Introduction
The contemporary global economy relies heavily on the need to have a stable healthcare system that caters for every citizen. This need is creating several structural realignments in the healthcare sector with a view to making it affordable and accessible to all (Commission of the European Communities, 2007). This work is an explication of healthcare system in Denmark, Netherlands in relation to the US
Denmark and Netherlands
Denmark experiences inequality in the provision of healthcare services. The vulnerable population of Denmark continues to be “alienated” from quality health care accessed by other high-class citizens (European Commission, 2006). These obvious disparities are, however, being eliminated gradually through several programs. The focus on the primary care and the quality agenda on health issues based on restructuring the hospital sector with a view to yielding a quality dividend in healthcare, have seen the sector improve. Coupled with the rationalization of hospital governance structures, the dream of a quality healthcare is yonder in Denmark (Younis, 2013).
The two-tier health sector-financing dichotomy in the Netherlands before 2006 had all along been considered an act of discrimination. This two-tier framework deeply exacerbated the inequality in the country. However, the current policy reforms require that all citizens acquire the basic insurance package (Smedley, Stith, & Nelson, 2003). The current restructuring process in Netherlands is slowly eliminating the two- tier system
Healthcare Performance in reference to population of Denmark
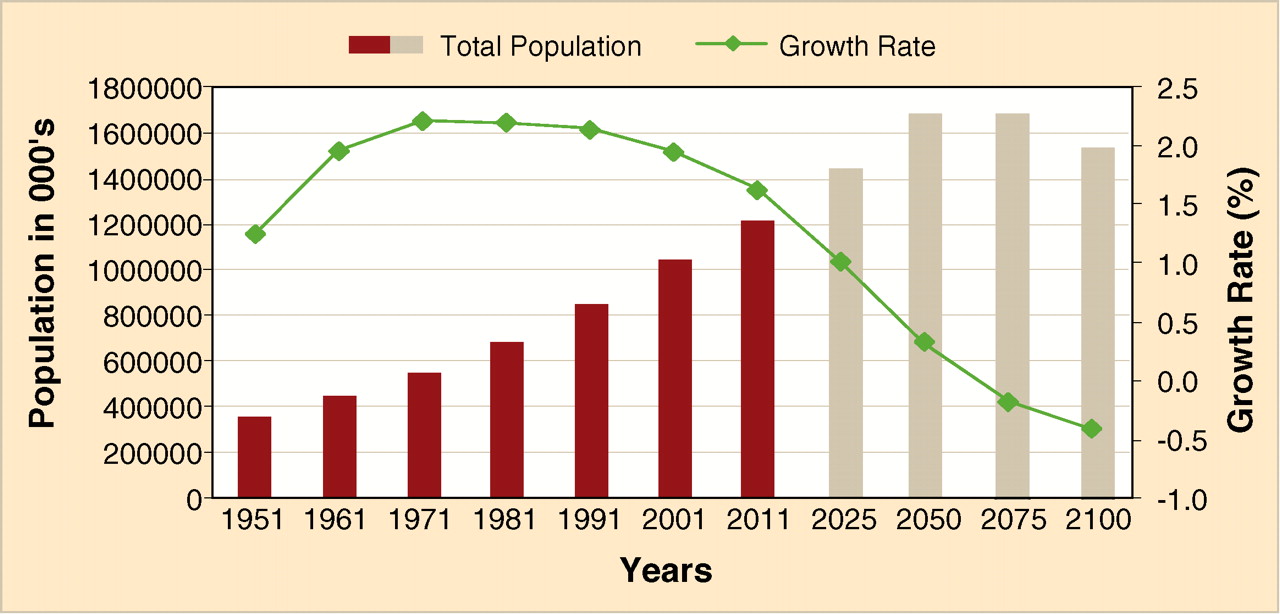
Denmark has a near optimal performance of the health sector as compared to other European neighbors (Eurohealthnet, 2013). With a population of 5.6 M and a growth rate of 0.2%, the healthcare budget for Denmark is considered very adequate. The 2008 Euro barometer survey on healthcare reveals that 90% of the Danes are satisfied with the healthcare performance. The public expenditure in the sector has been steadily rising by a margin of 8% annually (Eurohealthnet, 2013).
Netherlands
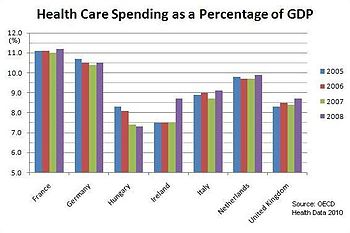
The healthcare spending in Netherlands has been on a plateau since 2005. The funding is an insurance issue and is highly regulated by the government. With a population growth rate of 0.5% per annum, analysts are warning that the recurrent budget on expenditure will considerably increase by a margin not less than 12%. So far, the performance of the sector has been very solid despite the cases of healthcare inequality witnessed (Equity Channel, 2013; Daley & Gubb, 2011).
US vs. Netherlands and Denmark
Denmark and Netherlands have an elaborate healthcare rubric that has reduced the inequality rate considerably (Gele & Harsløf, 2010). The restructuring of the funding process in both countries has greatly benefited them. Conversely, the American healthcare system ignored the majority of the unemployed poor. The adoption of the “Obamacare” though, has witnessed an improvement of the funding model (Younis, 2013).
Lessons for the US
Higher costs and unequal health programs remain America’s salient challenges in the healthcare sector. The US could borrow from Denmark, the restructuring of the healthcare facilities to enable complete decentralization of the process to enhance efficiency and equality (National Social Marketing Centre, 2013). Secondly, the adoption of the monthly tax credit for the low earners as done in Netherlands would boost healthcare in the low-end economic class (Stegeman, Costongs, Needle & DETERMINE Consortium 2011)
Maryland healthcare system
Healthcare issues in Bowie, Maryland have had an impact on the quality of healthcare in the US in general. The most salient problem in the town is the humongous rate of the uninsured citizens (13%). Bowie can choose to effect the tax credit refunds or employ a scheme through which the non-insured would be brought on board. Most prominently, the need to offer tax credits to this class of people would improve the terms of healthcare.
Conclusion
Management of the healthcare sector requires constant evaluation and assessment of the environmental dynamics. Issues such as population dynamics, economic balance, and poverty index must be factored during the planning process. The lesson from European experience in the management of the sector is a framework that can be employed in a setting and with little improvements, yield desirable results for effective healthcare management (Wellesley Institute, 2011).
References
Commission of the European Communities. (2007). Together for health: A strategic approach for the EU 2008-2013 [White paper]. Web.
Daley, C., & Gubb, J. (2011). Healthcare in Netherlands. Civitas, 12(3545), 16-20.
Equity Channel. (2013). Web.
EuroHealthNet. (2013). Health policies in the EU. Web.
European Commission. (2006). Tackling health inequalities in the EU: The contributions of Various EU-level actors. Web.
National Social Marketing Centre. (2013). Health equity case studies. Web.
Smedley, B. D., Stith, A. Y., & Nelson, A. R. (2003). Unequal treatment: confronting racial and ethnic disparities in health care. Washington, D.C.: National Academy Press.
Stegeman,I., & Costongs, C., Needle C., & DETERMINE Consortium. (2010). The story of DETERMINE: Mobilising action for health equity in the EU—Final report of the DETERMINE consortium. Brussels: EuroHealthNet. Web.
Wellesley Institute. (2011). European action on health. Web.
Younis, M. Z. (2013). Interview: Comparative effectiveness research and challenges to healthcare reform in Europe and USA. Journal of Comparative Effectiveness Research, 2(3), 223-225.