Selected Issue – Universal Healthcare
- U.S. has unique healthcare system – largely privatized;
- Rising costs create barriers to access;
- Universal coverage – redistributive policy type;
- Universal healthcare prevalent topic in politics and administration;
- “Cannot be achieved without recognition of its dependence on, and consequences for, both governance and politics” (Greer & Méndez, 2015).
Most developed and developing countries in the world maintain a healthcare system which is universal or at least partially public, providing access to fundamental medical services and medications to its residents. In the United States, the government only serves as a regulator or subsidiary. There have been increased calls for universal healthcare, but the issue is strongly political and complex. Such healthcare uses the redistributive type of policy by building upon public goods for the benefit of society, benefiting less advantaged groups the most ((Denhardt, Denhardt, & Blanc, 2014). Such policy is financed from the national budget through taxation.
Impact of Organizational Resources
- National healthcare is mostly created and regulated through the Department of Health and Human Resources (HHS);
- Multiple sub-agencies engage in collaboration to drive national health initiatives;
- Sophisticated strategic planning required to coordinate in the implementation of healthcare policy;
- Organizational resources are available for implementation of universal healthcare;
- However, significantly greater funding and personnel would be required to develop and implement a national level oversight that would be required.
The HHS is a vital agency and organization in the implementation of national healthcare policy. It consists of multiple collaborating subagencies within that strategically plan large-scale healthcare initiatives. The organization has significant resources at its disposal but relies on cooperation with other federal and state agencies as well as private entities to achieve its objectives which may be potentially challenging to such enormous changes as universal care.
Impact of Human and Budget Resources
- Human resources drive implementation of healthcare policy;
- Dedicated HR department at HHS agency with systemic approach to management;
- Offices focused on program management, resource management, and operations vital to support the national healthcare system;
- Budget for HHS approved annually by Congress;
- Each department and sub-agency with HHS must submit proposals and justification;
- Concern that universal healthcare will bankrupt the system unjustified;
- Costs will increase but competent transparent budgeting can ensure achieving public health objectives.
Human and budget resources are key for the function of any organization, and in the HHS these are aspects that are highly systematic and regulated tediously. Human operations are a complex system which guides various aspects of functionalities and program development at HHS. Therefore, in the creation of a universal system of care, the HHS has the available professionals to develop its components but will need to expand. Meanwhile, the budgeting will have to be approved by Congress based on detailed justifications for each expenditure or program.
Politics and Policy Impact
- Governance of political institutions impacts redistributive policy;
- The U.S. bicameral and partisan political system has numerous veto points to essentially block healthcare policy;
- Zero sum approach held by many on universal healthcare;
- Policy must be not only passed but funded in future years;
- Political ideology has significant opinions on universal healthcare influencing a stagnation of policy in U.S. federal and state representations;
- There is increased political disagreement on how to proceed forward with healthcare in the U.S.;
- Despite universal agreement that change is needed, the policy comes down to partisan and special interest influence;
- This approach creates barriers to management and implementation of good public policy;
- The HHS is reliant on funding from Congress, and not only budgetary constraints are concerning, but political slashing of funding for programs;
- Policy and legislation being political results in leadership having navigate the complex politics when leading the agency and developing new initiatives.
Healthcare is defined by politics, particularly the concept of universal healthcare and the redistributive type of policy it entails. Any legislative and policy system has chokeholds, known as veto points, where a policy may become stagnated or fail, such as court rulings, referendums, or multiple chambers of legislature. In the U.S. the administrative political system has one of the highest numbers of veto points, which combined with ideology makes healthcare policy exceptionally slow to develop and pass. Furthermore, the politics promotes inegalitarianism on the privatized health system making it easy to stop implementation of universal care.
As was evident with Obamacare, major overhauls to national health policy are problematic. A decade after passage it still faces appeal, legal challenges, and funding cuts. Similar aspects would apply to universal healthcare, at an even greater intensity. The policy aspect of healthcare is so dependent on politics that neither legislature nor the HHS agency itself can proceed forward without constant barriers.
Ethical Concerns
- First concern is fiscal responsibility when working with public resources and funding.
- Management of funds must be transparent and avoid supporting private gain as commonly occurs with numerous private contractors and insurers in healthcare.
- Competent management of funds to achieve access and coverage amid budge constraints (Tran, Zimmerman, & Fielding, 2017).
- Second concern is equitable distribution of resources.
- Healthcare is inherently disparate in terms of access.
- Socioeconomic and racial factors play a role in availability of public health.
- Equitable access and funding must be provided to all populations in need (DeSalvo et al., 2017).
Universal healthcare as a public service require competent management by public administration which provides the public good at a high ethical standard. Ethical concerns include fiscal responsibility and equitable distribution of resources when it comes to public healthcare. This includes ensuring transparency in spending and not inappropriately funding private entities present in the sector. Furthermore, the disparities should be eliminated to the best of the possibilities by public administration by providing equitable funding and quality of care to lower-class socioeconomic neighborhoods.
Constitutional Law
- Constitution does not explicitly guarantee right to healthcare;
- Provides Congress the ability to establish statutory rights for individuals;
- Using this, Medicare and Medicaid have been created;
- Congress has power to enact laws for public welfare as well as fund them;
- Legislative powers used to regulate economic aspects of healthcare (Sunkara & Rosenbaum, 2016).
According to the Constitution healthcare is a not a guaranteed right. Instead the document provides legal tools for Congress to enact statures and laws which can create statures and legislation that regulate healthcare. This includes major policies and statures such as Medicare and Medicaid. Furthermore, Congress has the power to levy taxes, regulate commerce, create economic mandates, and fund mandates which are parts of the national healthcare system. This allows broad possibilities to expand access to healthcare to greater populations given proper policies and funding are in place.
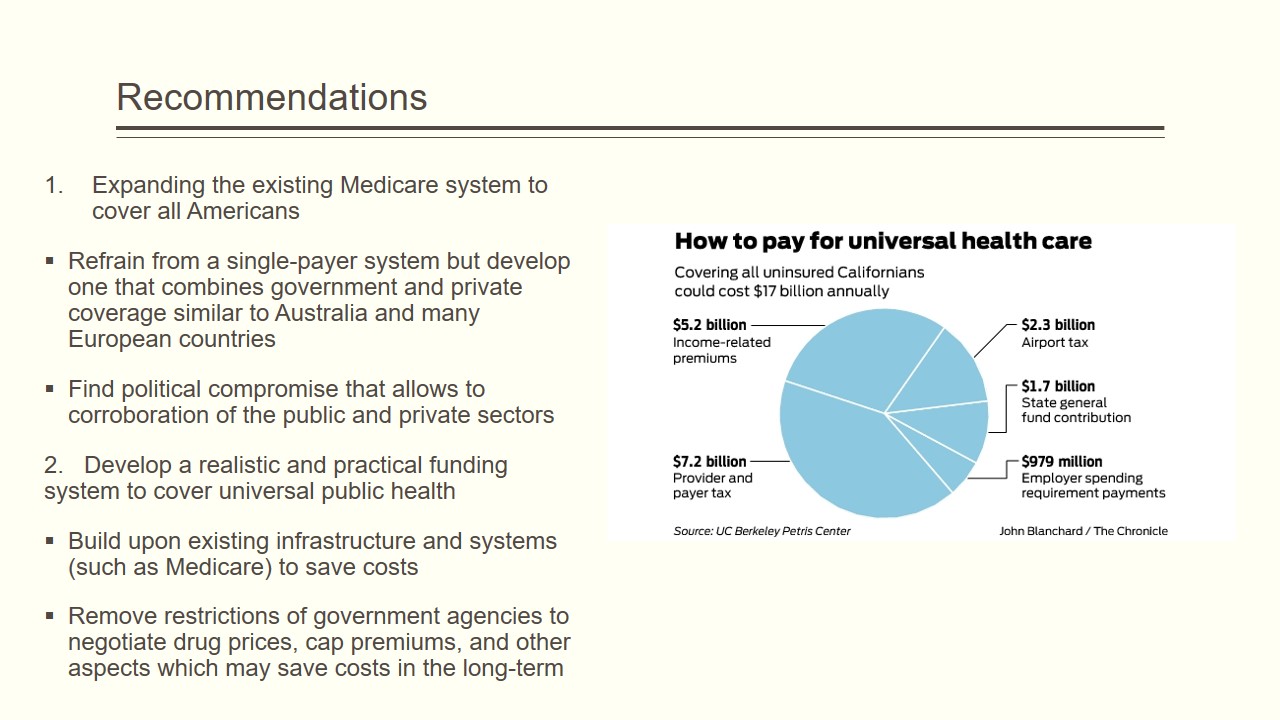
Recommendations
- Expanding the existing Medicare system to cover all Americans:
- Refrain from a single-payer system but develop one that combines government and private coverage similar to Australia and many European countries;
- Find political compromise that allows to corroboration of the public and private sectors.
- Develop a realistic and practical funding system to cover universal public health:
- Build upon existing infrastructure and systems (such as Medicare) to save costs;
- Remove restrictions of government agencies to negotiate drug prices, cap premiums, and other aspects which may save costs in the long-term.
The only way forward to adopting some level of universal healthcare is to find compromises, primarily politically. This can be done by avoiding ideological slogans of medical “communism” but focus on developing a proposal of a healthy collaboration with the private sector since the majority of Americans support this approach rather than single payer system. In order to deal with funding issues, it is proposed to use existing systems, and provide greater bargaining power for the government in reducing its bulk purchases and investments into the healthcare system.
References
Denhardt, R. B., Denhardt, J. V., & Blanc, T. A. (2014). Public administration: An action orientation (7th ed.). Belmont, CA: Thompson – Wadsworth – Cengage Learning.
DeSalvo, K. B., Wang, Y. C., Harris, A., Auerbach, J., Koo, D., & O’Carroll, P. (2017). Public health 3.0: A call to action for public health to meet the challenges of the 21st century. Preventing chronic disease, 14, E78. Web.
Greer, S. L., & Méndez, C. A. (2015). Universal health coverage: A political struggle and governance challenge. American Journal of Public Health, 105 (Suppl 5), S637–S639. Web.
Sunkara, V., & Rosenbaum, S. (2016). The Constitution and the public’s health: The consequences of the US Supreme Court’s Medicaid decision in NFIB v Sebelius. Public Health Reports, 131(6), 844–846. Web.
Tran, L. D., Zimmerman, F. J., & Fielding, J. E. (2017). Public health and the economy could be served by reallocating medical expenditures to social programs. SSM – Population Health, 3, 185-191. Web.