Introduction
Since they were commercially introduced in 1982, large-molecule biologic drugs have revolutionized the management and treatment of multiple diseases. Biosimilars are large-molecule drugs with similarities with but not identical to the reference biologics (those already approved) in terms of quality, safety, and efficacy (Kirchhoff et al., 2017). Many pharmaceutical companies in the US are developing biosimilar medicines at a relatively fast rate. More than 33 different biologics have been sent to the FDA for approval in 2022 alone (FDA, 2022). In addition, it is expected that an increasing number of newly developed biosimilars will hit the market as research on diseases of the immune system, the blood system, malignant tumors, the digestive system, connective tissue, and others progress (Kirchhoff et al., 2017). Nevertheless, the major problem affecting the adoption and use of biosimilars in the US healthcare sector is not related to their presence, but mainly the hesitance of healthcare providers to prescribe these medicines to their patients (Gibofsky, Evans & Strand, 2022). Nevertheless, specialized education is the most effective method for creating awareness and knowledge about biosimilars among prescribers, which will also encourage them to use the products. Consequently, this paper discusses the healthcare provider hesitancy around the use of biosimilars, the important role that the providers can play in improving patient acceptance of the products, and how specialized education to prescribers can help reduce healthcare practitioners’ hesitance to biosimilar use.
Description of Biosimilars and Their Importance Disease Management and Treatment
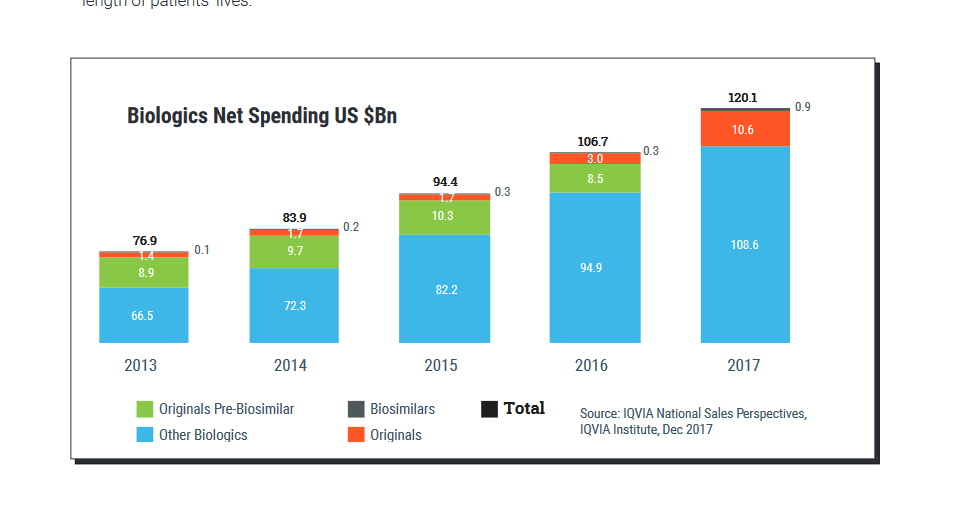
Biosimilars are a cost-effective alternative to their corresponding reference biologics approved for managing specific diseases as shown in figure 1. In particular, they represent the reference biologics in terms of efficacy, immunogenicity, quality, and safety. Although the process of making biosimilars is as complex as those used to manufacture the reference biologics, they fetch lower prices in the market for two reasons. First, they increase competition with the reference biologic, which forces prices downwards. Secondly, biosimilars have a reduced regulatory approval pathway (In the US, biosimilars go through an abbreviated approval process as they do not need to prove clinical efficacy given their similarity to the reference biologic). Consequently, patients access to care is increased, which can lead to early treatment initiation and a great therapeutic continuity for chronic diseases (Feldman & Reilly, 2020). At the same time, these products can help improve competition in the industry, which will eventually reduce the costs that payers have to endure every year.
There are various examples of biosimilars that have shown high levels of effectiveness, safety, efficacy, immunogenicity, and quality similar to their references. The drugs Truxima, Ruxience and Rixathon are biosimilars of trastuzumab (Herceptin), a targeted cancer drug (Feldman & Reilly, 2020). Like the reference product, these medicines have shown effectiveness and safety in managing chronic lymphocytic leukemia and some types of non-Hodgkin lymphoma and non-cancer related illnesses. Similarly, Idacio, Hyrimoz, Yuflyma, Imradi, and Amgevita are biosimilars of adalimubab (Humira), which is used to treat several conditions such as ulcerative colitis, Crohn’s disease, and arthritis (Huizinga, Torii & Muniz, 2021). In all these examples, the biosimilars fetch lower prices compared to their reference biologics, hence making it possible to improve patient access to treatment early enough.
Healthcare Provider Hesitancy as a Barrier to the Use of Biosimilars in the US
Although regulatory and legal limitations are known to be the most observable barriers to the availability of biosimilars in the country, the adoption and final use largely depend on the willingness and ability of the healthcare providers (HCPs) to prescribe the products and the readiness of the patients to accept them. Even in Europe and China where there are larger numbers of approved biosimilars, the rate of uptake is reduced because of the low rate of adoption by HCPs and the willingness of the patients to accept them (Declerck et al., 2017). According to Tanaka et al. (2022), systematic reviews of surveys in US, Japan, and Europe reveal that HCPs in the regions generally lack overall familiarity and understanding of the products. Moreover, they demonstrate a large degree of concerns about safety and efficacy among HCPs, which greatly limits biosimilar prescribing. In another systematic review by Cohen et al. (2018), it was revealed that even in cases where the HCPs have knowledge and positive attitudes towards biosimilars, the prescribing can be limited for patients already exposed to biologics.
In general, it was revealed that HCPs may avoid switching from reference biologics to biosimilars due to skepticism regarding pharmacist-led substitution of medicines. Studies have also revealed that lack of involvement of subspecialists with more experience regarding the use of biosimilars is also a major factor that contributes to the low rate of biosimilar prospection in the US (Feldman & Reilly, 2020). Poor collaboration between the stakeholders has reduced the confidence of prescribers. Moreover, low access to unbiased educational material about biosimilars and lack of autonomous shared-care decision-making process have constrained the use of the products in the country.
All these factors greatly contribute to the high level of prescriber hesitancy around the use of biosimilars in the country. Nevertheless, there is hope because recent studies have shown that the overall familiarity and understanding of biosimilars among HCPs have improved since 2015 (Leonard et al., 2019). Physicians and pharmacists appear to comprehend the definition of biosimilars as used by FDA. However, surveys also reveal that most physicians and pharmacists approach the use of biosimilars cautiously because of the existing concerns regarding the extent of cost savings, pharmacist-led substitution, interchangeability, and nonmedical switching.
Nonmedical switching with biologics takes place when a patient changes from an approved reference products to its biosimilar or vice versa for some reason not related to the clinical demands. Such reasons include insurance formulary coverage and treatment costs and availability. A 2019 survey with pharmacists and clinicians revealed that more than 80% of those surveyed are concerned with nonmedical switching to biosimilars (Leonard et al., 2019). Moreover, they are concerned with the impact of the switching to the patient care and their practices. In another 2019 survey of 320 rheumatologists, over 73% reported that they are ready to switch from prescribing one rheumatic drug reference to another rather than going for its biosimilars (Cohen et al., 2018). In this study, less than 35% of the respondents expressed willingness to switch from a reference rheumatic drug to its biosimilar (Cohen et al., 2018). Among others, they cited concerns about the possible impact on patients, patient perceptions, and their careers as the reasons that motivate them to avoid switching to biosimilars. Likewise, a 2020 survey with 602 HCPs reveal that prescribers are more likely to use a biosimilar to patients who are newly starting therapy than to those already using reference biologics (Feldman & Reilly, 2020). Consequently, nonmedical switching is a factor that contributes to the prescribers’ concern with biosimilars, thus their hesitancy around the product use.
Interchangeability refers to the practice of changing one drug for another with an aim of achieving the same clinical effect in each patient. In any given patient, an interchangeable biologic is a biosimilar whose results are the same as those of the reference product. The FDA has approved almost 40 biosimilars as of October 2022, but it has granted an interchangeable designation to a limited number of the approved products (Gibofsky, Evans & Strand, 2022). The FDA requires additional studies to demonstrate that a biosimilar is an interchangeable product per each patient, which makes many drug manufacturers to avoid seeking for an interchangeability approval (Leonard et al., 2019). This is a major concern among HCPs because they are mostly not aware whether a product is an interchangeable biosimilar or not.
Low level of clarity is a problem affecting HCPs as they prescribe biosimilars. According to a survey conducted between 2017 and 2021, there is a lack of clarity on interchangeability among HCPs, which makes them avoid prescribing biosimilars to their patients despite having knowledge of their effectiveness and low prices (Gibofsky, Evans & Strand, 2022). Furthermore, over 84% of rheumatologists in a 2019 survey reported that they were aware not all FDA-approved biosimilars are automatically deemed interchangeable by the regulator (Leonard et al., 2019). Nevertheless, just 20% were aware that the FDA approval of a drug as interchangeable meant that the product could be substituted without the need to contact the prescriber (Feldman & Reilly, 2020). Moreover, the majority of the prescribers were not aware that none of the existing biosimilars are designated by FDA as interchangeable. Therefore, the lack of intertangle biosimilars is a major factor that makes HCPs to be hesitant in prescribing these products in the US.
Pharmacist-led substitution is the concept of dispending one medicine instead of another generic drug or an interchangeable biosimilar without consulting the prescriber. The FDA generally allows the pharmacist-led substitution for small-molecule medicines, specifically for drugs with pharmacokinetic bioequivalent to the reference product (Feldman & Reilly, 2020). Most HCPs are largely opposed to automatic substitution of these medicines by pharmacists. Physicians generally express hesitancy due to concern about loss of involvement in patient treatment and dealing with high levels of complexity related to the use of biosimilars.
Prices and cost savings also results in HCPs hesitance in using biosimilars in the US. Biosimilars are developed with an intention of providing affordable options for treatment to patients and payers, which is expected to lower the systemic financial burden because of the lower prices (Gibofsky, Evans & Strand, 2022). In addition, the idea is to increase competition with the reference biologics, which will eventually reduce the cost of all drugs. Studies indicate that for each therapeutic reference product, there should be more than one biosimilar if costs are to reduce significantly. Nevertheless, there are very few biosimilars in the market today, which reduces motivation among HCPs to use the products when the costs are even not justified (Gibofsky, Evans & Strand, 2022). For example, a recent study shows that the majority of HCPs in different drug management fields are likely to choose the approved reference products over their biosimilars when both products are available and on the formulary.
Moreover, the study indicates that lack of a difference in formulary statuses between the two drugs and financial incentives greatly reduce the wiliness of the HCPs in using biosimilars. Additionally, savings realized by the payers and consumers have so far not demonstrated direct benefits to the patients and their families, which reduces the incentives of the HCPs to prescribe biosimilars. Absence of strong financial incentives to prescribe biosimilars makes HCPs to seek prior authorization to receive the approved reference products for patients already under therapy despite knowing the administrative burden associated with them. Majority HCPs report that they are likely to prescribe biosimilars when they clearly understand that the costs of therapy on their patients will reduce. However, even in cases where HCPs know that the biosimilar will reduce costs for patients, they are also concerned that the product discount programs can mitigate difference in the costs. Insufficient cost savings reduces the likelihood of the HCPs to switch to biosimilars. They tend to seek greater transparency about the prices of the approved biosimilars and their reference biologics. If HCPs can clearly see the direct cost savings for their patients, they are likely to feel encouraged to continuously prescribe those biosimilars. Instead, requirements for prior authorization and appreciation of drug discounts burden the prescribers, which makes the potential cost savings less rewarding. Due to the long process, prescribers are likely to stick to the reference biologic even when they are aware that they might help their patients reduce costs.
The Role of Specialized Education in Addressing and Resolving HCP Hesitancy
Even though the HCP understanding and perception of biosimilars is improving with time, the level of acceptance greatly varies across the difference specialties in the US healthcare sector. For example, most oncologists readily accept biosimilars as a low-cost and clinically useful alternative to the reference biologics necessary to alleviate financial burden of cancer treatment (Gibofsky, Evans & Strand, 2022). On the contrary, most gastroenterologists tend to be highly concerned with the safety, indication extrapolation, and immunogenicity of biosimilars, thus a high level of hesitance. Therefore, it is important for HCP education to be highly specialized rather than remain generalized as it is the current state. Prescribers across specialties will benefit from specialized education because misconceptions and misinformation lie within each specialty about the robust evaluation, review, and approval standards by FDA.
Moreover, prescribers require specific rather than general data for extrapolated indications. It is the role of manufacturers and FDA to provide real-world data that demonstrate the safety and efficacy of each biosimilar compared to the reference products. Such comparisons should be provided in journals, books, and materials that should be disseminated to the prescribers along with each biosimilar (Gibofsky, Evans & Strand, 2022). It is also important to consider the fact that most prescribers are too busy to take time reading in-depth clinical data. Instead, HCPs should receive easily digestible materials that clearly and simply describe and demonstrate the safety, cost saving ability, equivalence, and other characteristics of each biosimilar in relation to its reference biologic.
Conclusion
This paper has examined the problem of hesitance of healthcare providers in prescribing biosimilars in the United States. Evidently, even though many biosimilars are set to be approved in the next few years, the rate of their use might still be below expectations mainly because of this hesitance. The problem is the willingness of the HCPs to use the biosimilars for the first time to switching to them. As the paper indicates, HCPs resistance results from various factors, especially poor understanding of the biosimilars and low incentives to use them. The most successful way of resolving and addressing the problem of HCP hesitance is to provide specialized education on the use of biosimilars. Generalized information has proved to be less effective, which implies that for each biosimilar and specialty, education materials should be provided to the HCPs. In addition, such materials need to be simplified and easy to read and understand and should compare each biosimilar and its reference biologic.
References
Cohen, H. P., Blauvelt, A., Rifkin, R. M., Danese, S., Gokhale, S. B., & Woollett, G. (2018). Switching reference medicines to biosimilars: A systematic literature review of clinical outcomes. Drugs, 78(4), 463-478.
Declerck, P., Danesi, R., Petersel, D., & Jacobs, I. (2017). The language of biosimilars: Clarification, definitions, and regulatory aspects. Drugs, 77(6), 671-677.
FDA. (2022). Center for Drug Evaluation, Research. About biosimilars and interchangeable products. Web.
Feldman, M., & Reilly, M. S. (2020). A white paper: US biosimilars market on pace with Europe. Generics and Biosimilars Initiative Journal, 9(4), 150-155.
Gibofsky, A., Evans, C., & Strand, V. (2022). Provider and patient knowledge gaps on biosimilars: Insights from surveys. AJMC, 28, 2227-S233. Web.
Huizinga, T. W., Torii, Y., & Muniz, R. (2021). Adalimumab biosimilars in the treatment of rheumatoid arthritis: a systematic review of the evidence for biosimilarity. Rheumatology and Therapy, 8(1), 41-61.
Leonard, E., Wascovich, M., Oskouei, S., Gurz, P., & Carpenter, D. (2019). Factors affecting health care provider knowledge and acceptance of biosimilar medicines: A systematic review. Journal of Managed Care & Specialty Pharmacy, 25(1), 102-112.
Tanaka, E., Kawahito, Y., Kohno, M., Hirata, S., Kishimoto, M., Kaneko, Y., Tamai, H., Morinobu A., Sugihara, T., Murashima A., Kojima, M., Mori, M., Ito, H., Kojima T., Sobue Y., Nishinda, K, Matsushita, I., Nakayama, T., Yamanaka, H., & Harigai, M. (2022). Systematic review and meta-analysis of biosimilar for the treatment of rheumatoid arthritis informing the 2020 update of the Japan College of Rheumatology clinical practice guidelines for the management of rheumatoid arthritis. Modern Rheumatology, 32(1), 74-86.