeley, A.D., Kopelman, M. D., Wilson, B. A. The Handbook of Memory Disorders. Wiley, 2002.
- Garrison, M, The Empire of Illness: Competence and Coercion in Health-Care Decision Making. William and Mary Law Review, 49 (2007), 781.
- Maj, M., Sartorius, N. Dementia. Wiley, 2002.
- Selkoe, D. T. The Aging Mind: Deciphering Alzheimer’s Disease & Its Antecedents. Daedalus, 135 (2006), 58.
- Stuss, D. T., Levine, B. Adult Clinical Neuropsychology: Lessons from Studies of the Frontal Lobes. Annual Review of Psychology, 2002, p. 401.
- Ward, A. Attention: A Neuropsychological Perspective. Psychology Press, 2004.