Modern access to information technology can potentially develop the rational usage of human resources and abilities. Telesitter is a portable two-way video camera installed in patients’ rooms, helping the staff to monitor their conditions. The data is rapidly transferred to the hospital employees if any acute situation happens. The technological progress of IT methods can help reduce hospital costs and provide rational planning of the staff activities. The purpose of the paper is to research the scholarly literature on the critical topic and analyze the modern problems in medicine, the positive sides of using Tele sitters, and the potential benefits Tele sitters can bring. Hence, the paper’s methodology will be qualitative analysis using secondary sources.
The current work aims to develop a project helping understaffed hospitals implement and utilize Tele sitters. Project objectives are understanding the weak chains of the medical nurse system in monitoring patients, applying the innovative method to the hospitals, and making it efficient within two years of practice. Only scholarly articles and other trustworthy data providers were used during the paper creation, and all the statements taken from different sources are highlighted with citations. Developing the system of Tele sitters in more hospitals can enhance the hospitals’ income and help understaffed departments.
The number of patients that need bedsitters increases according to the season and the collaboration of their pathology. Often, a patient requires 24-hour control and support, and Tele sitters can easily cover such needs by changing shifts and saving the costs on nurses and bedside sitters. According to Roth’s analysis (2019), US San Diego Health estimated the cost savings by using Tele sitters by $2.5 million within two years. Telesitters can provide a patient with communication and companionship, so the psychological aspect of the monitoring is being saved. Several people need support and the feeling of being cared for by someone. Telesitters have good-quality equipment allowing them to communicate with patients.
The main concern in current medicine should be planning and managing nurses’ work time rationally. According to the experience gathered from nursing leadership and management, it is proved that nurses can be easily integrated into the IT system and control the major indicators using electronic data. Along with the usual informatics nurse responsibilities, a new position in the hospital is called the chief nursing informatics officer (CNIO) (Murphy, 2011). Developing the duties of nurses inside the department can help improve the clinic’s efficiency and provide better outcomes. Moreover, the intensive care units, due to the more significant number of acute pathologies, need the video monitoring systems similarly, and Tele sitters were proved efficient in these departments as well (Romig, 2019). So, the first step in implementation is proper education of the nursing staff to comprehend Tele sitters’ responsibilities and possible ways to interrelate with them and take action rapidly after receiving data from them. The duration of the first step should take three months as the practical implementation of the knowledge is planned further on and will take substantially more time. Educated nurses are the human resources needed for the project.
The main issues standing in front of the hospitals for implementing and utilizing the system are the budget for the cameras and following equipment. However, cost savings on nurse shifts, occupational burnouts of the staff, and the spending on patients’ elopements and falls in the long-term perspective are more expensive than using the method. The study by Plahar (2020) proved the statistically positive effect of patient video monitoring on the number of falls in the hospital in Northern California. According to the study by Johnson (2017), video monitoring proved to be more efficient and beneficial for hospitals and patients’ safety, and within a tool, clinics could manage more patients with less staff occupied. So, the second step of program implementation is to set the required equipment and develop a long-term plan of increasing hospital administrations gradually with a similar number of employees within six months. Physical resources for the project are equipment allowing Tele sitters to monitor patients (video cameras, microphones, computers, and offices). The technical resources needed for the project are the data software to unite human and physical resources.
In the first six months of implementation, it is essential to evaluate the cooperation of the working personnel and calculate the time used for information transferring between them. This can help highlight the weak chains of the system and develop strategies to help reduce the time losses. During the first year of method utilization, patients will be surveyed to distinguish Tele sitters’ positive and negative sides. Patients, being custom receivers, might provide managers with helpful feedback assessing how different they find it to be monitored via video tools, what Tele sitters lack compared to the bedside sitters, and how essential these aspects are for them. Moreover, some patients might feel uncomfortable being constantly monitored, even though “virtual curtains protect the data” and patients’ privacy is protected (Roth, 2019). The first six-month plan sets the equipment and assesses the cooperation between various groups of employees and patients’ feedback.
Step three of program utilization enhances the outcomes received in the first six months of work. The time loss between the data transfer and patient feedback can help highlight the major issues and develop a strategy for further improvements. Step 3 is also six months of work, allowing personnel to get used to the innovatory system and smoothen all the disadvantages. Afterward, the project is finished and is integrated into the clinic, and the formative evaluation of its outcomes are the patient’s application forms assessing the work of staff, and leaving reviews. If more than 90% of patients are satisfied with the method and its implementation, the project can be successful and completed.
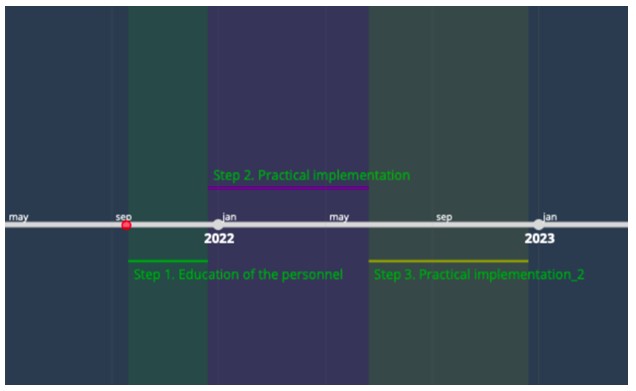
Below presents a graphic timeline of the project’s most critical stages, as shown in Figure 1. The first step is educating the staff for three months; the second is setting the proper equipment, assessing the cooperation between various groups of employees, and providing patient feedback, for which six months are needed. The third step is also practical, as a previous one, and lasts for six months. During it, the staff will correct the time losses and small details slowing the work process, and the final assessment as patient’s feedback will be done. Thus, in 1 year and three months, the Tele sitters can be implemented in the hospital and successfully utilized.
References
Johnson, J. R. (2017). Clinical Questions About the Use of Video Monitoring for Patient Safety. Journal of Neuroscience Nursing, 49(6), 341–343.
Murphy, J. (2011). The nursing informatics workforce: Who are they and what do they do? Nursing Economics, 29(3), 150–153.
Plahar, A. Q. W. (2020). Implementing Virtual Sitters to Reduce Falls and Sitter Costs. Doctor Nursing Practice, 234, 1-196.
Romig, M., Derrett, R., Latif, A., & Sapirstein, A. (2019). Telemedicine consultation to the general ICU. Telemedicine in the ICU. Springer, Cham.
Roth, M. (2019). Ochsner reduces patient falls by 51% with Tele sitters. Health Leaders Media.