Nurse-to-Patient Ratio (NPR): Issue Description
- Nurse-to-Patient Ratio (NPR): correlation between the number of nurses and patients in a healthcare facility;
- NPR can be viewed as a quality indicator since it is required to have a specific number of nurses to manage patients’ needs;
- Because of a recent NPR drop, quality management tools will have to be incorporated into the nursing setting.
The Nurse-to-Patient Ratio (NPR) is the correlation between the number of nurses and that one of patients in a specific healthcare facility. Because of the lack of qualified staff, high demands and poor workplace environment, the NPR has been dropping greatly over the past few years (Giammona et al., 2016). Therefore, the quality of nursing services has been on the decline for a continuous period (Giammona et al., 2016). The introduction of the measures that will contribute to a rapid increase in the NPR rates and, thus, the improvement in the quality of nursing services, is necessary.
NPR from the Six Sigma Model Perspective: Description
- Positive change of the NPR is crucial to the quality of nursing services;
- The Six Sigma framework will have to be considered as the primary tool;
- The DMAIC (Define, Measure, Assess, Improve, and Control) approach will be used to encourage change;
- Thus, all six domains of healthcare quality will be addressed (Agency for Healthcare Research and Quality, 2015).
The promotion of positive change in the nursing setting is crucial. Particularly, a redesign of the existing schedule, as well as the rearrangement of roles and responsibilities among nurses, will have to be viewed as a necessity. The use of the Six Sigma model will have to be adopted to promote changes in the target environment and encourage nurse to accept new quality standards. The adoption of the DMAIC framework (see Fig. 2) will have to be viewed as an opportunity to encourage a continuous change in the realm of a nursing facility.
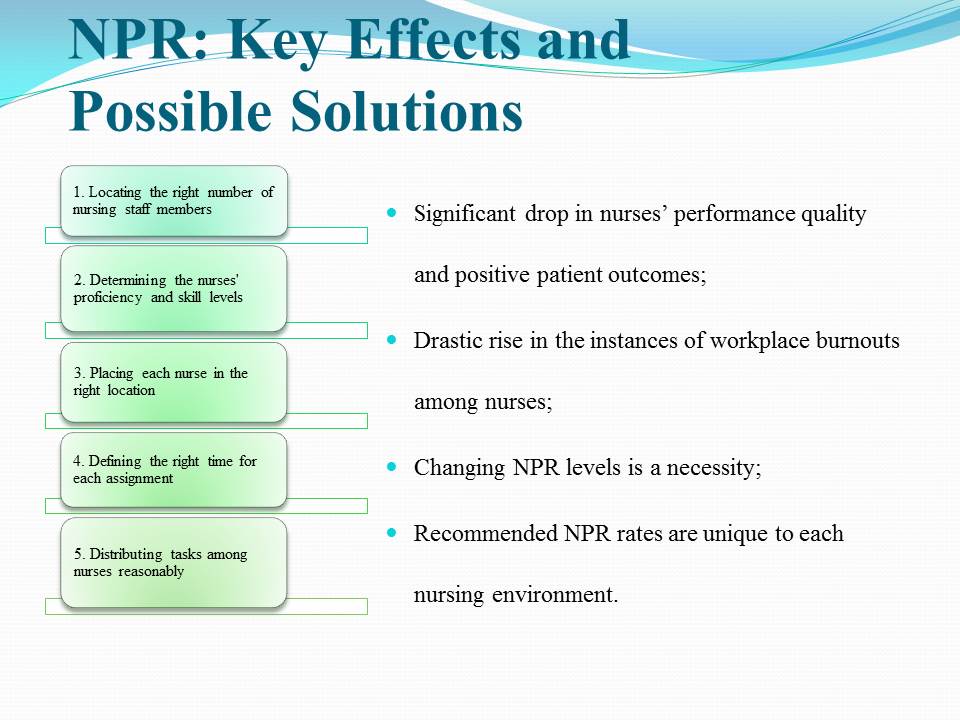
NPR: Key Effects and Possible Solutions
- Significant drop in nurses’ performance quality and positive patient outcomes;
- Drastic rise in the instances of workplace burnouts among nurses;
- Changing NPR levels is a necessity;
- Recommended NPR rates are unique to each nursing environment.
The NRP has a drastic effect on the quality of nursing services due to the lack of competent staff, the schedule issues, and the increasingly high pressure experienced by nurses. As a result, an even greater drop in the quality of nurses’ performance can be expected due to the possibility of a workplace burnout (Cho et al., 2015).
Based on the Acuity-Based Staffing Model (ABSM) (see Fig. 1 above), it is reasonable to assume that the choice concerning the number of nurses that the target environment requires must be made on a case-by-case basis (Vortherms, Spoden, & Wilcken, 2015).
- Locating the right number of nursing staff members;
- Determining the nurses’ proficiency and skill levels;
- Placing each nurse in the right location;
- Defining the right time for each assignment;
- Distributing tasks among nurses reasonably.
Application of the Acuity-Based Staffing Model (ABSM)
- ABSM will allow rearranging the tasks and responsibilities based on nurses’ skills and proficiency levels;
- ABSM will serve as the means of maintaining a reasonable approach toward staffing;
- ABSM will lead to a gradual drop in the rates of workplace burnouts among nurses;
- ABSM will contribute to an increase in the quality levels of the provided nursing services.
The adoption of the ABSM-based approach will supposedly help improve the current issue regarding the NPR by rearranging roles and responsibilities among nurses, as well as changing the current approach toward staffing. The framework will help make sure that the tasks and responsibilities assigned to nurses match their level of proficiency and are manageable. Thus, a rapid drop in the number of workplace burnouts can be expected in the contemporary nursing setting.
Proposal for Improvement
- The problem concerning the NPR levels must be recognized;
- The ABSM tool must be introduced to the nursing setting;
- The roles and responsibilities of nurses must correlate with their competence levels.
It is strongly advised that the introduction of the ABSM framework should be viewed as a necessity. The specified tool will help reduce the pressure levels among nurses by reconsidering the current strategy toward assigning specific roles and responsibilities to nurses. The new and improved strategy based on correlating the number and difficulty of tasks with the level of skills that a nurse displays will ultimately lead to a massive improvement in the service quality and well-being levels among nurses.
Expected Outcomes
- Improved approach toward distributing roles and responsibilities among nurses;
- Sharp rise in the number of positive patient outcomes;
- Enhanced opportunities for meeting patients’ needs;
- Rapid drop in the number of workplace burnouts.
It would be wrong to assume that the ABSM will help eradicate the issue of low NPR completely. However, it is expected that the approach will serve as the means of controlling the problem. The framework will become the foundation for approaching each case of NPR individually and interpreting the results of the correlation between the number of nurses and that one of patients on a case-by-case basis. Consequently, the unique needs of patients from any nursing setting will be recognized and addressed successfully. Furthermore, the redesign of the approach toward distributing roles and responsibilities among nurses is bound to lead to a significant drop in workplace burnout rates among nurses (Barton, 2013).
References
Agency for Healthcare Research and Quality. (2015). The six domains of health care quality. Web.
Barton, N. (2013). Acuity-based staffing: Balance cost, satisfaction, quality, and outcomes. Nurse Leader, 11(6), 47-64.
Cho, E., Sloane, D. M., Kim, E. Y., Kim, S., Choi, M., Yoo, I. Y., … Aiken, L. H. (2015). Effects of nurse staffing, work environments, and education on patient mortality: An observational study. International Journal of Nursing Studies, 52(2), 535-542.
Giammona, S., Arena, G., Calò, M., Barone, M. B., Scelsa, D., Lepre, A., … Schlenk, E. A. (2016). Nursing workload and staff allocation in an Italian hospital: A quality improvement initiative based on nursing care score. CentralEuropean Journal of Nursing and Midwifery, 7(2), 420-427.
Vortherms, J., Spoden, B., & Wilcken, J. (2015). From evidence to practice: Developing an outpatient acuity-based staffing model. Clinical Journal of Oncology Nursing, 19(3), 332-337.