Outline
- Introduction
- Examples of Errors in Pharmacy
- Process-Map Analysis
- Verbal Explanation
- Graphic Input
- SIPOC Model Analysis
- Verbal Explanation
- Graphic Input
- Main Problems in the Business Identified
- Main Root Causes
- Common Causes
- Tools and Data to Collect
- Proposed Solution and Measure
- Conclusion
Introduction
The issue of the inaccurate prescription filling in the pharmaceutical industry poses threats to the individual’s well-being and business’s success. Though medication errors in the dispensation process do not occur frequently, even rare inaccuracies result in customers filing a lawsuit against the company. To propose an effective solution to the issue, the critical problems in the HMO’s pharmacy followed by a process map of the prescription filling process and SIPOC model analysis need to be identified.
Examples of Errors in Pharmacy
Despite a relatively reliable recording system in the pharmacies, medication discrepancies happen due to a variety of reasons. As specified by Bishop, Cohen, Billings, and Thomas (2015), several examples of problems in the industry include faulty prescribing, prescription, and transcription. More frequently, pharmacies face difficulties in administrating and dispensing medicine (Bishop et al., 2015). Aldwaihi, Schifano, Pezzolesi, and Umaru (2016) support the findings of the earlier research, suggesting that dispensing errors result in the distribution of the drug of inferior quality, strength, and dose. For preventing such instances, it is essential to develop a process-map outlining the critical problems in HMO pharmacies.
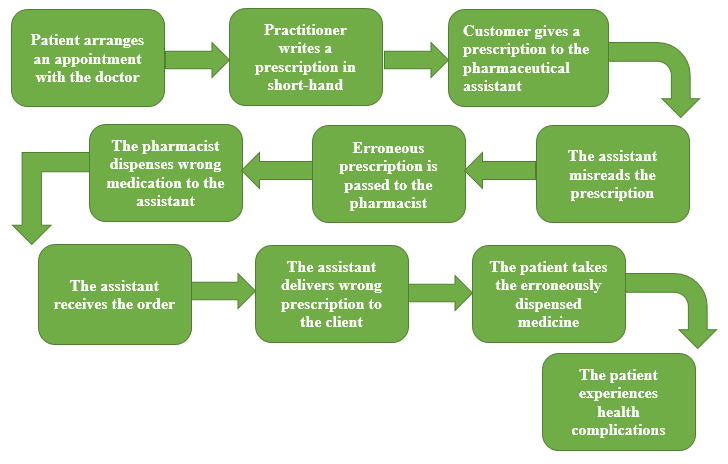
Process-Map Analysis
As shown in figure 1, errors in filling a prescription at the HMO pharmacy may occur during several stages. This process-map focuses specifically on the issues connected with dispensing medicine, such as incorrect labeling or distribution of the wrong dose. Key problems identified in the industry are loss of the assistant’s attention when reading the prescription, and pharmacist’s failure to identify and correct mistake in the clerk’s labeling (Bishop et al., 2015). The scope of the detected issues and their effect on the HMO pharmacy’s business process should be further analyzed, using the SIPOC model.
SIPOC Model Analysis
According to the SIPOC model, the business process in a pharmacy is divided into five categories: supplier, input, process, output, and customer. As briefly summarized in figure 2, suppliers in the industry are pharmacy staff, doctors, and patients. Customers include individual patients, families, and healthcare professionals. Input constitutes of the patient’s record, medication prescriptions, and printer drug directory, while output contains medicine, daily dose recommendation, and prescription labels. The general process follows several specific steps in chronological order. First, the pharmacy assistant intakes and entries the prescription. Then, he passes the prescription to the pharmacist who verifies it. After the verification procedure, the pharmacist passes the order back to the assistant who dispenses the drug to the customer.
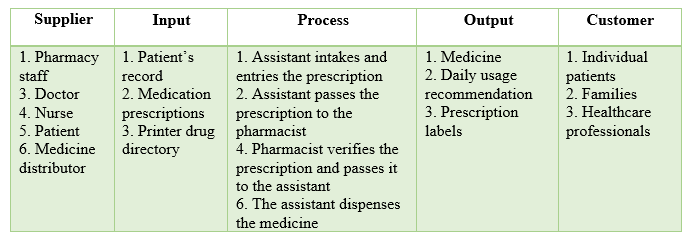
Errors in the dispensing process, described in the process-map, prevent the pharmacist from obtaining a correct prescription from the assistant. This inaccuracy infringes the correct sequence of actions, outlined in the SIPOC model, and results in the wrong medication dispensed to the customer. The root cause of the problem lays in the assistant’s inability to enter the prescription correctly (Aldwaihi et al., 2016). Since the assistant’s lack of focus on the entry-stages results in the pharmacist dispensing the wrong type of medicine, the causes of the issue are common. The adverse effects arose as a result of the intervention are predictable and controllable with a series of alternative solutions.
Main Problems in the Business Identified
To further analyze and resolve the problem, it is essential to collect additional data. Campmans et al. (2018) wrote that self-report questionnaires, where pharmacy staff anonymously identify the causes for dispensing discrepancies, may be beneficial in the situation. Common comments received in the surveys include distraction while dispensing, fatigue, as well as similar names and appearance of the drugs (Campmans et al., 2018). Reported reasons vary in different pharmacies, thus, gathering individual feedback will allow managers to implement the best solution.
Proposed Solution and Measure
While it is impossible to eliminate the human factor, the pharmacist’s dispensing process may be improved through the usage of advanced technologies. Campmans et al. (2018) suggested incorporating barcode scanners and Tall Man lettering to reduce the instances of pharmacists or/and assistants misreading the prescription letter. First, barcode scanners verify whether the chosen drug from the shelf corresponds to the selected drug on the screen after the entry. Second, Tall Man lettering alerts the staff about the possible confusion in the look-alike drug names, their dosage, and strength (Campmans et al., 2018).
The one strategy to measure the aforementioned solution can be a thorough examination of the reports from the alert system. Findings should be statistically analyzed with the dynamics of the medication discrepancies compared before and after the installment of the technology.
Conclusion
Ultimately, inaccurate medicine dispensation infringes the exact process of filling a customer’s prescription, leading to some negative consequences. Erroneously distributed drug with a wrong dose, strength, quantity, or quality may result in the customer’s severe health complications. Though it is impossible to eliminate the human factor, in terms of fatigue and loss of focus, incorporation of advanced technologies, such as barcode scanners and Tall Man lettering might reduce the number of dispensing errors.
References
Aldwaihi, K., Schifano, F., Pezzolesi, C., & Umaru, N. (2016). A systematic review of the nature of dispensing errors in hospital pharmacies. Integrated Pharmacy Research and Practice, 5, 1-10. Web.
Bishop, M. A., Cohen, B., A., Billings, L. K., & Thomas, E. V. (2015). Reducing errors through discharge medication reconciliation by pharmacy services. American Journal of Health-System Pharmacy, 72(17), 120-126. Web.
Campmans, Z., Van Rhijn, A., Dull, R. M., Santen-Reestman, J., Taxis, K., & Borgsteede, S. D. (2018). Preventing dispensing errors by alerting for drug confusions in the pharmacy information system – A survey of users. Plos One, 13(5), 1-11. Web.