Specific Aims
The purpose of this study is to examine how different factors contribute to the re-admission of CHF Medicare patients. The major focus of this study will be to scrutinize the current strategies used in Medicare in addressing the problem of CHF patients. In addition, factors that cause these patients to come repeatedly in the Medicare needs consideration in order to come up with a more workable strategy to avert the situation. Am interested to know why there is an increasing rate of readmission in our Medicare while the government is pumping much money into the health sector.
Having worked closely with some doctors and nurses during my community work has given me substantial knowledge of some of the main problems facing the CHF patients and this study will buffer the measures taken by Medicare in attending to these patients. This research seeks to critically evaluate, and analyze the current situation with the aim to give solutions that will improve medication that will, in turn, reduce the readmission rate. This paper will address specific factors related to preventable re-admissions among Medicare patients with CHF.
The specific aims of this study will be:
- to highlight the rate of CHF patients readmission in Medicare
- To address possible causes of these readmissions.
- To quantify medication problems related with readmission of the patients
Research questions
- What are the main contributing factors that cause readmission of critical heart failure (CHF) patients who are under the Medicare program in the United States?
- How does medical practitioners’ negligence increase the rate of readmission?
- What is the possible role should CHF patients play in order to reduce prevalence to disease reoccurrence?
- How do socio-environmental factors associated with the increasing readmission rate among Medicare patients suffering from CHF?
Justification
A careful review of the literature found that there is an increasing incidence of readmission of congestive heart failure (CHF) patients in the United States. The previous studies done failed to address the current trend in disease prevalence to patients who had been diagnosed with other related diseases such as Noncardiac comorbidities Hypertension that have remarkably increased from 30% in 1994 to 56% in 2006 (Bueno et al., 2010).
An additional trigger of this study was the increased readmission of Medicare patients hence raising a question whether there is quality and reliability of medical services across New York and the larger United States. This study will therefore address additional issues relating to role played by medical personnel that increase rate of readmission of CHF patients.
Background & Significance
Following the decision by Centers for Medicare and Medicaid services (CMS) on June 2009 to publicly reporting the hospitals that registered high rate of readmission through their website formed the foundation of my study. The CMS could no longer run away from the fact that the rate of readmission had become rampant for patients who had earlier hospitalized and discharged of Pneumonia, Acute Myocardial Infarction, or Heart Failure. It stated that one fifth of discharged patients suffering from the above diseases got readmission within 30 days, which is a critical problem that needs a keen study. This situation met many challenges with the enacting of patient protection and affordable care act where questioning of hospitals on this rate of readmission as well as payment adjustment by 2013 continues.
Medicare payment advisory commission is worried of pneumonia, CHF, and AMI costs incurred by the patients during hospitalization as well as increased potentially preventable readmissions. Recommendation to Congress and CMS required policies implementations in order to counteract this trend. However, many debates have taken place on hospital readmissions and much research on means of preventing readmission from occurring takes a high demand.
Statistics shows that 13% of inpatients in the United States consume more than half the medical bill in the facility they are being attended. In 2009, Centers for Medicare and Medicaid Services (CMS) reported that those patients with Medicare had likelihood of being readmitted one month after their inpatient stay. The blame to this trend reflects the prevailing practices among medical facilities as well as some attributes that put blame on some CHF patients. To manage CHF, medical care practitioners agree that all stakeholders must play their part diligently (Centers for Medicaid and Medicare, 2009).
According to Minott’s study of the readmission rate in the United States, he revealed that hospitalization was the most expensive type of care with the healthcare continuum (Minott, 2008). The scholar noted that the rate accounts for about 31% of medical care bill reported in the United States. The high cost of treatment does not necessary mean that the quality of medical care services are low but acts as an indication that there is a certain inconsistency in medical care provision. New York has registered the highest number of readmission of patients suffering from CHF (Minott, 2008).
A study carried out by Ashton et al. (1995) revealed a comparison of some readmission rates on different disease. The results revealed that patients suffering from heart failure were more prone to readmission. One out of the seven discharged diabetic patient was readmitted, one out of twelve patients discharged of obstructive lung cancer was readmitted, while one out of five heart failure patient discharged was readmitted (Ashton et al., 1995). This reveals how the CHF patients need care so that we curd danger to the patient life resulting from carelessness behaviors preventable at early stages.
Many studies to determine whether there is association between the quality of inpatient care and early readmission have attracted attention of many researchers who include; Ashton, Del Junco, Souchek, Wray and Mansyur, who conducted a study on this topic (Ashton et al., 1997). According to Epstein (2009), the increased readmission rate is an indication of some weaknesses in the Medicare care provision that the government should address with emergency. In these attempts, no single study has proved this hypothesis. Data collected by these researchers have differed in terms of credibility since after analysis, the preventability of readmission by improving quality inpatient ranged from 9% to 48%. Not only the researchers have failed to prove the possibility of low-quality inpatient as cause of readmission but even the analyst who come up with different conclusions using same data. Therefore, although low quality inpatient can contribute to readmission, no guarantee that improvement of inpatient services will deliver better results.
According to Goldfield et al. (2008), there is high correlation between readmission rate and the quality of medical service given at the first stage to CHF patients. In their study, they noted that those Medicare patients attended by incompetent medical practitioners had high tendency of developing complications that calls for readmission (Goldfield et al, 2008). Simmons was keen to note high correlation between poor care of CHF treatment and chances of readmission. In addition, patients treated with less attention to the condition they were suffering from had the tendency of getting a readmission. According to the scholar, other than giving CHF attention, those patients attended for other medical conditions but attention on the fact that they are as well suffering from CHF ignored are more likely to develop complications seeking for further readmission (Simmons, 2009).
Hodges in her study related CHF readmission with medical factors that included uncontrolled hypertension among other infections, lack of support from the society and patients’ failure to adhere to medications, diet and adaptation to the changing lifestyle (Hodges, 2009). In addition, she blamed the premature discharging plans and lack of teachings to patients and family member that could have greatly contributed to readmission that have increasingly observed at the initial hospitalization among the CHF patients who were older adults. Juan et al. (2009) also echoed this sentiment where they suggested that adoption of comprehensive discharging system that integrates medical counseling and follow-ups could minimize the rate of readmission. In their study, they proposed combination of implantable cardiac devices with optimal medical therapy, which have positively averted the earlier trend to a reduced readmission. Proctor et al. (2000) discovered that 33% to 40% of the older adults diagnosed with CHF were susceptible to readmission within the first three months after discharge. It must be of common interest to put into consideration of this factor since most researchers have found it as a possible contributor to readmission and hence if well addressed we can prevent the current trend to a better solution.
Some researchers have noted poor coordination of services before and after discharge as main source of readmission. CHF patients are sensitive and need careful handling by the medical facility attended as well as home care service providers who will follow the release. The role of the government to intervene in the situation through incentives to reduce the duration of stay that patients have in a certain medical care facility aimed at reducing treatment but to some extent it have been challenged due to poor medication. Bill introduction in 1989 in the United State aimed at establishing a cost-based payment mechanism for patients with the main aim of reducing the duration of stay in hospitalization. Despite the bill there was an increased readmission rate believed to have resulted from those patients who had been released prematurely (Simmons, 2009).
On the other hand, there is patients’ accusation for contributing to readmission through non-adherence to the discharge plan and medication compliance. No matter how the medical care providers work extra hard in fighting the CHF, without the cooperation of the patient can ruin this effort. Patients’ failure to adhere to their required roles an objectives increases chances of failure in the provision that leads to readmission.
According to Medicare Payment Advisory Commission (Med PAC), the changes in medical bill settlement as adopted by Medicare patients may be a contributing factor where medical facilities that have profit motive as their main agenda taking the short cut of discharging CHF patients prematurely. In comparison, Private patient spends more money for their health services compared to patients who relies in Medicare system. In addition, the procedure and method of getting the reimbursement is tiresome and sometime irritating. United States taxpayers incurs cost a total of $15 Billion through readmission of CHF patients. These high expenditures triggered the authority to develop a program called Deficit Reduction Act (DRA) of 2005 whose mandate was to regulate the payment of performance inactive. According to Deficit Reduction Act (DRA) of 2005, the aim was to persuade the government to undertake measures that would have prevented medical facilities in raising additional charges in the case of readmission (Medicare Payment Advisory Commission (Med PAC), 2007).
CMS must have cited Social-economic situation of the patients to contribute to readmission of CHF patients. They indicated that there is close link between the living condition of CHF patients and readmission rate. The study had suggested that the readmission rate is higher among the Black demographic population, which in most cases is the low class and middle class population in the United States. The study by CMS suggested that those hospitals whose patients received no information on how to manage their condition after their release had high risk of readmission with the same condition (CMS, 2008)
Previous researches have focused the relationship between medical care quality and rate of readmission but the studies are general in nature and rarely concentrate on one condition or class of patients. The Uniqueness of this research focus on zeroing in on those patients that have Medicare cards and are suffering from CHF. The main reason for the narrower approach is to assist the researcher attain more concrete and comprehensive information that can add more value to the available literature (Moullin, 2007). The factors that lead to poor provision of the medical care are multiple and concentration on one might not offer a lasting solution to the problem (Epstein, 2009).
The study carried out by Juan, James and Jamie (2009) elevated this through criticizing earlier studies on readmission rates that limited to single-center experiences over a period of several years. In return, we may get useful information but have shortcomings in addressing the population in general as well as the prevailing practices.
Theoretical/Conceptual Framework
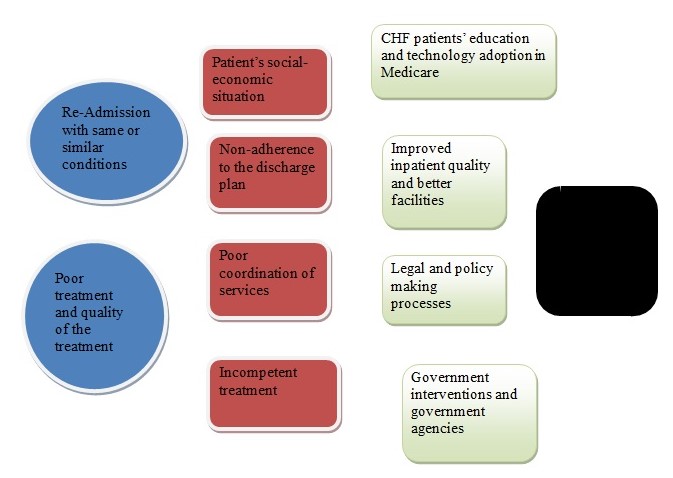
There is no doubt that increased rate of CHF patients have caused a cause for alarm to medical personnel, government, government agencies as well as the patients themselves. This study comes at the correct time and it is worth investigating the causes of this readmission as well as devising possible means to minimizing or preventing reoccurrence of readmission of the CHF patients. It is worth carrying out this study since it will save both government and the CHF patients some money usable for other purposes other than attending readmitted patients.
If the current situation is something to go by, then we face a danger of increased readmission rate due to combination of different factors related to quality in medical care services. This increased rate may serve as gauging rate of services quality delivery. According to WHO (2009), many factors have led to readmission that includes those factors that can be attributed directly with medical care facilities, patients and societal factors can also be attributed to the readmission rate. Patients should be well informed on how to care for their condition and those that are willing to comply with the advises given are at lesser risk of readmission (World Health Organization, 2009).
It was clear to me that Different medical facilities may have their specific factors that lead to readmission. This calls for unique attributes in mind that there is need to have performance measures as tools to gauge the degree of quality and affordability of medical care services given by particular medical facility. In the case of hospital readmission, the developed performance measures should be elaborated enough to give guideline and point areas that need improvement within certain medical facility US (Department of Health and Human Services, 2009).
The United States of America medical bill makes second largest portion of its budget from security and it approximately accounts for 16% of the gross domestic product (GDP). According to WHO (2009), the medical care expenditures in United States is likely to be on an upward rise in the near future with some of the factors quoted to contribute as readmission rate increase. WHO advised that the government should seek for methods to offer high medical care quality and reduce the expenditure in the provision; this is the challenge that the government of United States has faced (Medicare Payment Advisory Commission, 2007).
Conceptual Model
This research adopted quantitative approach that both dependent variable and independent variables. The dependent variables are the rate of readmission among patients suffering from CHF condition in the United States. The Independent variables include quality of medical services provisions, the living condition of the patients, awareness and the rate of follow up programs, and the discharge regulations compliance rate. Data in this research relies on information contained in the New York readmission rate data and primary sources like interviews, and surveys.
References
Ashton, C.M., Del Junco, D.J., Souchek, J., Wray, N.P., & Mansyur, C.L. (1997). The association between the quality of inpatient care and early readmission: a meta-analysis of the evidence. Med Care, 35(10), 1044-1059.
Ashton, C.M., Kuykendall, D.H., Johnson, M.L. Wray, N.P., & Wu, L. (1995). The association between the quality of inpatient care and early readmission. Ann Intern Med., 122(6), 415-421.
Bueno et al. (2010). Trends in Length of Stay and Short-term Outcomes Among Medicare Patients Hospitalized for Heart Failure. JAMA, 303(21), 2141-2147.
Centers for Medicaid and Medicare. (2009). New Ratings for Americas Hospitals. Web.
Epstein, A.M. (2009). Revisiting Readmissions: Changing the Incentives for Shared Accountability. New England Journal of Medicine, 360(14), 1457-1459.
Goldfield, N.I. et al. (2008). Identifying Potentially Preventable Readmissions. Health Care Financing Review, 30(1), 75–91.
Hodges, P. (2009). Factors Impacting Readmissions of Older Patients with Heart Failure. Crit Care Nurs Q, 32(1), 33–43.
Juan, M.A., James, W.J., & Jamie, B. (2009). Current Trends in Heart Failure Readmission Rates: Analysis of Medicare Data, Clinical Cardiol, 32(1), 47–52.
Medicare Payment Advisory Commission. (2007). Payment Policy for Inpatient Readmissions: Promoting Greater Efficiency in Medicare. Web.
Minott, J. (2008). Reducing Hospital Readmissions. Academy Health. Web.
Moullin, M. (2007). Performance measurement definitions: Linking performance measurement and organizational excellence. International Journal of Health Care Quality Assurance, 20(3), 181-184.
Moullin, M. (2009). Public Sector Scorecard. Nursing Management, 16(5), 26-31.
Proctor, E., Morrow-Howell, N., Li, H., & Dore, P. (2000). Adequacy of home care and hospital readmissions for elderly congestive heart failure patients. Health Soc Work, 25, 87–94.
Simmons, J. (2009). New 30-Day Readmission Rates Listed at HHS Hospital Compare Web site. Health Leaders Media. Web.
US Department of Health and Human Services. (2009). Compare Hospital Quality. Web.