Executive Summary
Identified patient problem: Hong Kong pilots are at a high risk of having obesity that affects their health and subjects them to comorbidities.
Aim: To develop a cohesive strategy of obesity management that targets issues associated with pilot’s work.
Practice Gap:
- Nurses in the clinic have inadequate knowledge required to manage patients with obesity.
- The existing management practice involves ordering additional test studies, stress ECG, or multiple referrals to specialists, without a guideline for addressing obesity and its causes.
- Additional education and training of the nursing staff are necessary to help pilots learn how to manage their condition considering the specifics of their work.
- Pilots with high BMI should be able to manage their weight through behavioural change since the process requires long-term adherence to recommendations.
Objectives:
- Improve the knowledge of the clinic’s nurses regarding obesity management and weight reduction strategies suitable for pilots.
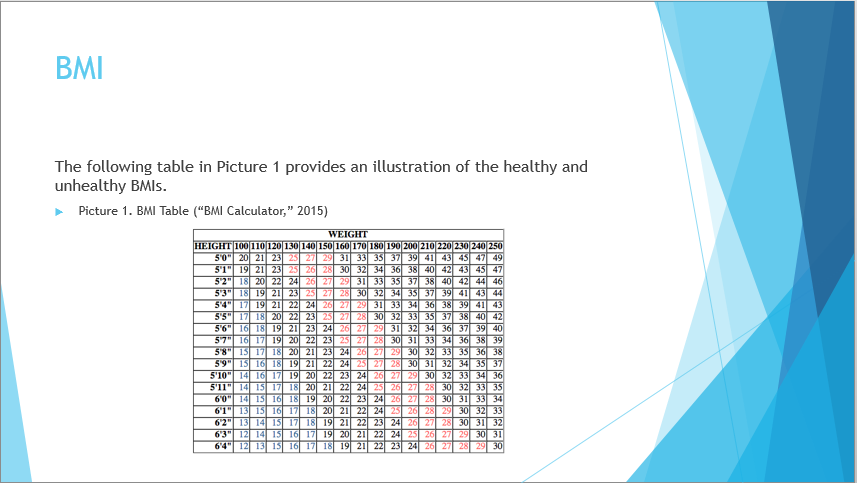
- Reduce the BMI of pilots with results of 35 and higher, by helping them lose 5% to 10% of the initial weight.
- Mitigate the risk comorbidities such as sleep apnoea that can lead to a pilot’s licence suspension through behavioural weight management.
Learning Tasks/Activities:
- Update and improve personal knowledge regarding the adverse outcomes associated with pilots’ work and obesity as a common diagnosis for the population and review the current literature to locate evidence-based strategies for weight management.
- Develop a guide for teaching behavioural change practices to pilots and consulting with Aviation Medical Examiners to gain the approval of the strategy and conduct a workshop for nurses.
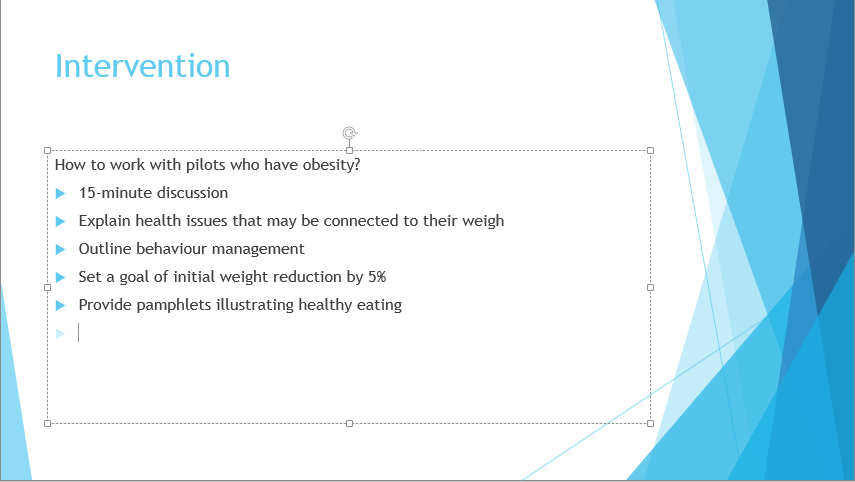
- Develop a guide for nurses that will help manage obese patients and conduct a lifestyle modification program interventions by having 30-minute sessions with pilots and give them pamphlets and self-monitoring forms.
- Evaluate the outcomes and finalise the recommendations that can be used by the clinic’s staff to aid pilots in managing their weight and obesity comorbidities. Also, examine the compliance and adherence rates based on pilot’s answers in the self-monitoring forms.
Background
Obesity is a common issue that is reflected in the excess weight that affects an individuals’ health by resulting in comorbidities, such as sleep apnoea, heart disease or others. The statistics for the Hong Kong population presented on Figure 1 as it suggests that one in four individuals suffers from obesity, which is provided by the Hong Kong government. Studies by Bhat, Verma, Pant, and Singh Marwaha (2019), Caldwell et al. (2009), Cao et al. (2019), Causse, Chua, and Rémy (2019) and show that pilots are especially vulnerable to developing obesity, and Cheng et al. (2016) suggest that behavioural change is the most feasible strategy of sustainable weight management.
If the pilots have an abnormal BMI, waist and neck measurements, the clinic usually sends them for additional tests, and if the issue is not managed appropriately, the pilots can be grounded for three months or get suspended. Also, in her article Blakemore (2018) discusses the issue of doctors not sending their patients for further evaluations if they are obese providing an understanding of a need to develop a clear guideline for clinicians and nurses. Despite the evidence supporting behavioural change and behavioural change for weight loss, many medical professionals fail to refer their patients to appropriate specialist that would help them manage their weight.
Identified Patient Problem and Practice Gap
The number of people in Hong Kong who suffer from obesity is 25% while de Souza Palmiera and Marqueze (2016) report that more than 50% of pilots are overweight and out of them, approximately 14% are diagnosed with obesity. Hence, this is an increasing problem both for the general population and for pilots who depend on good health to be able to renew their license and continue working in aviation, since the regulations in this field are stringent. The health promotion model (HPM) and the Donabedian’s model are used to structure the nutrition and physical activity elements of this intervention.
A common problem is the inability to adjust personal lifestyle to the requirements of the job. The examined pilots were interviewed to evaluate their perspective on why they gained weight and most report the irregular work hours, time zone changes, frequent stays in hotels, and work-related stress as the main reasons they are unable to sustain a healthy diet. This is consistent with the reports of scholars such as Gupta, Coates, Dorrian, and Banks (2018), Lord, and Conlon (2018) and Nicole et al. (2019) with specific emphasis on shift work, identified by Gupta et al. (2018) as the main issue contributing to excess weight gain. Additionally, most pilots report a lack of physical activity, both when working and on the weekends, which is also a result of their work.
Another practice gap is the lack of knowledge of staff members that is necessary to manage obesity. This is an essential component since under the current protocols; the Aviation Medical Examiners have to send the pilots undergoing a routine examination for additional testing or suspend them from flying if their health assessment indicates issues with weight. However, this does not address the problem of reducing weight to achieve a healthy BMI and mitigate possible comorbidities, which is usually a long-term process requiring input both from a healthcare professional and from a patient.
Objective
The main focus of this intervention is on developing an obesity behavioural change program for pilots undergoing a routine check-up at the aviation clinic and improvement of nurses’ knowledge regarding the issue, which should help mitigate the adverse outcomes of obesity. The program timeline is from September 2019 until the result evaluation in August and the pilots will be able to continue adhering to the recommendations after the project is over.
Four Learning Tasks
The 7 APN domains were targeted when designing the learning tasks and through this project were achieved. The GIBBS reflective cycle is used to evaluate the scenario of this intervention – five pilots with excess weight came to the clinic to renew their license. Apart from the weight, two of the five suffered from sleep apnoea and were dissatisfied with their health.
- Feelings – I felt guilty because the clinic does not have a standard practice for helping patients with obesity.
- Evaluation – It is clear that the clinic encounters a substantial number of patients with obesity and this condition affects different domains of their health.
- Conclusion and Analysis – The main issue is having a proof of concept that the proposed intervention will have a positive impact. This requires collecting evidence such as studies and conducting an intervention that will help address the problem.
- Action plan – I have decided to develop a guide that pilots can use to change their unhealthy behaviours, since the intervention is easy to implement and does not require continuous monitoring from nurses.
Learning Task One: Improve my understanding of comorbidities prevalent in the pilot population
The main objective of this learning task was to identify the practice gap and improve my knowledge and understanding of obesity, leading indicators, and its impact on a person’s health. The review of the literature and the guideline on cardiac health issues prevalent in the population of pilots revealed that obesity is a severe concern. In order to improve my professional knowledge of healthy weight management, I enrolled in an online nutrition course. Additionally, to enhance the understanding of the behavioural change principles, I took an online course regarding the behavioural change essentials at Beck’s institute. Furthermore, I was able to consult with an Aviation Medical Examiners to receive advice and approval of the project.
In general, based on these findings, a self-assessment questionnaire and a checklist for pilot check-ups was developed. APN domains 4, 6 and 7 were achieved since I consulted with an Aviation Medical Examiner working in aviation-specific healthcare and located evidence-based studies supporting the need for a similar program. In addition, I enrolled in a specialised course on behavioural change to obtain a certificate and improve my understanding of this concept.
The following questionnaire was distributed to pilots during the 15-minute session. The funnelling method was applied to design these questions.
- Describe your daily eating habits, providing details about types of foods you consume and alcohol intake.
- Tell us about your routine for cooking at home.
- Tell us about your exercise and physical activity routine.
- Explain how you think an improvement can be made to the eating and exercise routines.
Learning Task Two: Create a workshop for nurses
In this learning activity, I prepared a two-hour workshop for the nurses working in the clinic to close the practice gap of obesity management. I developed a questionnaire for nurses to evaluate their knowledge pre and post-workshop and identify whether they benefited from the initiative. Through this learning task, APN domains 2 and 4 were achieved since I participated in the quality improvement program for my clinic.
Learning Task Three: Have a staff workshop discussing obesity and develop a guide
A PowerPoint presentation (See Appendix) with the primary assessment questions was prepared, and we discussed and role-played two patient case studies from our practice to establish a protocol for addressing obesity. The main goal was to ensure that the nurses know how to assess main characteristics indicating that a pilot’s excess weight may endanger his or her health (Zhao, Su, Wang, Wang, & Zhan, 2018; Sykes, Larse, Griffith, & Aldington, 2012; Xanthopoulos, Berkowitz, & Tapia, 2018). Additionally, as suggested by Hood, Corsica, Cvengros and Wyatt (2013), Hood, Nackers, Kleinman, Corsica, and Katterman (2014) and Raynor, Thomas, Cardoso, Wojtanowski and Foster (2019) self-management is the key to achieving success in weight loss, hence, in the workshop, the nurses discussed strategies for empowering pilots and helping them set adequate goals for healthy weight loss and track progress through self-assessments. Stress management and rewards were also discussed, which are supportive mechanisms helping sustain adherence to the program in the long term.
APN domains 1, 3, 5, 6 were achieved since I displayed leadership qualities by organizing and managing the workshop. Additionally, I negotiated an improvement for the clinic’s existing practises to ensure that pilots receive support and guidance with the issue of obesity, which also contributed to the promotion of the advanced practice attributes.
Learning Task Four: Develop a comprehensive practice guide on behavioural lifestyle change with recommendations for obese patients, evaluate the results of the intervention
This learning task was the final part of the intervention, and it incorporated an evaluation of the results. Five pilots were asked to participate in the program since their routine check-ups revealed issues with excess weight. They were instructed on the specifics of behavioural change, provided with a 30-minute training on breathing for stress management, and presented with a printed copy of the self-monitoring guide.
Additionally, to ensure a healthy weight loss practice, I assisted them in setting a target weight, which was no more than 5% of the initial measurement. The detailed information on the target measures is presented on Figure 2. The pilots were encouraged to choose rewards as part of the process to ensure sustainable changes. The inclusion of 30-minute face to face interventions include the breathing exercises, diet, nutrition, physical activity, dietary food choices and better choices, goal setting, list of self-monitoring forms, pamphlets and posters ,lastly discussion of rewards.
The main quantitative outcome measures were BMI, neck circumference, waist, and the lab tests, including a lipid profile, hba1c and glucose, which were collected before and after the interventions. For the qualitative outcome evaluation and in order to examine whether the pilots were able to benefit from the behavioural change program, phone calls every three months after the initiation of the intervention. In order to recall the pilots for weight checking, I scheduled follow up calls with the same assessment checklist to identify the change in their behaviour,
Additionally, they were asked to provide information about their weight, waist, and neck measurements as part of their self-reporting process, which is the quantitative assessment of the results. For the qualitative evaluation, they were interviewed to describe their perception of the program, usefulness, and impact of rewards on the results.
APN domains 1 and 4 were achieved since the evaluation of results have proven that the intervention is indeed useful and enhances the quality of healthcare services provided by the aviation clinic. Additionally, this program improved my personal attributes since I learned about evidence-based obesity management practice specific for the pilots and improved my leadership skills.
Encountered Difficulties and Solutions
The pilots visit the clinic to renew the license that allows them to continue working. One can argue that behavioural change is a complicated matter that requires continuous input from patients. Hence, the main difficulty encountered during this project was the need to develop a strategy for explaining nutrition, diet, and techniques for self-monitoring, stress management, and goal setting in regards to their weight. However, the fact that the clinic is responsible for the pilot’s health assessment allowed to develop a reward system.
One issue was connected to developing an adequate incentives plan that would motivate the pilots to participate in this project and adhere to the recommendations. Self-rewards were included as part of behaviour management since the clinic can provide 20% of the other country’s license and 50% of the license investigations, for example, ECG or audiogram.
The most critical observable contributing factors to the improvement of pilot’s health were the ability to review their eating behaviour in different conditions, for instance, during long flights. The positive impact on subjects, nurses, and practice is in the ability to use this program to help other pilots improve their health. After implementation, the pilots report feeling better and having more control over their eating behaviour, which contributes to their quality of life.
Sustainability
The program’s duration is from September 2019 until August 2020 and it is designed to achieve results and sustain the outcomes. Additionally, it is vital to ensure that similar learning workshops are held at the clinic to enable continuous improvement of the nurses’ knowledge on nutrition, physical activity, and approaches to improving the health of aviators. Another strategy is recording the essential parts of the workshop as a video, for instance, explaining the main principles of healthy nutrition and behavioural change.
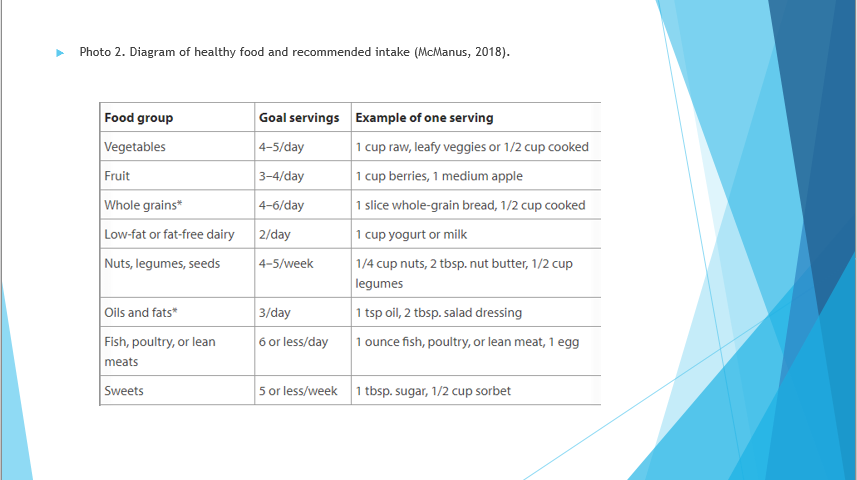
Healthcare organizations such as the World Health Organization or the Hong Kong government developed guides on healthy diet and food which can be used by nurses during their work (“Healthy diet,” 2018; “Towards 2025”, 2018; “Change for health,” n.d.; “Obesety”, 2019). Additionally, the self-assessment forms and questionnaires for pilots can be distributed digitally to all nurses in the clinic to ensure that they always have a copy. In general, this program can be sustained by encouraging the nurses to be a part of the project and presenting them the positive outcomes of this intervention as evidence.
Results
Workshop Questionnaires
The questions were developed using the example of a questionnaire by Snodgrass et al. (2016).
- Do you address weight management when working with pilots or do you plan on doing so in the future?
- How often do you encounter pilots undergoing medical certification tests that have evident weight management issues?
- Are there specific resources or advice that you can give pilots that need to manage their weigh?
- Explain how you usually react if a patient has excess weight?
Staff Knowledge Pre and Post Workshop Evaluation
Each response counts as 1 point.
- What national or interactions healthcare organizations’ diet guides can you recommend to your patients (name at least two)?
- What is the average BMI, and which BMI is considered dangerous for a person’s health?
- What complications can a patient with obesity have if the weight is not managed?
- Apart from weight, what other factors can be used to diagnose obesity (at least 3)?
- What options of behaviour management can be used to help patients lose weight (at least 2)?
The questions and correct responses for the nurses that were used to evaluate their knowledge of obesity and excess weight management. In summary, the evaluation of results is presented in Figure 3, suggesting that nurses lacked the necessary knowledge before the workshop. Out of the five questions, the first nurse scored 3, while the second answered two questions, while after the workshops, all five questions were answered correctly by both nurses.
Assessment Form for Qualitative Evaluation
Table 1. Results evaluation (created by the author).
Table 1 contains the initial BMI of pilots at the beginning of the intervention, as well as their results over twelve months of monitoring, are recorded. The outcomes suggest that the five were able to significantly reduce their weight, although only Patient 3 achieved healthy BMI. This may be connected to the high initial BMI of patients 2 and 3, who will need to continue using the intervention to gain healthy weight, but the two pilots are no longer obese. Pearson Moment correlation for bodyweight is 1, which indicates a linear relationship between the initial and outcome BMI.
The Likert evaluation scale is used in this section.
- Do you track your daily food intake? (not necessarily calories, but what you eat during a day)? (never -1, sometimes – 2, occasionally- 3, from time to time – 4, always – 5)
- Do you track your physical activity levels? (never -1, sometimes – 2, occasionally- 3, from time to time – 4, always – 5)
- Are you satisfied with your physical health? (very unsatisfied – 1, somewhat satisfied – 2, partially satisfied – 3, satisfied – 4, very satisfied -5)
- Do you perceive your eating habits as good? (very bad – 1, not good – 2, somewhat good – 3, good – 4, very good – 5)
- Do you experience significant stress at work? (never -1, sometimes – 2, occasionally- 3, from time to time – 4, always – 5)
Figure 4 contains their responses before and after the intervention. Before the intervention, the five pilots scored below 10 points each when describing their satisfaction with their weight and healthy habits. The results support the conclusions made by evaluating the open-ended questions distributed to pilots. After the intervention, patient 2 reports 25 points and others report above 15 out of 25 quality of life, indicating a significant improvement. In summary, the pilots benefited from intervention since they report tracking their activities, managing their stress, and having better control of their weight.
Likert Scale Program Evaluation
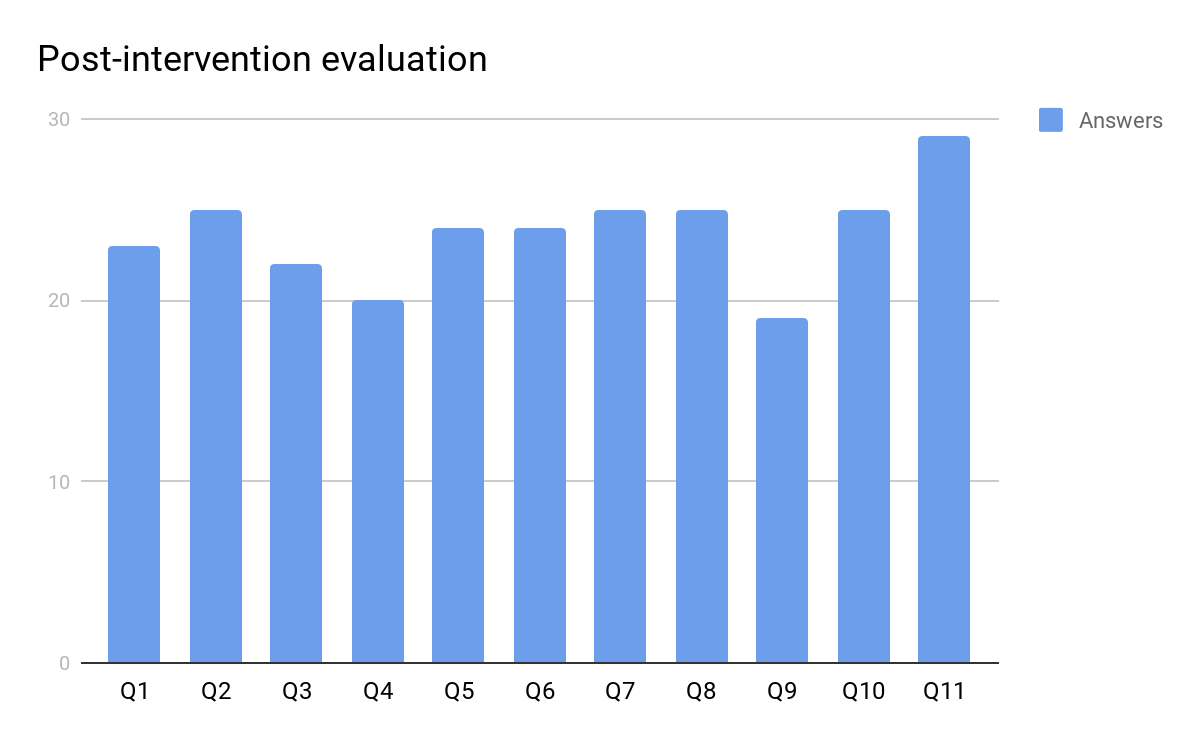
Below is the Likert scale for evaluating the program after the intervention, to gain a better understanding of the pilot’s view of this project. Results are presented in Figure 5, and notably, all pilots stated that the materials provided by the nurse were useful.
- Do you perceive the program as beneficial for your health and well-being? (strongly disagree – 1, disagree – 2, neutral – 3, agree – 4, strongly agree – 5)
- Do you think you were capable of complying with all the recommendations of this program? (strongly disagree – 1, disagree – 2, neutral – 3, agree – 4, strongly agree – 5)
- Were you able to adhere to the exercise recommendations over the course of the program (the duration; frequency of exercising)? (strongly disagree – 1, disagree – 2, neutral – 3, agree – 4, strongly agree – 5)
- Were you capable of adhering to the nutrition recommendations? (strongly disagree – 1, disagree – 2, neutral – 3, agree – 4, strongly agree – 5)
- Do you perceive this intervention as beneficial for your self-efficacy relating to weight management? (strongly disagree – 1, disagree – 2, neutral – 3, agree – 4, strongly agree – 5)
- Do you belive that your knowledge about nutrition and exercise has improved to enable an effective self-management after the program is over? (strongly disagree – 1, disagree – 2, neutral – 3, agree – 4, strongly agree – 5)
- What is your current energy level? (very low -1, low – 2, standard – 3, high – 4, very high – 5)
- What is your current stress level? (very high -1, high – 2, neutral – 3, low – 4, very low – 5)
- Has your body image improved after this program? (strongly disagree – 1, disagree – 2, neutral – 3, agree – 4, strongly agree – 5)
- Do you belive that you lost a substantial amount of weight over the course of this program? (strongly disagree – 1, disagree – 2, neutral – 3, agree – 4, strongly agree – 5)
- Has your daily physical activity after the program increased? (strongly disagree – 1, disagree – 2, neutral – 3, agree – 4, strongly agree – 5)
Open-Ended Question
- Q1. Do you think that the guide provided by your nurse (including the bouquet, meal plan, exercise recommendations) was useful? (Yes/no or other explanation).
Conclusion
Overall, as an advanced practice nurse, I benefited greatly from this program because I was able to carry out the review of academic literature on obesity management specific to the pilot population. The literature review suggests that obesity is a problem in Hongkong and that approximately fifty per cent of pilots working here have weight issues, with 14% having an obesity diagnosis. This is an issue mainly because excess weight endangers the health of these people, with an increased risk of heart disease or sleep apnoea.
This can either lead to their suspension from professional practice until their weight problem is addressed or endangerment of passengers travelling via commercial airlines, since pilots’ work requires maximum concentration and exceptional health. A such, this program addressed one significant gap the exists in aviation-specific medicine – effective obesity management through behavioural change and education of nurses who work in the clinic to ensure that they are capable of using an evidence-based approach to the management of patients who have access weight.
This project used the HPM and Donabedian’s models to approach the issue of nutrition and exercise tailored towards the challenging work conditions of pilots. Additionally, the GIBBS reflective cycle was applied to analyze the problem in the context of the pilot clinic and create an appropriate action plan. As a result, a two-hour workshop for nurses was designed, and their knowledge of obesity management has improved.
Over the course of one year, all five participants achieved a substantial reduction in their body weight and consequentially their BMI, with Patient one decreasing his BMI from 27 to 23, Patient 2 from 35 to 25, Patient 3 from 30 to 24, Patient 4 from 31 to 29, and Patient 5 from 38 to 35.
References
Bhat, K. G., Verma, N., Pant, P., & Singh Marwaha, M. P. (2019). Hypertension and obesity among civil aviation pilots. Aerospace Medicine and Human Performance, 90(8), 703–708. doi:10.3357/amhp.5374.2019
Blakemore, E. (2018). Doctors should send obese patients to diet counseling, panel says. But many don’t.
Caldwell, J. A., Mallis, M. M., Caldwell, J. L., Paul, M. A., Miller, J. C., & Neri, D. F. (2009). Fatigue countermeasures in aviation. Aviation, Space, and Environmental Medicine, 80(1), 29–59. doi:10.3357/asem.2435.2009
Cao, X., MacNaughton, P., Cadet, L., Cedeno-Laurent, J., Flanigan, S., Vallarino, J., … Allen, J. (2019). Heart rate variability and performance of commercial airline pilots during flight simulations. International Journal of Environmental Research and Public Health, 16(2), 237. doi:10.3390/ijerph16020237
Causse, M., Chua, Z., & Rémy, F. (2019). Influences of age, mental workload, and flight experience on cognitive performance and prefrontal activity in private pilots: A fNIRS study. Scientific Reports, 9(1), 1-10. doi:10.1038/s41598-019-44082-w
Change for health. (n.d.). Web.
Chen, X., Xie, L., Liu, Y., Chen, D., Yu, Q., Gan, X., & Yu, H. (2016). Metabolic syndrome and periodontal disease among civilian pilots. Aerospace Medicine and Human Performance, 87(12), 1016–1020. doi:10.3357/amhp.4654.2016
De Souza Palmeira, M. L., & Cristina Marqueze, E. (2016). Excess weight in regular aviation pilots associated with work and sleep characteristics. Sleep Science, 9(4), 266–271. doi:10.1016/j.slsci.2016.12.001
Gupta, C. C., Coates, A. M., Dorrian, J., & Banks, S. (2018). The factors influencing the eating behaviour of shiftworkers: What, when, where and why. Industrial Health, 57(4), 419-453. doi:10.2486/indhealth.2018-0147
Healthy diet. (2018). Web.
Healthy people. (n.d.). Web.
Hood, M. M., Corsica, J., Cvengros, J., & Wyatt, J. (2013). Impact of a brief dietary self-monitoring intervention on weight change and CPAP adherence in patients with obstructive sleep apnea. Journal of Psychosomatic Research, 74(2), 170–174. doi:10.1016/j.jpsychores.2012.12.006
Hood, M. M., Nackers, L. M., Kleinman, B., Corsica, J., & Katterman, S. N. (2014). Dietary self-monitoring in patients with obstructive sleep apnea. Behavioral Medicine, 40(4), 154–158. doi:10.1080/08964289.2013.842534
Lord, D., & Conlon, H. A. (2018). Cardiovascular risk factors in airline pilots. Workplace Health & Safety, 20(10), 1-4. doi:10.1177/2165079917751478
Obesity. (2019). Web.
Raynor, H., Thomas, J., Cardoso, C., Wojtanowski, A., & Foster, G. (2019). Examining the pattern of new foods and beverages consumed during obesity treatment to inform strategies for self-monitoring intake. Appetite, 132, 147-153. doi:10.1016/j.appet.2018.10.018
Snodgrass, S. J., Guest, M., Kable, A. K., James, C., Ashby, S. E., Plotnikoff, R. C., & Collins, C. E. (2016). Weight management advice for clients with overweight or obesity: Allied health professional survey. Healthcare, 4(4), 85. doi:10.3390/healthcare4040085
Sykes, A. J., Larse, P., Griffith, R., & Aldington, S. (2012). A study of airline pilot morbidity. Aviation, Space, and Environmental Medicine, 38(10), 1001-1005.
Towards 2025. (2018). Web.
Xanthopoulos, M. S., Berkowitz, R. I., & Tapia, I. E. (2018). Effects of obesity therapies on sleep disorders. Metabolism, 84, 109–117. doi:10.1016/j.metabol.2018.01.022
Zhao, J., Su, C., Wang, H., Wang, Z., & Zhan, B. (2018). New evidence on the effect of medical insurance on the obesity risk of rural residents: Findings from the China health and nutrition survey (CHNS, 2004-2011). International Journal of Environmental Research and Public Health, 15(2), 383. doi:10.3390/ijerph15020383
Appendix: Workshop Presentation