Introduction
Implementation of public programs should be followed by evaluation strategies to assess the effectiveness and transparency in addressing social needs. Therefore, various evaluation approaches are followed to examine whether the proposed solutions benefited the targeted population. A successful assessment involves the systematic, purposeful collection and analysis of data documenting the efficiency or shortcomings of interventions. This means that rigorous evaluative processes allow the policymakers and shareholders to determine whether a program should be maintained, altered, or eliminated based on the findings. This paper is a program evaluation strategy focusing on service connection using the available literature on the success or failure of the intervention in addressing Veterans Affairs in the Hudson Valley and across the United States.
The program evaluation process is often adaptive and examines multiple features to gauge the success or failure of an intervention. In this case, a summative strategy, which refers to the observed impact of the project on change in selected indicators, explores the results of a program or policy (Kaczmarek & Romaniuk, 2020). It provides the decision-makers with information that links activities with achievements, enabling them to infer the effectiveness of the implemented solutions. Therefore, it means that a summative assessment normally occurs at the end of a project or when the intervention has been in implementation for a while and has gained stability. The goal of the service connection evaluation is to measure the program’s effectiveness in addressing veterans’ healthcare struggles by finding out problems in the process and possible solutions.
Program Background
The cumulative exposure to violent situations can significantly affect someone’s mental wellbeing. The United States military recognizes that war has considerable impacts on its members’ physiological and psychological health, which led to the creation of a service connection program. According to Landes et al. (2021), veterans with service-connected disabilities are evaluated by the Department of Veterans Affairs (VA) to be disabled by an injury or illness that occurred or was aggravated during active military service. This intervention is only intended to benefit people exposed to conditions that left them mentally or physically impaired while in service. Therefore, an accident that occurred while in the military, even if not during deployment, is considered a condition that qualifies as service-connected disability.
The government has been providing benefits to the veterans in varying degrees since the colonial settlements of America. Panangala et al. (2014) observed that in 1718, Rhode Island created legislation that offered benefits to every soldier, officer, or sailor who served in the armed services and the family members or dependents of those who perished during the war. Such legislation has undergone many changes over the years. In 1776, Continental Congress argued that disabled veterans should receive half of their monthly payment for as long as their disabilities exist (Panangala et al., 2014). The advancement in research and medicine indicated that resulting disability from military service is not readily apparent. Therefore, from the 1920s through to 2008, Congress examined conditions that might qualify as veterans disability or illnesses caused or aggravated by being in military service, culminating in a comprehensive report that helps in the decision-making process (Barnes et al., 2007; Bodurow & Samet, 2008; Panangala et al., 2014). The conditions made it easier for deserving veterans to receive necessary compensation and help in their time of need.
The program is essential because it provides long-term care benefits to veterans. As Redd et al. (2020) described, physical and mental injuries, including post-traumatic stress disorder (PTSD), are major comorbidity for veterans. As a result, focusing on care plans that offer solutions to the illnesses that occurred or exacerbated while serving in the military reduces the burden on the veterans and their families. Spinola et al. (2021) indicated that medical or psychological evaluations are performed to determine the eligibility for service-connected disability benefits. Therefore, this evaluation process incorporates medical records detailing a veterans’ history before and after discharge, including collateral reports and neuropsychological exams. The evaluations are integral to the program because it determines the monthly stipend and other benefits such as qualifications for Veterans Healthcare Administration service, survivor benefits, and preferential hiring for federal jobs (Spinola et al., 2021). Evaluating the veterans’ eligibility is lengthy and must fulfil certain conditions.
Program Evaluation, Recommendations, and Desired Impacts
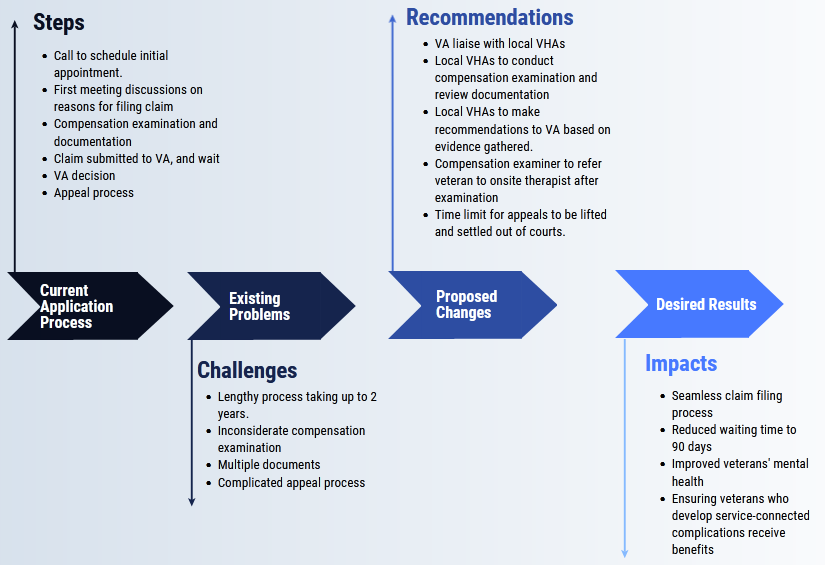
The eligibility for service connection disability compensation involves that the injury or disability be service-connected. Secondly, an individual must have been discharged under oath as any dishonorable conditions disqualify a veteran from this program. Veterans with mental health conditions, such as PTSD can apply for the benefits. The application process is as follows: first, the veteran calls Veteran Benefits Advisor, where they discuss the reason for initiating the compensation request. The veteran must book an in-person appointment where they initiate the process to file the claim and provide the necessary documentation. The Benefits Advisor submits and adjudicates the claim. The VA reviews the claim alongside supporting medical evidence and notifies the claimant in writing. The claimant can appeal the decision within a specified period (“File a claim,” 2022).
This benefits application procedure has several challenges that should be addressed. As of February 2022, the process takes the VA an average of 162.4 days to decide (“How to file,” 2022). The waiting length is problematic for many veterans in serious need of compensation and health benefits for survival. Secondly, if the decision is denied, the veteran files an appeal to the U.S. Court of Appeal within 120 days (“The VA appeal,” 2021). The court process means that the veteran undergoes the same process and must be ready to cater to legal expenses. Thirdly, Rosen (2011) indicates that veterans have to recount their painful and traumatic experiences while trying to prove they deserve compensation. The medical examinations, psychiatric interviews, examiner’s reports, and the back-and-forth means that the applicants can wait for about two years for the VA’s rating decision (“How long does,” 2021). The key challenges with the process are the length of time taken between filing a claim and the VA decision, documentation and medical tests, and the appeal procedure.
Several changes could help improve the service-connected application and award process. The first recommendation is that VA should liaise with local veteran health administration (VHA) facilities to speed up filling out claim forms. Most of the time is spent by VA reviewing the files; however, veteran’s conditions may worsen during this waiting period (Rosen, 2011). Therefore, VA should rely on recommendations or compensation ratings made by psychiatrists and medical examiners. Local offices are better suited to carry out the medical reviews to assert that a veteran deserves compensation because they meet in person than the VA officers who make the decision, having never met the claimant. This approach of empowering local VHAs can speed up the claim procedure. The veterans are not supposed to recount the painful/traumatic experiences to VHAs. Instead, the VA can ask for evidence from medical experts responsible for treating veterans with PTSD. The compensation examiner should refer the veterans to qualified therapists after the examination. The appeal process should review any new information before directing the veterans to the courts, which might discourage those in need from applying for service-connected compensation. Additionally, the time limit to appeal within 120 days should be eliminated, enabling the veterans to seek disability benefits as medical problems appear.
Conclusion
The recommended changes could lead to acceptable results described as follows. First, the veterans could receive the VA decisions within 90 days because the local VHAs could handle the bulk of the work. Veterans’ mental health could improve based on collaboration between compensation examiners and therapists. The reviewed appeal process can allow veterans to present new evidence that might prove their conditions are service-connected. In fact, this process can allow veterans who develop service-connected disabilities many years after discharge to receive compensation benefits. This process alongside proposed changes is illustrated in figure 1.
Reference
Barnes, D. K., McCutchen, S. R., Ford, M. A., & McGeary, M. (Eds.). (2007). A 21st century system for evaluating veterans for disability benefits. National Academies Press.
Bodurow, C. C., & Samet, J. M. (Eds.). (2008). Improving the presumptive disability decision-making process for veterans. National Academies Press.
File a claim for service-connected disability compensation. (2022). The State of New York. Web.
How long does it take to get your VA disability claim rating?(2021). Berry Law. Web.
How to file a VA disability claim. (2022). Veterans Affairs. Web.
Kaczmarek, K., & Romaniuk, P. (2020). The use of evaluation methods for the overall assessment of health policy: Potential and limitations. Cost Effectiveness and Resource Allocation, 18(1), 1-12.
Landes, S. D., London, A. S., & Wilmoth, J. M. (2021). Service-connected disability and the veteran mortality disadvantage. Armed Forces & Society, 47(3), 457-479.
Panangala, S. V., Shedd, D. T., Moulta-Ali, U. (2014). Veterans Affairs: Presumptive service connection and disability compensation. Congressional Research Service. DIANE Publishing.
Redd, A. M., Gundlapalli, A. V., Suo, Y., Pettey, W. B., Brignone, E., Chin, D. L., Walker, L. E., Poltavskiy, E. A., Janak, J. C., Howard, J. T., Sosnov, J. A., & Stewart, I. J. (2020). Exploring disparities in awarding VA service-connected disability for post-traumatic stress disorder for active duty military service members from recent conflicts in Iraq and Afghanistan. Military Medicine, 185(Supplement_1), 296-302.
Rosen, M. I. (2011). Compensation examinations for PTSD—an opportunity for treatment? Journal of Rehabilitation Research and Development, 47(5).
Spinola, S., Fenton, B. T., Meshberg-Cohen, S., Black, A. C., & Rosen, M. I. (2021). Comparison of attitudes towards the service connection claims process among veterans filing for PTSD and veterans filing for musculoskeletal disorders. Medicine, 100(35).
The VA appeals process. (2022). Veterans Disability Info. Web.