The national scorecard on the state of the U.S Health system consisted of an audit into the performance of the system. The 2008 scorecard was used to assess the condition of healthcare in terms of quality, accessibility, and impact as well as equality in its availability. The parameters however indicated a minimal improvement from the previous 2006 results. In 2008 the commonwealth fund commission received the report that showed achievements just above sixty percent. The report pointed out that the major areas of poor performance included healthcare access and the level of mortality in the U.S. According to the scorecard, data on the metrics used shows an overall decline from the expected including aspects of efficient delivery and healthy living.
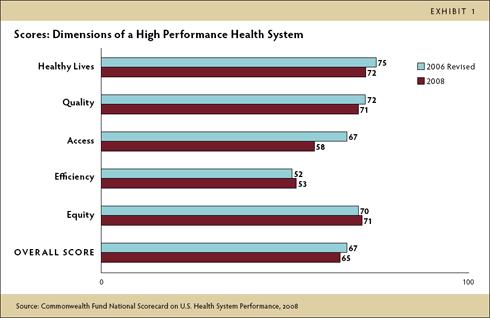
The report further outlined the scores for each parameter with the areas of quality and equity attaining a 71 percent score while the healthy living was ranked at 72 percent (The Commonwealth Fund Commission on a High-Performance Health System, 2008). The objective of this research is to analyze the results based on findings in the area of Health care quality, access, and efficiency. The study will focus on these areas as they are related to issues that are prevalent in current health policies. Moreover, aspects such as quality and access play a major role in determining the performance of any healthcare system. For instance, studies of the current policy show that the system is facing challenges in areas of funding, equity, and access due to the competition between players in the private and public sectors. In addition, the system has been found to be inefficient with problems being encountered in administration and medical insurance (Garson, 2010). This implies that challenges noted in the 2008 national scorecard on health are relevant for the current system.
Quality
The national health system scorecard involved an examination of quality in various areas. The report looked into the safety of care, efficiency, coordination as well as timeliness. Recent studies have shown that healthcare quality contributes majorly to a successful system. This is due to the attention paid to creating good relationships between physicians and their clients. There has been an increased need to improve quality to lower healthcare costs. For instance, the safety of healthcare provided is can be easily assessed from the rate of mortality that is related to mistakes. Moreover, the number of emergency cases connected to drug intake is a show of safety as part of quality. Quality is a metric that has been introduced lately in health studies (McLaughlin & McLaughlin, 2008).
Effectiveness on the other hand is indicated by the ability to manage chronic and terminal illnesses such as diabetes and high blood pressure. These are particularly important as the two diseases are on the rise among populations today. Research shows that an estimated 215,000 people aged 20 and below had diabetes in the year 2010 (National Diabetes Information Clearing House, 2011). For example, medical centers were evaluated on basis of ability to follow treatment programs and health plans. This is in addition to the delivery of preventive care to populations susceptible to problems such as hypertension and cardiac ailments. Coordination also determines the state of the healthcare system. The 2008 report analyzed this in terms of the rate of admission and discharge as well as the level of readmission after discharge. During this time, the report brought out the importance of qualified staff coupled with a good transitional program for patients on referral. For example, in 2004, the scorecard shows a variance between patient groups from 94 percent to 36 percent in the year 2006. This is compared to the number of discharges from the hospital that increased from 50 to 68 percent. These parameters can also be used in the system today in the evaluation of quality.
Access
The national scorecard on the US health system also examined access as a factor that is equally important in health care today. This is due to the increased debates on issues such as insurance for the population as well as affordability. The report in 2008 pointed out that an estimated 42 percent of the working population was uninsured in comparison to other countries. Furthermore, the challenges posed by insurance costs are still being felt today in the healthcare system. The scorecard at that time centered on the affordability of insurance. It was shown that the expected premium rates increased at a higher rate than that of earnings. In 2007, approximately 41 percent of the adult population had health debts. Current research attributes the problems of access to insufficient funds. It has been established that providing health care for all would cost approximately $88.6 billion.
In 2011, a survey carried out by the commonwealth fund emphasized the need to establish medical homes (Osborn, 2011). This was viewed as a method of mitigating financial impediments in access and delivery of medical care. Based on the outcomes of the survey, medical representatives from various states and countries made various recommendations. These included the need to develop plans that ensure easier access in terms of cost and quality. The issue of access as noted in 2008 is therefore still relevant as up-to-date studies are directed as minimizing cost to increase accessibility.
Efficiency
The 2008 scorecard also intimated that the health care system was inefficient. This was particularly brought out by the rate of admission, quality, and the organization of care. Efficiency is also defined by the rate of conformity to set rules and standards of health care delivery. This aspect is also fundamental in the improvement of access and quality. For instance, efficiency in the system has been attributed to easy cost management and control in the medical field (Barr, 2011). Further study has found that inefficiency in the US health care system occurs in areas of allocation and productivity (National Bureau of Economic Research, 2011). This refers to the outcome of healthcare and the benefits brought about by costs incurred in provision. Insufficiency has also been attributed to 395,000 deaths due to hypertension and 465,000 for smoking (Frenk & Murray, 2010). Furthermore, the recent focus on cost reduction efforts has been tied to the enhancement of efficiency. The situation can however be improved through the formulation and implementation of better health policies.
It is apparent that challenges highlighted in the 2008 national health scorecard are relevant to current health policy. It has been established that the scorecard evaluated the performance of the healthcare system based on factors that included quality, efficiency, and access as well as healthy life and equity. The study has concentrated on efficiency, quality, and access. This is because these factors have been the focus of major recent surveys and studies. In addition, it has been noted that access is intertwined with quality and related to efficiency. There is therefore a need for improvement in the health care system so as improve quality, access and efficiency so that more lives are saved.
References
Barr, D. A. (2011). Introduction to U.S. Health Policy: The Organization, Financing, and Delivery of Health Care in America. Baltimore: JHU Press.
Frenk, J., & Murray, C. J. (2010). Ranking 37th — Measuring the Performance of the U.S. Health Care System. The New England Journal of Medicine , 362, 98-99.
Garson, J. (2010). The US Healthcare System 2010 :Problems, Principles, and Potential Solutions. Current Perspectives , 101, 2015-2016.
McLaughlin, C., & McLaughlin, C. P. (2008). Health policy analysis: an interdisciplinary approach. Sudbury: Jones and Bartlett Publishers.
National Bureau of Economic Research. (2011). The Relative (In)Efficiency of the U.S. Health Care System. Web.
National Diabetes Information Clearing House. National Diabetes Statistics, 2011. Web.
Osborn, R. (2011). Controlling Costs Across Health Systems: The Commonwealth Fund 2011 International Symposium on Health Care Policy . Web.
The Commonwealth Fund Commission on a High Performance Health System. (2008). Why Not the Best? Results from the National Scorecard on U.S. Health System Performance. The Commonwealth Fund , 97.