Levocarnitine is a compound that occurs naturally and plays a part in ferrying fatty acids into the mitochondria for β- oxidation. It acts as an acyl group acceptor thereby helping to maintain adequate cellular levels of free coenzyme A (CoA). Likewise, it functions as an osmoprotectant in organs such as the kidneys, and as a plasma membrane stabilizer (Cuturic et al., 2013). In humans, endogenous L-carnitine level is furnished by its absorption from dietary sources, from de novo biosynthesis and extensive tubular reabsorption in the kidneys. The molecule has a potential of being used as a medicinal compound and as a food supplement. In this paper, however, specific focus is given to the purported uses of levocarnitine for treating psychiatric diseases, e.g., depression, anorexia, etc. The scientific evidence supporting its use as a mental health drug, and some of its pharmacodynamics properties are also presented.
Uses in Psychiatric Disease
Numerous studies have demonstrated levocarnitine’s antioxidant properties, its role in sequestering free radicals and in reducing physical and mental fatigue in elderly (Cuturic et al., 2013). The use of levocarnitine and l-acetylcarnitine has several benefits including improvement of the motor, cognitive and behavioral functioning. A study with a high dose l-carnitine treatment in a transgenic mouse model of Huntington’s disease demonstrated that the compound had neuroprotective properties and alleviating effects on the condition (Cuturic et al., 2013). Similar studies were conducted on human subjects using low doses of levocarnitine, and after a six month monitoring period, the results showed that the compound had benefits of slowing down the progression of Huntington’s disease (Cuturic et al., 2013). Equally, treatment of the activated microglia with levocarnitine reverses the impact of detrimental neuroinflammation associated with Parkinson’s disease.
The attention-deficit hyperactivity disorder (ADHD) is a heritable neurobehavioral condition that often occurs in children who present a range of problematic behavior (Cuturic et al., 2013). It is caused by structural or functional aberrations in the communication between the basal ganglia and the frontal cortex. While this condition is adequately treated using stimulants, antidepressants, clonidine, and bupropion, some of these drugs are associated with adverse side events. L-carnitine is a safe alternative compound to treat the condition. Also, a combined regimen of carnitine and cobamamide has been shown to improve anorexia nervosa patients’ physical state, i.e., it normalizes the gastrointestinal function, increases body weight, and promotes the growth of brain tissues (Onofrj et al., 2013).
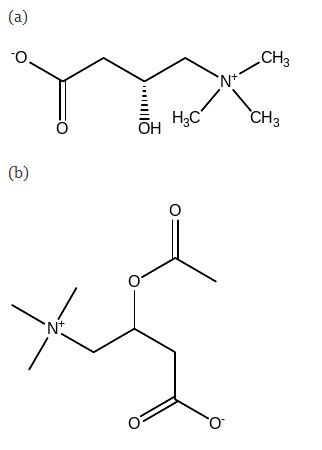
The enzymatic attachment of an acetyl group to levocarnitine readily yields l-acetylcarnitine (ALC). Inside the cell, carnitine and acetylcarnitine are inter-convertible. This l-carnitine derivative has beneficial effects on patients diagnosed with depressed mood and dementia (Onofrj et al., 2013). It is useful in treating moderately depressed mood and has fewer side effects. Also, it is widely used to treat cognitive impairment associated with dementia, Parkinson’s disease, and other neurodegenerative disorders. Acetylcarnitine taken at a dose of 2g/day helps to improve memory and word recall in abstinent alcoholics who are cognitively impaired (Onofrj et al., 2013).
Supporting Evidence
Low levels of levocarnitine (≤ 20μmol/l) have been associated with incidences of ADHD behavior in children. In a trial treatment, children who have ADHD were treated with 100mg carnitine two times a day (Cuturic et al., 2013). A decrease in hyperactive, impulsive behavior was observed. Cessation of the carnitine medication resulted in a recrudescence of ADHD symptoms, while its reintroduction led to improved response again. Continued use of the drug for six months caused the restoration of normal, non-clinical behavior in those children. The carnitine system plays a role in the mitochondrial elongation-desaturation of (n-3) fatty acids to form a docosahexaenoic acid (Cuturic et al., 2013). This fatty acid is vital for brain maturation and functioning, and its concentration is shallow in the plasma of ADHD patients. Possibly, carnitine’s role in reducing ADHD severity may be through stimulating the synthesis of both docosahexaenoic acid and acetylcholine in specific regions of the brain (Cuturic et al., 2013).
In psychiatric patients, chronic valproate therapy results in hypocarnitinemia that leads to metabolic encephalopathy. A study by Cuturic et al. (2013) on 38 hypocarnitinemic patients with some degree of cognitive impairment reported that a combination therapy of oral levocarnitine and the comprehensive psychiatric treatment resulted in overall improved behavioral, cognitive and motor functioning. The evidence also suggested influences of ethnic traits in carnitine bioavailability since the outcome was more favorable among Caucasian subjects than among African-American counterparts (Cuturic et al., 2013).
Experiments involving cellular and animal models have demonstrated that acetylcarnitine has a potential for treating depression (Wang, Han, & Lee, 2014). Also, several randomized clinical studies revealed ALC’s potency in treating the dysthymic disorder, fibromyalgia, and minimal hepatic encephalopathy with marginal side effects (Wang et al., 2014). The researchers concluded that ALC is a promising efficient and safe next treatment alternative with “novel action mechanisms for depression patients, especially, the elderly and persons with co-occurring diseases and who react negatively to antidepressants” (Wang et al., 2014, p. 35).
Side Effects
Apart from its usefulness, levocarnitine may elicit some unwanted effects. Among the adverse events, hypertension, tachycardia, fever, and seizures are severe, occur infrequently and require medical attention. Additional side effects may feature, but do not need medical care since they dwindle with time as the body adjusts to the drug. In this group are diarrheas, headache, nausea/vomiting, abdominal discomfort, depression, dizziness, impaired vision, loss of appetite, swelling of body appendages, itching, and weakness. The majority of these effects occur less frequently. Levocarnitine use produces an unpleasant body odor, likely because of the formation of trimethylamine during its metabolism (Cuturic et al., 2013). An overdose of levocarnitine (~4000mg) has been reported to cause transient psychosis in persons with a history of substance abuse (Cuturic et al., 2013). The condition presents with symptoms of agitation, violence, confusion, renal dysfunction, rhabdomyolysis and auditory hallucinations.
Drug Interactions
Two drugs have been shown to interact with levocarnitine. These are dicumarol and warfarin (Coumadin, jantoven, and warfarin). Using these drugs together with levocarnitine may lead to increased risk of bleeding. Some evidence has suggested that levocarnitine prolong the hypoprothrombinemic effects of warfarin and other coumarin anticoagulants, although the mechanisms of interaction are yet to be confirmed (Cuturic et al., 2013). Cases of international normalized ratio (INR) increase and bleeding were reported in patients treated with warfarin or acenocoumarol following the introduction of levocarnitine regimen (Cuturic et al., 2013). Discontinuation of levocarnitine led to a restoration of normal INR levels. Thus, precaution should be taken when using coumarin anticoagulants with levocarnitine, including frequently checking the INR levels and adjusting the anticoagulant levels accordingly.
Recommendations
Given that levocarnitine and acetylcarnitine occur endogenously, they are safe drugs to use. Although the search for valid scientific and clinical evidence continues, I recommend the inclusion of these drugs in the psychiatric treatment regimen.
Conclusion
In summary, levocarnitine has several properties which are potentially beneficial in treating psychiatric ailments. Although levocarnitine is in the market, it is licensed as a drug for other conditions and not mental disorders. However, since the supplement is well tolerated in the body, its adoption in psychiatric practice is overdue.
References
Cuturic, M., Abramson, R. K., Moran, R. R., Hardin, J. W., Frank, E. M., & Sellers, A. A. (2013). Serum carnitine levels and levocarnitine supplementation in institutionalized Huntington’s disease patients. Neurological Sciences, 34(1), 93- 98. Web.
Onofrj, M., Ciccocioppo, F., Varanese, S., Di Muzio, A., Calvani, M., Chiechio, S., …Thomas, A. (2013). Acetyl-l-carnitine: From a biological curiosity to a drug for the peripheral nervous system and beyond. Expert Review of Neurotherapeutics, 13(8), 925-936. Web.
Wang, S., Han, C., & Lee, S. (2014). A review of current evidence for acetyl – l – carnitine in the treatment of depression. Journal of Psychiatric Research, 53(1), 30-37. Web.