Description of the Topic and Background Information
Pressure injuries (PIs) are caused by the unrelieved pressure or shearing of body parts, which causes tissue damage to an affected person. The skin of an affected individual may appear intact, or the injury may appear as an open ulcer. Various factors, such as prolonged skin moisture, nutrition and perfusion, may potentiate the harmful effects of the injury. As seen in Figure 1, pressure injury may have various stages where skin layers can be affected at different levels.
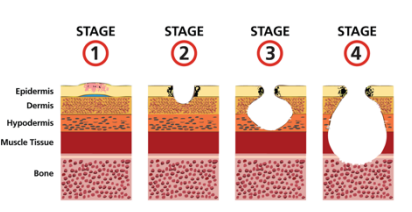
Stage 4 is the most severe one, where the bone can be affected, which increases the exacerbation rate for the affected person. PIs may lead to decreased quality of life, but 95% are preventable (Schub & Schub, 2021). In 2008, the US government, through the Centers for Medicare and Medicaid Services (CMS), ceased reimbursing facilities for treating PIs within the range of stages 3 and 4 (Schub & Schub, 2021). Risk assessment using PI assessment methodologies forms part of standard preventative ways that have been used to offer remedies for this medical problem. Patient repositioning after every 2 hours has been recommended as one o the effective clinical trial to prevent PIs. Evidence-based practices (EBPs) suggest that constant low-pressure support areas lower incidences of PIs, and sheepskin mattresses are known to offer similar results.
Significance of the Topic to Nursing Practices
Understanding the existence of pressure injuries and ways that can be used to prevent them is important in nursing practice. The topic’s significance is that it enables nurses to know the etiology, risk factors, risk assessment and delivery of prevention plans that can be effective for the patients (Gillespie et al., 2020). Additionally, the topic is significant because it enlightens the possible ways the problem can be solved, reducing the number of hospitalizations, cost of treatment and possible mortalities that can result from PIs (Sharp et al., 2019). For example, through the topic, a patient can understand why various clinical trials are put in place to prevent the deterioration of ulcers when they are ailing.
Pressure ulcers can affect any person, but they are commonly associated with adults compared to children. Through the topic, nursing practice is equipped with implementation programs that focus on preventive measures to alleviate risks revealed by using PIs assessment tools. Regarding mortality rates, PIs have a 60% probability of leading to death for older persons after they have been hospitalized and discharged after one year (Gillespie et al., 2020). Thus, the topic serves as a holistic approach to dealing with the issue from the patient, nurse, and doctor’s point of view. Nurses must be aware of the rising incidences of PIs and how to handle them to combat the underlying risks in public health (Sharp et al., 2019). Learning more about PIs aid in accurately assessing patients’ characteristics, and the knowledge can be shared with them and their colleagues.
PICOT Question
Patient, intervention, comparison, outcome and time (PICOT) questions are important in clinical strategies to solve a particular medical issue. In this case, the PICOT question is as follows; In older adults, how does manual repositioning compared to decreased mechanical load influence the prevention of pressure injuries over their ailing period? The question comprises the elements of PICOT and lies under prognosis. Under the topic, the question helps a researcher dig deep into the preventive methods that can be useful and which are more effective for normal PIs (Sharp et al., 2019). Decreasing mechanical load is an alternative when a patient cannot reposition themselves.
References
Gillespie, B. M., Walker, R. M., Latimer, S. L., Thalib, L., Whitty, J. A., McInnes, E., Lockwood, I., & Chaboyer, W. P. (2021). Repositioning for pressure injury prevention in adults: An abridged Cochrane systematic review and meta-analysis. International Journal of Nursing Studies, 3(2), 5–12. Web.
Schub, T., & Schub, E. (2021). Pressure ulcers: A patient safety issue.
Sharp, C. A., Schulz Moore, J. S., & McLaws, M.-L. (2019). Two-hourly repositioning to prevent pressure ulcers in the elderly: Patient safety or elder abuse?Journal of Bioethical Inquiry, 16(1), 17–34. Web.