Epidemiology
- PCOS – hypertrophied ovaries with multiple tiny cysts.
- Highly prevalent: affects 6-10% of women (Barbosa, de Sa, Rocha, & Arbex, 2016).
- Higher incidence in Hispanic women (>20% affected).
- Higher prevalence in women with morbid obesity (28% vs. 5.5%) (Christensen et al., 2013).
- PCOS accounts for:
- 75% of infertility cases.
- Hyperandrogenism (95%).
Etiology/Causes
- Etiology of PCOS is not well understood.
- Most common causes – endocrine disorders:
- Hypothalamic-pituitary axis impairment,
- Abnormal ovarian steroidogenesis;
- Insulin resistance.
- Impaired pituitary function causes altered LH/FSH balance – hyperandrogenism.
- High testosterone levels in affected women indicate impaired steroidogenesis.
- Insulin resistance affects receptors & enzymes controlling ovarian testosterone production (Conway et al., 2014).
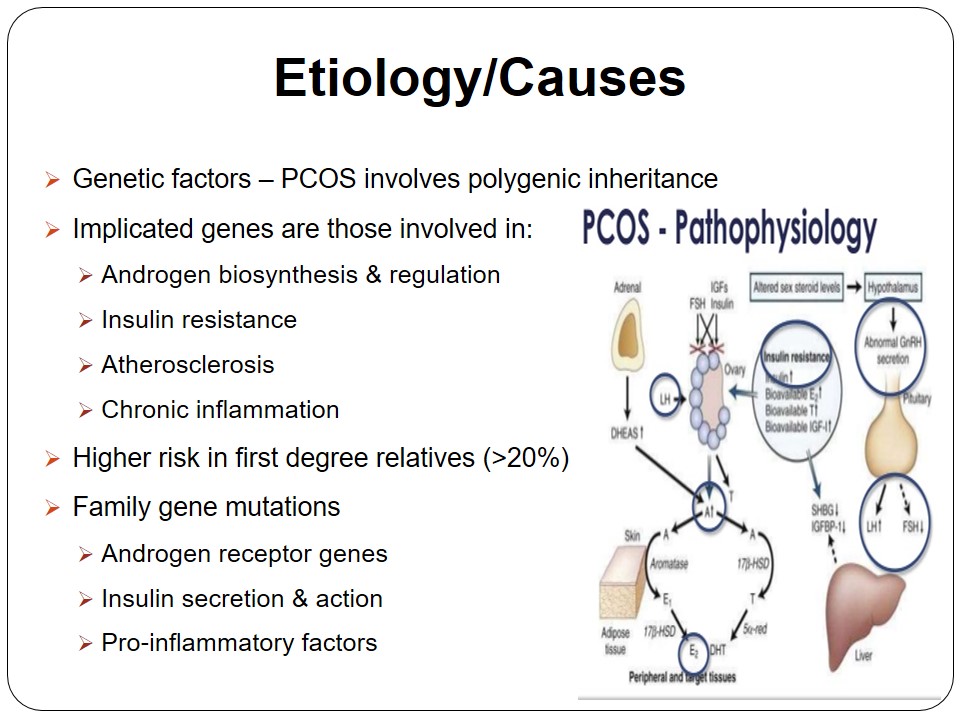
- Genetic factors – PCOS involves polygenic inheritance.
- Implicated genes are those involved in:
- Androgen biosynthesis & regulation;
- Insulin resistance;
- Atherosclerosis;
- Chronic inflammation.
- Higher risk in first degree relatives (>20%).
- Family gene mutations:
- Androgen receptor genes;
- Insulin secretion & action;
- Pro-inflammatory factors.
- Environmental factors – least frequent cause of PCOS.
- Co-morbidity – over 50% of females with PCOS are obese (Conway et al., 2014).
- Related metabolic syndromes include:
- Obesity;
- Insulin resistance.
- Increased glucose intolerance – T2DM development.
- Definition of PCOS phenotype includes environmental factors.
The etiological agents in PCOS development are not fully known. It is considered a multigenic disorder with three possible causes: “hypothalamic-pituitary axis dysfunction, abnormal steriodogenesis, and insulin resistance” (Barbosa et al., 2016, p. 60). Impairment in the pituitary/hypothalamus function increases luteinizing hormone (LH) levels relative to follicle-stimulating hormone (FSH) concentrations, increasing the risk of hyperandogenism and amenorrhea (Conway et al., 2014). Abnormal ovarian steroidogenesis results in higher testosterone levels. Insulin resistance due to genetics or lifestyle affects the receptors and enzymes controlling ovarian androgen secretion, increasing the PCOS risk.
Genetic factors have also been implicated in PCOS pathogenesis. Different phenotypes of this disease are linked to genes involved in ovarian androgen synthesis and regulation (Barbosa et al., 2016). Further, genetic variants implicated in insulin resistance, atherosclerosis and chronic inflammation also cause PCOS in first-degree relatives. Such polymorphisms affect androgen and insulin receptors.
The etiology of PCOS also implicates environmental factors – metabolic syndromes. Obesity – abnormal BMI due to unhealthy lifestyle – occurs as a co-morbid condition in 50% of women diagnosed with PCOS (Conway et al., 2014). Insulin resistance is another metabolic syndrome associated with PCOS development. Therefore, the diagnosis of PCOS often involves screening of obesity and insulin resistance in the female patient.
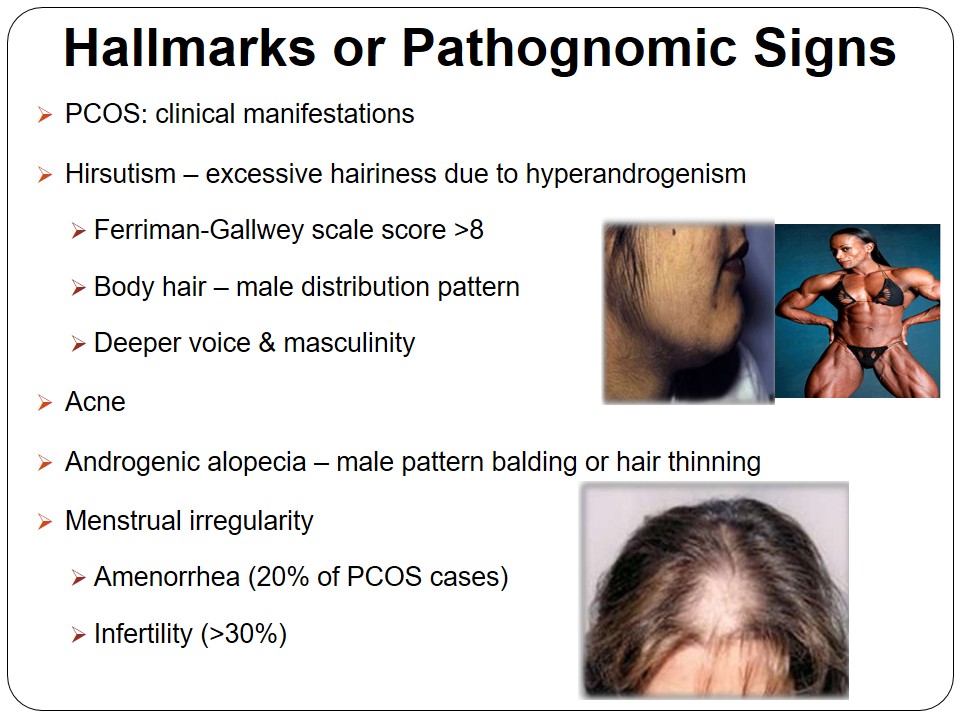
Hallmarks or Pathognomic Signs
- PCOS: clinical manifestations.
- Hirsutism – excessive hairiness due to hyperandrogenism:
- Ferriman-Gallwey scale score >8;
- Body hair – male distribution pattern;
- Deeper voice & masculinity.
- Acne.
- Androgenic alopecia – male pattern balding or hair thinning.
- Menstrual irregularity:
- Amenorrhea (20% of PCOS cases).
- Infertility (>30%).
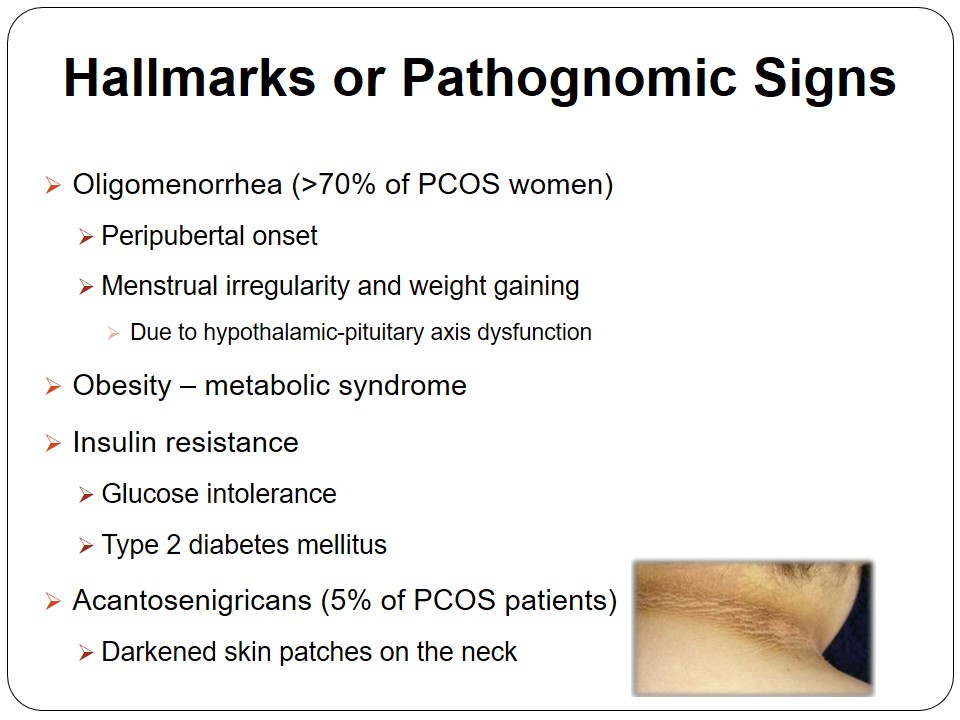
- Oligomenorrhea (>70% of PCOS women):
- Peripubertal onset.
- Menstrual irregularity and weight gaining.
- Due to hypothalamic-pituitary axis dysfunction.
- Obesity – metabolic syndrome.
- Insulin resistance:
- Glucose intolerance.
- Type 2 diabetes mellitus.
- Acantosenigricans (5% of PCOS patients)
- Darkened skin patches on the neck.
The most common clinical manifestation of PCOS is hirsutism. Hirsute women are hairy on the chest, face, and arms/legs just like males. Hirsutism is attributed to increased 5α-reductase activity (Witchel et al., 2015). PCOS also manifests as acne or facial lesions, hyperandrogenism – deeper voice and muscles – and androgenic alopecia (balding). Other pathognomic signs include menstrual abnormalities such as amenorrhea and infertility due to LH/FSH imbalance.
Oligomenorrhea, a condition characterized by infrequent menstrual flow, affects over 70% of women with PCOS (Witchel et al., 2015). The underlying cause is the enhanced androgen biosynthesis in the ovary due to impaired hypothalamic-pituitary function. The metabolic signs or symptoms of PCOS include obesity and insulin resistance, which causes glucose intolerance and T2DM in patients. Women with PCOS also present with acantosenigricans – dark skin patches on various parts of the body.
Diagnostic Criteria
- Androgen Excess & PCOS Society (AE-PCOS) criteria:
- Positive diagnosis includes all of the following:
- Androgen excess;
- Ovulatory dysfunction – polycystic ovary;
- Exclusion of other etiologies, e.g., Thyroid dysfunction.
- Androgen excess – clinical hyperandrogenism & hyperandrogenemia (AE-PCOS, 2016):
- Hyperandrogenism: hirsutism, acne & androgenic alopecia;
- Hyperandrogenemia: testosterone bioavailability.
- Ovulatory dysfunction:
- Menstrual cycle irregularity – manifests clinically as amenorrhea & anovulation;
- Ovarian dysmorphology – polycystic ovary confirmed through ultrasound.
- Positive diagnosis includes all of the following:
- Other Diagnostic Criteria:
- Rotterdam Criteria:
- Oligo-ovulation and/or anovulation;
- Clinical/biochemical signs of hyperandrogenism;
- Polycystic ovaries – confirmed through ultrasound.
- Transvaginal ultrasound:
- >12 follicles in ovaries;
- Each follicle measures 2-9mm thick;
- Enlarged ovary (>10 mL).
- NIH Criteria:
- Menstrual irregularity due to oligo/anovulation;
- Signs of hyperandrogenism;
- Exclude other etiologies related to the two.
- Rotterdam Criteria:
- Etiologies excluded in PCOS diagnosis: AE-PCOS criteria:
- Thyroid disease;
- Acromegaly;
- Hyperprolactin;
- Adrenal hyperplasia;
- Cushing’s syndrome;
- Androgen producing tumors;
- Simple obesity;
- Virilizing Ovarian neoplasm.
According to the Androgen Excess/PCOS Society (AE-PCOS) criteria released in 2016, PCOS diagnosis involves two considerations: “androgen excess and ovulatory dysfunction” (para. 2). A woman with androgen excess presents with either hyperandrogenism or hyperandrogenemia – elevated testosterone bioavailability (AE-PCOS, 2016). On the other hand, ovulatory dysfunction manifests as menstrual irregularity (amenorrhea and anovulation) and polycystic ovary (AE-PCOS, 2016).
The other PCOS diagnostic criteria include the Rotterdam and NIH criteria. A positive diagnosis using the Rotterdam criteria requires the presence of two out of the three signs: oligo-ovulation/anovulation, hyperandrogenism, and/or polycystic ovaries confirmed through ultrasound (Legro et al., 2013). PCOS is confirmed if a transvaginal ultrasound reveals more than 12 follicles in either ovary that measure 2-9mm thick each and an enlarged ovary (>10 mL).
Correct PCOS diagnosis requires the exclusion of related medical etiologies. The other causes of hyperandrogenism and menstrual irregularity that require exclusion include Cushing’s syndrome, hyperprolactin, thyroid disease, acromegaly, obesity, etc.
Question 1
What are the potential benefits of PCOS to the affected female population?
- PCOS affects 5-10% of females – selective advantage.
- Improved species survival due to:
- Retention of calories and increased adiposity that enhances survival in hostile conditions.
- Lower risk of osteopenia & osteoporosis.
- The pregnancy issue.
Having the PCOS gene confers certain selective advantages to the affected women. It may lead to improved survival during winter or famine due to increased adiposity, i.e., PCOS related obesity. Further, PCOS lowers the risk of osteopenia and osteoporosis due to insulin resistance (hypoinsulinemia), which preserves bone mass density in affected women (Katulski et al., 2014). PCOS accounts for over 90% of infertility cases. Thus, pregnancy is not an issue in PCOS patients.
Question 2
What are the long-term sequelae linked to PCOS in women?
- Type II Diabetes Mellitus:
- Due to insulin resistance.
- Dyslipidemia:
- Due to simple obesity or higher BMI in PCOS patients.
- Endometrial Carcinoma.
The primary long-term co-morbidity of PCOS is type II diabetes mellitus (T2DM). Insulin resistance and obesity are the two hallmarks of PCOS. Therefore, prolonged insulin resistance increases the risk of T2DM development in PCOS patients. Dyslipidemia (abnormal lipid levels in the blood) may occur in obese PCOS patients. Another long-term sequelae related to PCOS is endometrial carcinoma or uterine cancer.
References
Androgen Excess/PCOS Society [AE-PCOS]. (2016). Polycystic ovary syndrome (PCOS): A reference for healthcare providers. Web.
Barbosa, G., de Sa, L. B., Rocha, D. R., & Arbex, A. K. (2016). Polycystic ovary syndrome (PCOS) and fertility. Open Journal of Endocrine and Metabolic Diseases, 6, 58-65. Web.
Christensen, S. B., Black, M. H., Smith, N., Martinez, M. M., Jacobsen, S. J., Porter, A. H., & Koebnick, C. (2013). The prevalence of polycystic ovary syndrome in adolescents. Fertility and Sterility, 100(2), 470-477. Web.
Conway, G., Dewailly, D., Diamanti-Kandarakis, E., Escobar-Morreale, H. F., Franks, S., Gambineri, A., … Yildiz, B. O. (2014). The polycystic ovary syndrome: A position statement from the European Society of Endocrinology. European Journal of Endocrinology, 171(4), 1-29.
Engmann, L., Jin, S., Legro, R. S., Polotsky, A. J., Hansen, K. R., Coutifaris, C., … Santoro, N. (2017). Racial and ethnic differences in the polycystic ovary syndrome metabolic phenotype. American Journal of Obstetrics and Gynecology, 216(5), 493-401. Web.
Katulski, K., Slawek, S., Czyzyk, A., Podfigurna-Stopa, A., Paczkowska, K., Ignaszak, N., … Meczekalski, B. (2014). Bone mineral density in women with polycystic ovary syndrome. Journal of Endrocrinological Investigation, 37(12), 1219-1224. Web.
Legro, R. S., Arslanian, S. A., Ehrmann, D. A., Hoeger, K. M., Murad, M. H., Pasquali, R., & Welt, C. K. (2013). Diagnosis and treatment of polycystic ovary syndrome: An Endocrine Society clinical practice guideline. Journal of Clinical Endocrinology and Metabolism, 98(12), 4565-4592. Web.
Witchel, S. F., Oberfield, S., Rosenfield, R. L., Codner, E., Bonny, A., Ibanez, L., … Lee, P. A. (2015). The diagnosis of polycystic ovary syndrome during adolescence. Hormone Research Paediatrics, 83, 376–389. Web.