Introduction
What could happen when someone calls 911, and there is no response, or the ambulances arrive too late? The healthcare system in the United States has been subject to many critical issues, one of which involved the shortage of personnel. Much of the current focus in research and policy-making is on such aspects as nursing and access to drugs, which means that other areas of shortages go unnoticed.
The paramedics and Emergency Medical Technicians (EMTs) are facing the same situation where acute declines in their numbers are affecting the efficiency and effectiveness of the entire system. The problem has not been approached the same way that nursing or other healthcare personnel shortages are, especially in healthcare research. Therefore, it means that the only way that the problem has been made public is through the news media. A growing number of publications and online news channels have raised their concerns regarding the issue. After a closer examination, it emerges that the concerns are justifiable and that the state should attempt to develop appropriate remedies.
As a cofounder of Acute Medical Services, where I currently serve as the President and Executive Chairman, I would like to express that the issues outlined in this paper are professional and personal observations made throughout the 27 years of emergency medical services (EMS). Most importantly, the paper will outline the need for developing the capabilities of and creating an enabling environment for private practitioners to ease the shortage. Such recommendations are not from an entrepreneurial perspective but from a practitioner’s point of view where the overall wellbeing of the Americans is prioritized. Both public and private sectors are currently unable to meet the demand.
Therefore, this paper is an expression of the need for the Senate to address the problem and facilitate both sectors to operate effectively in serving Americans. A few recommendations will be discussed after the nature and extent of the EMS shortage have been discussed in detail.
Why the Shortage?
The EMS profession is hardly recognized as part of the broader healthcare system in the United States. However, it does not mean that the challenges regarding the personnel shortage are dissimilar in the two contexts. As mentioned earlier, the shortage of EMS and EMT personnel is a concern being addressed in the media without much scholarly interest. However, an experienced expert in the EMS field can also make informed and expert observations, which is a key aspect of the voices raised in the media. Several reports and examinations explain several causes of the shortage, which include inadequate personnel, shifting to better-paying jobs, over-dependence on volunteer work, reduction in the number of graduates, and unprecedented violence associated with the profession. To better understand these causes, it is important to explore them further, as explained by several experts.
The most obvious cause of personnel shortage would be that there are fewer workers as compared to the demand for their services. The EMS in the United States can be perceived as employing inadequate numbers of workers in this field. There may be justifiable reasons for this observation, but the key point is that a profession with few qualified workers in the labor market would experience shortage problems. According to Buckley (2020), the number of first responders has dropped by 9% in the last decade across the United States, as highlighted in a survey conducted by the New York State Health Department. Such statistics indicate that fewer people are entering this workplace to replace those that are leaving.
The major problem and cause of the EMS shortage is the lack of finances, both in the private and public sectors. Such sentiment has been voiced in an article in the FR Conversations, where it is expressed that the EMTs need a viable wage to operate (Nationwide EMT shortage plagues emergency providers, n.d.). Even when volunteer work is used, training activities take both time and money, and the volunteers are required in most cases to pay for the training with their money.
For the professionals, the EMS does not provide a promising career path because of the low wages. Many people with training will tend to find a paying job as an EMT, after which they need for better careers causes them to leave the profession entirely. According to Edwards (2019), North Dakota emergency responders are required to attend between 50 and 60 hours of training, costing approximately $600 and have to be paid by unpaid volunteers. Therefore, it becomes apparent that even voluntary work faces hindrances and cannot be depended upon as a short-term solution to the shortage.
The wages for the EMS workers have also been criticized by many people as being inadequate. Many professions use compensation to attract employees, which should work for the EMTs. Such a concern is raised by Spencer (2020), who states that the Marathon Area Volunteer Ambulance Corps is among those losing their personnel to firms that can pay better wages. Losing personnel to other EMS providers should not be a major problem to the system because the workers stay in the industry. However, losing workers to other professions is the main challenge because it leaves deficiencies within the EMS.
For instance, Edelman and Garger (2019) explain that approximately 60% of the available EMS workers have less than years’ experience because those with more years have left the EMS to join the firefighters. Besides being short-staffed, the EMS faces a more significant challenge when the best employees opt for other professions leaving only inexperienced ones behind. Therefore, it can be argued that the EMS is unattractive for many people who would prefer better alternatives. In the case of New York, Figure 1 below should help illustrate the effects of losing EMS workers to other jobs.
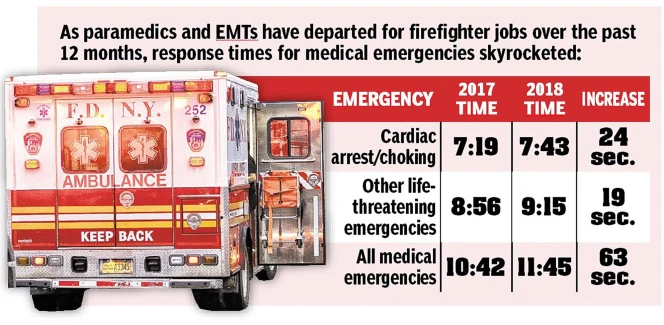
Nuisance and violence have also been highlighted as significant reasons for the shortage. Edelman and Garger (2019) reveal that EMTs are always complaining about nuisance calls, which makes their work difficult stressful. The current shortage means that the available personnel cannot be overstretched, and the number of calls coming in daily is too much for them to handle. The stressful work environment is unsustainable, which makes it easier for the EMTs to contemplate leaving for a better career. The issue of unprecedented violence has been raised by Byers (2020), who expresses that St. Louis is the most dangerous city in the United States where an EMT is not expected to last two years. However, it can be argued that violence is specific to certain regions across the country, but the dangers of the job are enough to scare away potential employees.
Lastly, it is important to acknowledge another major reason for the shortage: the falling number of EMT graduates. According to Snuder (2019), the number of graduates from paramedic training has declined from 1200 to 250 annually over the last three years. Even with enhanced recruitment efforts, it can be argued that the solution cannot be found without making the profession attractive for new graduates. The decline in graduate numbers can be associated with several problems faced by the sector, including inadequate compensation and a highly stressful work environment. The challenge for the senate will be to develop appropriate legislation and policies that raise the graduate levels and to create a supply line for the EMS.
Average Payment for Medicare to Private Ambulance Providers
The subject of Medicare in the United States is another issue that can be improved concerning EMS services. Currently, inadequate data is showing the average payments that have been made to private ambulance service providers. The regulations of Medicare indicate that Medicate tends to cover only those ambulance services nearest to the appropriate hospital that can offer the type of care needed (Ambulance transportation basics, n.d.). The ambulance companies are not assured that Medicare will pay for the services offered, in which case the first responders may be hesitant to offer the services. In cases where Medicare fails to pay, it can be assumed that the charges are incurred by the patients themselves.
Without the statistics on the averages paid to private ambulances, it can be assumed that the private ambulances operate under the same terms as the public ones. Therefore, Medicare can cover up to 80% of the approved costs, which means that the recipients pay the remaining 20% needed (Ambulance transportation basics, n.d.). Another presumption is that the private ambulances only respond to those calls that have been approved by doctors to qualify for Medicare payments.
In any other cases, it can be assumed that the patients pay for all the costs. Regardless of whether the patients qualify for Medicare for their ambulance services, concerns have been raised that hiring an ambulance is very expensive. An observation made by reveals that about 71% of the providers do not accept the insurance of the patients. Additionally, 79% of the patients taking a ground ambulance could still pay up to $450 after the insurance has been paid. Even with payments made to private ambulances by Medicare, it can be seen that patients can fail to get adequate support from the EMTs.
The key problem with Medicare is that it cannot be relied upon by private providers, which eliminates a key source of funds. As explained earlier, the major challenge with the profession is the lack of funds to finance the basic activities. Medicare could provide a means by which even the private providers can gain revenues, which can then be used to pay better wages. The Senate should reconsider the use of Medicare for ambulance services to make it easier for the private sector to operate seamlessly.
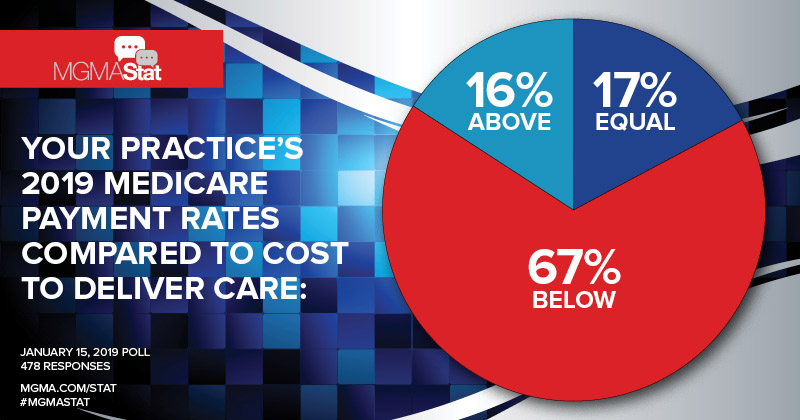
The shortfalls of Medicare include that they cannot effectively pay for all the ambulance services. As illustrated in the figure below, 67% of the Medicare reimbursements have been below the actual costs incurred by the proverbs (Voytal & Gelburd, 2019). The Senate should find a better framework with which Medicare should work to cover ambulance and other EMS costs fully.
Importance of Private Ambulance Providers to the Healthcare System
While recognizing that the shortage of EMS workers is a real problem, it becomes more apparent that the private sector has a key role to play. The question of how private ambulance providers are important for the healthcare system can be answered by exploring ways in which the providers supplement the public sector and how they can help ease the shortage of EMS workers. Calams (2021) explains that private ambulance providers comprise 18% of the ambulance service system in the country.
Therefore, it can be argued that private companies have proven themselves to be able to play a major role in providing care for Americans and that their growth supplements the public providers. As opposed to the public providers, the taxpayers do not fund private ambulances, which means that the patients pay the fees once they use their services. In a situation where the shortage of EMS personnel affects care delivery, private providers become a key part of the country’s ambulance system.
Another key aspect of private ambulance providers is the type of services offered. According to Calams (2021), public providers are usually the ones who respond to 911 calls. On the other hand, the private ambulance performs such activities as discharge, interfacility, and other schedules and non-emergency transports. The breakdown of tasks performed by both public and private sectors indicate that the two can work together to achieve the ultimate service quality for the Americans in terms of emergencies.
However, it is important to acknowledge that some municipalities across the United States also contract private ambulance providers to handle first responses and the 911 calls. In such cases, the authorities recognize the need to have the support of private providers, especially when there is an inadequate public infrastructure to handle emergencies effectively. The fact that the municipalities can place their trust in the private sector means that the services offered are indispensable and that they meet the necessary standards to form part of the country’s healthcare system.
The importance of the private ambulance providers to the US healthcare system becomes clearer during the time of shortage, whereby the private sector fills the gaps left by the public providers. The question of whether the shortage is a crisis or an opportunity is addressed by Bledsoe (2019), who expressed that now is the time to drive the EMS forward. The crisis is felt by the public sector when there is inadequate personnel for the first responder jobs. The available staff is thinly distributed and, in many cases, inadequate. The shortage can be interpreted as an opportunity for the private sector because their services can be used to fill the gaps left.
Regardless of the tasks that the private ambulances can handle, it should be acknowledged that they ease the burden on the public providers and offers Americans better chances of quality care. With effective pricing of services, private ambulances can work effectively alongside public providers, which makes them a vital component of the American healthcare system.
Differences in Funding between Municipality 911 Ambulance and Private Health Care Providers
The main difference in funding between the 911 ambulance and the private healthcare providers is the source of revenues. The public providers are paid by the taxpayers’ money, regardless of whether or not they will use the services (Calams, 2021). The mean hourly wage of the EMTs is $17.02, while the annual wage is averaged at $36,110 (Calams, 2021). However, the costs of public ambulances differ across agencies, municipalities, and the type of care given to patients. An example of the D.C Fire and EMS given by Calams (2021) states that the BLS transport costs an estimated $428. Other charges include ALS, ALS-2, and per load mile with averaged costs of $508, $735, and $6.55, respectively (Calams, 2021). Therefore, the funding for the public 911 calls comes from the government.
On the other hand, the funds for the private ambulance service providers come from the users of the services. The patients will be responsible for compensating the private EMS agencies for all services delivered, either through cash payments or through insurance for those providers that accept them. Calams (2021) reveals that private EMS may pay less than public agencies, but they will be more willing to hire less experienced EMTs.
Additionally, the costs of private EMS depending on the type of service offered. Currently, there are inadequate figures to show estimates for private providers. However, the main difference is that the private providers get paid directly from the clients while the 911 responders are funded by the government. Most importantly, it is critical to acknowledge that private providers can also get funding from the municipalities when they are contracted to offer EMS services. Additionally, private providers can be recruited by individual healthcare facilities, in which case they can get funding from such institutions.
Texas State Medicaid Pre-Authorization for Ambulance transport
In the State of Texas, Medicaid provides free transportation for patients and other eligible Medicaid clients. The pre-condition for these services is that the clients have no alternative means of transportation. However, the issue with ambulances is less straightforward because of the problem of pre-authorization. Medicaid requires that prior authorization be given before undertaking the transport services. However, it is essential to understand that the pre-authorization is not an affirmation that the insurer will pay for the services.
In Texas, there used to be a large prominent health system where pre-authorizations were effectively conducted. The situation has changed as a result of the changes in payers. The State now faces a situation of constant denials for pre-authorization, which has ultimately reduced the efficiency of the process. Therefore, it can be argued that the presence of many payers and the tendency to hold down the costs of the healthcare system are key contributors to the challenges faced by Texans. Additionally, it has been expressed that that pre-authorization is not a confirmation that Medicaid services will pay for the costs. Therefore, the ambulance services face a situation of uncertainty, meaning they cannot offer their services effectively.
Besides the issue of multiple payers, it is also important to acknowledge other causes of difficulties. Registration errors are other examples where patients previously authorized through commercial insurance change to Medicaid after a change in their financial status. In such a situation, there was no authorization from Medicaid, which makes it hard for claims to be accepted. There are also several requirements needed for Medicaid’s pre-authorization, which could also be a key hindrance. Therefore, the main reason that it is increasingly difficult to obtain a pre-authorization in the State of Texas is that the pre-conditions and requirements are difficult to meet.
What happens in the Absence of Private Ambulance Providers?
The importance of private ambulance providers has been outlined earlier. Therefore, it is time to examine a scenario where private providers did not exist. First, it can be argued that that the current shortage would be worse than it is now, and the country would be facing a crisis. The gaps left by the public providers would not be filled, and the entire healthcare system would be in much greater chaos. Second, the new EMT graduate would not have a means of building their resume for the public sector. As mentioned earlier, private ambulances are more inclined to hire less-skilled EMTs. Such an act cannot be criticized as a possibility of offering lower-quality services. Rather, the private providers should be applauded for offering new graduates an opportunity to build their careers and prepare them for the better-paying public sector.
Lastly, the absence of private providers can create further gaps in care delivery due to over-stretched public resources. The services offered by private providers would need to be handled by the public sector, which already has a limited capacity. It is important to acknowledge that some municipalities have been forced to recruit the services of private providers because of a shortage. Therefore, the absence of private providers would mean that there would be no opportunities for outsourcing.
Cost Hindrances for Private Ambulance Providers
The cost hindrances for the private ambulances are difficult to explain because there is no standard cost structure for all agencies. However, the most important aspect of these providers is that they depend on the payments from the client to operate. In many cases, private ambulances do not handle emergency responses unless they have been contracted by municipalities to handle the 911 calls. In this case, private ambulances are only hired when the clients can afford to do so or when there are no public ambulances available. Therefore, private ambulances face a difficult time in mapping their operational costs.
The cost hindrances are often in terms of the costs of operation that have an implication on their ability to deliver quality services or even stay afloat. The private ambulances have to pay all the EMTs, unlike the public sector, where the services of volunteers can help reduce the costs. As a commercial entity, the providers of private ambulances have to balance costs and revenues. Therefore, the fact that they can have higher average costs of operation means that they can hardly compete with the public providers. Many patients would prefer public providers because of the possibilities of better services and lower costs.
Correcting the EMS Worker Deficit
The problem of the EMS worker deficit is extremely difficult to solve, majorly because it is poorly understood. According to Petke (2019), there is no single answer to the problem, which means that the first step should be a further examination of the root causes. First, the shortage has been a result of the demand for the services growing without a corresponding growth in the EMS workforce. Second, the fact that the number of EMTs joining the industry is declining means that the country faces a two-pronged problem characterized by growing demand and a declining supply.
Therefore, the first and immediate response should be to increase the supply of the EMTs to match the demand. However, such a proposition is not as simple as it sounds because it has major implications for the entire industry. Understanding why people do not want to become EMTs and why the current personnel is moving away to better careers should be the new starting point in addressing the shortage.
Several proposals have been developed to correct the EMS shortage. However, many people have expressed that the major problem is inadequate funds. The first solution for the senate to consider is increasing funding for the EMS across the country. Petke (2019) expresses that the Clark County Fiscal Court, which is a partial funder of the ambulance services in the city, approved a budget amendment to increase the budget by an estimated $470000. The increase in budget is intended to cover both benefits and wages for the EMS workers. Therefore, it is apparent that increasing funds for public providers with the hope of offering better wages and benefits will help reduce the shortage by attracting new workers and retaining the current ones. If the main cause for the shortage is the lack of money, then availing more finances should be the ultimate solution to the problem.
The EMS workforce is distributed across several departments within a municipality. Petke (2019) suggests that merging documents can create a temporary solution where joint management of the EMS makes it possible to address all emergencies centrally. The rationale can be justifiable considering that one of the main reasons for the shortage is personnel leaving for better-paying jobs, including the fire services. Merging the departments can stop this mobility, but it may require that a standard rate of wages and benefits be developed to keep the workers in the sector. Failure to do so may result in the EMTs leaving for other jobs in the broader healthcare sector, leaving the EMS with an inadequate workforce.
Another solution offered from a scholarly perspective is using students to fill the gaps. A study by Uppal and Gondi (2019) proposes that a mutually beneficial partnership between the local EMSs and medical students can be developed in the shortage areas to mitigate the risks associated with inadequate EMS staffing. The partnership is deemed to be mutually useful for both parties because, on the one hand, the EMS can gain workers who do not necessarily require hefty remuneration.
On the other hand, the students are presented with a learning opportunity where on-field experience boosts their competence levels. The medical students will hope to serve in better positions within the larger healthcare system in the country. However, they also require opportunities to build their experience and competence. Therefore, allowing them to work under the supervision of veterans and helping to accomplish some of the critical care tasks can be a real short-term solution to the crisis.
Most importantly, the EMS should embrace the presence of private providers to help bridge the gap. Many of the options explored so far do not offer long-term and sustainable solutions. The private providers are business-oriented operators, which means that they can have more efficient operational models. Integrating their services with those of the public providers through public-private partnerships can offer a long-term solution to the shortage. Creating an enabling environment for the private operators, which includes public funding of private ambulances, can help boost the workforce in the industry. The rationale is that the public facilities are limited, and the municipalities can take advantage of the opportunities and competencies provided by the private providers.
The current environment does not allow private ambulance agencies to achieve their full potential. In many cases, the private sector has proven to be more efficient in certain areas, and, therefore, the same can be expected in the EMS. The competition resulting from multiple companies entering the market will only serve the patients better with improved services and better response rates. In a nutshell, the private sector offers the ultimate solution for correcting the EMS worker shortage.
Increasing Funding to EMS Providers
One of the ways proposed above for correcting the deficit is providing more funds to cater for the wages and benefits of the EMTs. Therefore, this is an appeal to the Senate to consider means of increasing funding to EMS, even if the approach will target only public providers. The rationale is that the public providers can only operate within the allocated budgets, meaning that when funds are inadequate them, the EMSs cannot hire adequate personnel.
Budgeting is seen as the ultimate tool to help solve the problem, majorly because the public EMSs are funded directly by the taxpayers’ money. In the private sector, the situation is different because the funding depends on the affordability of the services and the willingness of the municipalities to recruit the services of the private ambulances. The role of the private sector can also be enhanced by providing more resources to the EMS. The argument is that there are cases where demand fluctuations make it impossible for public entities to sustain high levels of staffing. The gaps left when demand surges can be filled with the use of private providers.
Most importantly, increasing funding tends to solve almost all problems within the EMS. Consider, for example, that the volunteers are unable to pay for their training, which prevents them from offering their services. More funds for the EMS means that the volunteers can be offered free training through government-funded training programs. Additionally, the training also offers more people an opportunity to enter the workforce without worrying that they will personally incur the costs of the training. Therefore, funding the EMS will be the ultimate effort with the most positive outcomes for the EMS worker shortage.
Another way to release more funds for the EMS is by ceasing standard payment rates for the ambulances. Such an approach is followed by initiating a lower reimbursement rate for repetitive ambulance transport requiring more than ten rounds. With these efforts, the funding for the low ambulance rates for trauma and medical ambulance rates can be increased. However, it should be noted that depriving funds for certain ambulance services may not be the ultimate solution. Therefore, the Senate is requested to find means of availing more funds without disrupting certain aspects, especially those that are critical.
One Certified and Licensed EMT per Ambulance
Currently, many states have resorted to having only one licensed or certified provider on an ambulance with a driver during the pandemic. Such an approach can be effective because it allows for the available personnel to be re-distributed to more ambulances to increase the rates of response.
Therefore, it can be recommended that this standard be upheld until the workforce become stable again. The key point is that the current move was institute due to the coronavirus pandemic where the shortage could have severely damaged the response rates of the EMSs. Since the approach has proven to be feasible, it is justified to emphasize that the same arrangement can be used post-Covid-19 as a short-term resolution. However, the efficiency of such an arrangement will need to be established before it can be sustained for longer periods. Without empirical evidence to show that having only one EMT and a driver on an ambulance affects the quality, the authorities can use it to address the shortage.
Competitive Bidding Process for Ambulance Companies
From an economic perspective, competition drives quality and benefits for the consumers. Setting up a competitive bidding process for the ambulance companies can be expected to work in the way. In other words, competitive bidding allows the provider with the best cost structures accompanied by the best quality services to win the ambulance contracts. Some regions across the USA have started using this approach. For example, the town of Weymouth initiated the process in 2017, which would see a competitive bidding process take place for the first time in the past decade (Trufant, 2017(a)). Such an approach offers the municipalities a competitive edge in obtaining services and outsourcing at lower costs. The problem of finances can be solved if the competitive bidding results in lower contracting costs to the private sector.
After the announcement of the plan to contract ambulances in Weymouth, several proposals soon followed, which indicates that competitive bidding can be the ultimate solution. According to Trufant (2017(b)), three companies sent their proposals, which were to be evaluated within 30 days. Therefore, it is possible to argue that competitive bidding allows the authorities to attract the services of private companies in cases where the public infrastructure and facilities are inadequate. The responses from the companies were also evidence that private companies can build capabilities to handle the responses.
For example, one of the ambulance companies, Brester Ambulance, undertook to build a public safety system to work with both the police and firefighters. Additionally, the firm opened headquarters in the city to make it easier for it to operate effectively. All these can be used as signs that competitive bidding helps the cities obtain better ambulance services from private providers.
Cap and Place Limitations on Damages
Another approach to be considered is the number of damages that can receive in case of a lawsuit. The recommendation offered is that capping and placing limitations on the number of damages can work to benefit the ambulance providers in terms of lowering the financial burden upon them. The problem of finances is majorly responsible for the efficiencies and capacities that can be achieved by providers, both public and private. Additionally, the probabilities of damages paid by the providers will imply that the companies face extra costs, which can be eliminated to allow them to spend on better efforts. For example, reducing the number of damages can raise funds for more personnel or training facilities.
However, it is important to understand that the essence of the laws in EMS is to prevent malpractice and protect the patients. Many of the lawsuits require the patient to prove that the providers acted negligently. The damages are an effort to instill a duty of care among the EMTs. With the current shortage and financial constraints, it would make it impossible for the ambulance providers to hire more staff or to offer better wages and benefits to the current workforce. Therefore, it can be argued that hefty damages affect the entire EMS profession negatively.
Affordable Healthcare for Front Line Workers
Affordable healthcare for frontline workers is a sensitive subject, especially when it comes to the response times of the ambulances. It can be expected that offering frontline workers affordable care will make it possible for them to afford the services of the ambulances. However, some scholarly research may prove that such an effort may negate the response times of the ambulances. According to Courtemanche et al. (2019), the introduction of the Affordable Care Act meant that both private and Medicaid coverage was expanded. The empirical results of their study reveal that the ambulance times were reduced by approximately 24%.
However, the current issue under consideration is the shortage of EMS workers as a result of reduced affordability of the ambulance services, which make the companies adjust by reducing wages and employing fewer people. Increased coverage to include ambulance services for all emergencies and necessitated ambulance transportation may avail funds for the ambulances even in cases where the patients cannot afford it. Therefore, there is a need to explore further how affordable healthcare can help address the current shortage of EMS workers.
Conclusion
The shortage of EMS workers is growing to become a national crisis in the United States. The root causes can be easily understood as expressed in this paper and can be used to help the senate develop the necessary policies to avert the dangers. Most importantly, the problem results from inadequate funds for the EMS. The challenge becomes more complex when the bad finances limit the ability of the providers to hire more staff. Most importantly, the EMTs are leaving for better-paying jobs, which means that the EMS is left with few experienced workers. The private sector also faces the same challenge because private providers are also unable to pay good salaries.
Therefore, the thoughts expressed in this paper reveal that the ideal way to deal with the situation is to make the profession attractive. The declining number of graduates is evidence that the EMS does not offer a good career. Increasing funding allows the providers to offer better wages and benefits, which attracts new personnel and helps retain the current ones. Other aspects have also been considered, including such initiatives as allowing one EMT and a driver for each ambulance.
Competitive bidding processes have already shown to be effective in engaging affordable private providers to bridge the gaps. Therefore, it has been argued that creating an enabling environment for private providers to thrive will help resolve the issue. Many of these issues and recommendations require a policy framework with a national outlook. The senate is the best place to start in the search for solutions for the EMS worker shortage.
References
Ambulance transportation basics. (n.d.). Web.
Bledsoe, B. (2019). The paramedic shortage – opportunity or crisis? Journal of Emergency Medical Services. Web.
Buckley, E. (2020). Growing shortages of EMT’s & paramedics: Statewide nine percent drop in last decade. WKBW. Web.
Byers, C. (2020). Unprecedented violence, pay issues, pandemic causing paramedic shortage in St. Louis. KHOU. Web.
Calams, S. (2021). Private vs. public ambulance services: What’s the difference? EMS1. Web.
Courtemanche, C., Friedson, A., Koller, A., & Rees, D. (2019). The affordable care act and ambulance response times. Journal of Health Economics, 67. Web.
Edelman, S., & Garger, K. (2019). NYC’s emergency worker shortage has become a crisis. New York Post. Web.
Edwards, E. (2019). What if you call 911 and no one comes? Inside the collapse of America’s emergency medical services. NBC News. Web.
Nationwide EMT shortage plagues emergency providers. (n.d.). Web.
Petke, F. (2019). Closer Look: No single answer to EMS staffing, shortages. The Winchester Sun. Web.
Snuder, K. (2019). Ambulance services face national paramedic shortage. EMS1. Web.
Spencer, C. (2020). EMT shortages affect greater Cortland area, America as a whole. Cortland Standard. Web.
Trufant, J. (2017(a)). Weymouth to soon open up bids for ambulance services. The Patriot Ledger. Web.
Trufant, J. (2017(b)). Three companies vying to provide Weymouth’s ambulance services. The Patriot Ledger. Web.