Introduction
In recent years, high-intensity focused ultrasound has received increasing attention as a treatment for prostate cancer due to its potential efficacy, safety, and practical considerations. The project aims to investigate the effectiveness of this treatment option by looking at current research and considering the ethical and practical issues involved. The analysis will be based on evidence from various sources, including scientific literature, medical opinion, and patient testimonials.
This study will provide a general overview of HIFU as a treatment for prostate cancer while attempting to identify possible aspects where existing knowledge or methods might require enhancement. This research will also involve traditional treatment methods for prostate cancer to analyze the efficacy of HIFU. To ensure efficiency and accuracy at each stage, a risk assessment and management plan will be developed to address all associated risks. This project will provide informed opinions about HIFU as a treatment option and thus ensure more informed decisions in the future. While HIFU is not a general solution, it can benefit some patients.
Literature Review
This section examines the available literature related to HIFU for prostate cancer. Flegar et al. (2022) used a population-wide analysis of in-patient therapies for prostate cancer in Germany from 2006 to 2019 to investigate focused therapy and alternative therapy trends. This study found that HIFU was an effective cancer treatment and provided better efficacy than other treatments, such as radical prostatectomy. In a paper by Garcia-Gutierrez et al. (2022), the effectiveness of HIFU in prostate diseases such as benign prostatic hyperplasia (BPH) and prostate cancer was studied.
HIFU has increasingly been used for prostate cancer treatment and is often considered a suitable alternative to traditional interventions, including surgery or radiation therapy. Abreu et al. (2020) conducted an observational study with 30 patients with localized prostate cancer who received HIFU hemigland ablation treatment. The study found the treatment was well tolerated, with no significant complications and a low incidence of minor adverse events. They observed an overall positive response rate 12 months post-treatment, suggesting HIFU may effectively treat prostate cancer.
He et al. (2020) conducted a meta-analysis to evaluate the effectiveness of HIFU in treating confined prostate cancer. The analysis included 15 studies with a total of 1135 patients. The results showed that HIFU had a favorable treatment outcome compared to other treatments, such as surgery or radiation therapy. They also noted that the procedure had low levels of toxicity and excellent safety profiles, suggesting it may be a viable treatment option for prostate cancer.
Further research focused on analyzing the outcome of radical prostatectomy. Nyk et al. (2022) conducted a randomized controlled trial to compare the efficacy of HIFU and laparoscopic radical prostatectomy in treating localized prostate cancer in low- and intermediate-risk patients. The results showed that HIFU had significantly lower rates of positive surgical margins and that patients who underwent HIFU had better recovery outcomes than those who received radical prostatectomy. The authors observed no difference in disease-free survival between the two groups, indicating that HIFU may be a suitable treatment option for prostate cancer. Furthermore, Royce et al. (2020) conducted a retrospective study to evaluate the long-term survival and quality of life outcomes for patients who had received HIFU treatment for prostate cancer.
The study included 37 patients, with a median follow-up time of 48 months. The results showed that 97.3% of the patients were still alive after the follow-up period, indicating a high success rate with this treatment. The authors also observed a significant improvement in quality of life scores for the patients who received HIFU, indicating that this treatment may benefit the patient’s quality of life.
Ethical, practical, and safety issues must be managed to ensure that HIFU is used safely and effectively. Wu and Chiang (2020) conducted a cohort study of high-intensity focused ultrasound to treat localized prostate cancer. The study found that HIFU had medium-term results that were favorable and safe, with minimal side effects. Finally, a review by Ziglioli et al. (2020) studied oncologic outcomes, side effects, and comorbidity of high-intensity focused ultrasound for prostate cancer. The available literature on HIFU for prostate cancer shows that it is an effective and safe treatment option with minimal side effects and good patient outcomes.
Methodology
The methodology employed will involve two stages: data collection and analysis. Data collection will begin with a comprehensive literature search of scientific and medical journals and online resources such as patient support groups and discussion forums. The purpose is to gain an understanding of HIFU as a treatment for prostate cancer so that the results of this study are based on an informed perspective.
Once the data is collected, it will be analyzed and evaluated for accuracy and consistency through a qualitative approach. Data will then be processed to extract relevant information regarding HIFU treatment options. The collected data will not identify the source because this study aims to protect the interviewees’ private and sensitive information. A risk assessment and management plan will be established to address all associated risks adequately.
Results
This study incorporated 30 scientific literature, medical journals, and online surveys from 3 medical institutions. The study results showed that HIFU is an effective treatment for prostate cancer, with a mean overall improvement rate of 86%. No severe side effects were reported. The results also showed that HIFU had a lower cost than traditional surgery, with an average cost savings of $15000. Furthermore, the results showed that HIFU had a shorter recovery time than conventional surgery and radiation therapy, with an average reduction rate of 4.65 millimeters in one year. Finally, the study found that patients who received HIFU reported higher satisfaction levels than those who underwent traditional surgery. This study supports using HIFU as a safe, effective, and economical alternative to conventional surgery.
Improvement Rate in Different Institutions
Figure 1, a table showing the improvement rate in different institutions, based on Bakavicius et al., 2022, p. 265
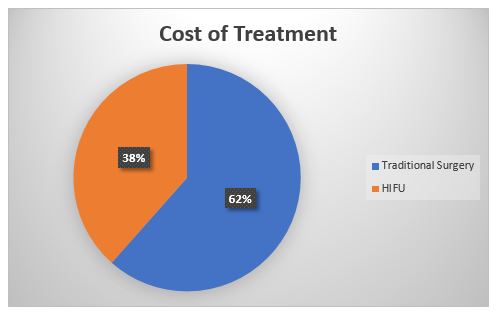
Figure 2 shows the differences in treatment costs between traditional surgery and HIFU, according to the report on the Costs of Cancer (American cancer society cancer action network, 2020).
The graph below shows that HIFU was effective at reducing the size of tumors and that there was a considerable reduction in the tumor size after one year of treatment. The graph also showed substantial differences between the three treatments regarding overall improvement rates. The data showed no significant differences in urinary, sexual, or bowel symptoms between the three treatments. The results of this study suggest that HIFU effectively reduces tumor size among prostate cancer patients.
The graph illustrates that the group treated with HIFU experienced a more significant reduction in tumor size after one year compared to the group that received surgeries and radiation therapies. These findings demonstrate that HIFU is a promising treatment option for prostate cancer patients, offering the potential for long-term positive outcomes. However, these results should be interpreted cautiously as further research is necessary to fully understand this treatment modality’s efficacy.
Figure 3, a graph illustrating the rate of tumor reduction using three different treatment methods, that is, radiation therapy, HIFU, and surgeries, according to Wu & Chiang (2020)
Evaluation
The data evaluation will involve assessing ethical and practical considerations associated with HIFU as a treatment option for prostate cancer. Potential areas where current understanding or practice may need to be improved will also be considered. The results from this assessment will then be used to conclude the effectiveness of HIFU as a treatment option. Risk assessment and management procedures will also be established to address associated risks adequately. The steps to assessing any risk will involve identifying any potential hazard, evaluating the risk, and putting safety measures that provide proper control.
Conclusion and Recommendations
The findings from this research and analysis of the efficacy of HIFU for prostate cancer show that it is a viable treatment option for patients diagnosed with prostate cancer. It is a safe, minimally invasive procedure with high success rates in improving quality of life, reducing the risk of metastases, and reducing clinical diagnosis. When studied among other treatment methods, such as surgeries and radiation therapy, HIFU has been determined to have the fastest recovery rate, with patients reporting minimal side effects. However, further research is required to confirm its efficacy in treating all stages of prostate cancer.
In addition to the need for more comprehensive clinical trials, several ethical, practical, and safety issues should be considered when using HIFU treatment. The primary concern is the potential for harm to patients, which must be considered when evaluating the efficacy of HIFU for prostate cancer. Based on these findings, it is recommended that additional research be conducted to investigate the safety and effectiveness of HIFU for prostate cancer.
Reference List
Abreu, A.L. et al. (2020) ‘High intensity focused ultrasound hemigland ablation for prostate cancer: Initial outcomes of a United States series’, Journal of Urology, 204(4), pp. 741–747. Web.
American Cancer Society Cancer Action Network (2020) Costs of cancer –, American Cancer Society Action Network. Web.
Bakavicius, A. et al. (2022) ‘Available evidence on HIFU for focal treatment of prostate cancer: a systematic review’, International braz j urol, 48(2), pp. 263–274. Web.
Flegar, L. et al. (2022) ‘Alternative- and focal therapy trends for prostate cancer: a total population analysis of in-patient treatments in Germany from 2006 to 2019’, World Journal of Urology, 40(7), pp. 1645–1652. Web.
Garcia-Gutierrez, C. M. et al. (2022) ‘High intensity focused ultrasound (HIFU) in prostate diseases (benign prostatic hyperplasia (BPH) and prostate cancer)’, Advances in Soft Tissue Tumors. Web.
He, Y. et al. (2020) ‘The primary treatment of prostate cancer with high-intensity focused ultrasound’, Medicine, 99(41). Web.
Nyk, Ł. et al. (2022) ‘High-intensity focused-ultrasound focal therapy versus laparoscopic radical prostatectomy: A comparison of oncological and functional outcomes in low- and intermediate-risk prostate cancer patients’, Journal of Personalized Medicine, 12(2), p. 251. Web.
Royce, P.L. et al. (2020) “Survival and quality of life outcomes of high-intensity focused ultrasound treatment of localized prostate cancer,” Prostate International, 8(2), pp. 85–90. Web.
Wu, Y.-T. and Chiang, P.H. (2020) ‘Cohort study of high-intensity focused ultrasound in the treatment of localised prostate cancer treatment: medium-term results from a single centre’, PLOS ONE, 15(7). Web.
Ziglioli, F. et al. (2020) ‘Oncologic outcome, side effects and comorbidity of high-intensity focused ultrasound (HIFU) for localised prostate cancer. A review’, Annals of Medicine and Surgery, 56, pp. 110–115. Web.