Introduction
A variety of disorders do not affect only one system of one’s body. Instead, their alterations influence multiple systems, for example, changing the ways a person moves, breathes, and thinks. Chronic obstructive pulmonary disease (COPD) is a condition that mainly alters an individual’s lungs (respiratory and pulmonary functions) (Hammer & McPhee, 2014). However, it also has an impact on the cardiovascular system, often leading to such complications as pulmonary heart disease (cor pulmonale) (Huether & McCance, 2017). Genetics and old age can affect the disorder’s development, but one of the chief contributing factors is behavior (Celli et al., 2015). COPD is a chronic disorder that creates problems with the respiratory and cardiovascular systems of the body, and its treatment should acknowledge various patient factors in order to control the symptoms.
Disorder and Alterations
COPD is a serious condition that can be prevented but cannot be reversed. It is one of the five most common causes of death in the world (Kew & Seniukovich, 2014). A person with COPD experiences shortness of breath and cough in the majority of cases. There are two kinds of COPD – chronic bronchitis characterized by a persistent cough and mucus production and pulmonary emphysema defined by consistent shortness of breath (Hammer & McPhee, 2014). Moreover, individuals may experience exacerbations of the disorder that may be affected by an infection or an irritant (Barnes, 2016). The leading cause of COPD is tobacco smoking, although others include environmental pollution, irritants such as smoke, fumes, or dust, and a genetic predisposition of alpha 1-antitrypsin (AAT) deficiency (Celli et al., 2015).
Pathophysiology of Alterations
Inhaled irritants cause the inflammation of the airways, and the bronchial wall fills with white blood cells such as macrophages and neutrophils. If the inflammation of the epithelium is continuous, the bronchi develop edema, the airways become narrow, and the smooth muscle thickens and increases in size. Moreover, the enhanced activity of proteases leads to the destruction of elastin. In bronchitis, the main processes involve mucus secretion and bacterial colonization which contribute to the edema. In emphysema, the bronchial walls lose their elasticity, and the lungs trap the air inside, disrupting the ventilation-perfusion balance. The obstruction results in a cough since a person tries to clear the airways from mucus and dyspnea due to the lack of air exchange. Dyspnea lowers the level of oxygen in the blood, narrowing the arteries and damaging the capillaries, which causes pulmonary heart disease (Huether & McCance, 2017).
Patient Factors: Genetics and Age
The inherited deficiency of AAT is one of the causes of emphysema. It is not common, constituting less than 3% of all cases (Huether & McCance, 2017). Nonetheless, this genetic predisposition causes people younger than 40 years old to develop COPD. Moreover, it also can exacerbate the condition even if a person does not smoke or encounter any environmental irritants. In the majority of cases, COPD accumulates symptoms with age, often being diagnosed in patients older than 40 years old (Celli et al., 2015). The process of diagnosing COPD should include the patient’s age and genetics, as these factors affect one’s pulmonary functions.
Patient Factors: Ethnicity and Gender
Such factors as ethnicity and gender contribute to the rates of COPD as well. Nonwhite people report fewer cases of COPD than whites (Hammer & McPhee, 2014). Gilkes et al. (2016) confirm this observation and state that white participants were twice as likely to have COPD as black people. It is also possible that one’s ethnicity may be connected to the genetic factor mentioned previously (Hammer & McPhee, 2014). Furthermore, the statistics indicate that men have a higher prevalence in developing COPD than women (Hammer & McPhee, 2014). It is unclear whether this correlation depends on people’s behavior and exposure to various chemicals. Both ethnicity and gender should be acknowledged in assessing patients’ pulmonary health.
Patient Factors: Behavior
People’s behavioral and environmental factors are among the main contributors to the development of COPD. Smoking is considered as the central cause of pulmonary problems – tobacco use is a habit that is contributed to many respiratory diseases, including COPD (Huether & McCance, 2017). In fact, smoking cessation is the first recommendation for people who are at risk of or have developed COPD. Other irritants such as fumes and dust are also considered as part of one’s behavior because the exposure to them is often connected to one’s occupation and lack of protective gear (Hammer & McPhee, 2014). If possible, people should avoid breathing polluted or contaminated air and wear protective masks in places with irritants. One’s behavior plays a substantial role in preventing and managing COPD.
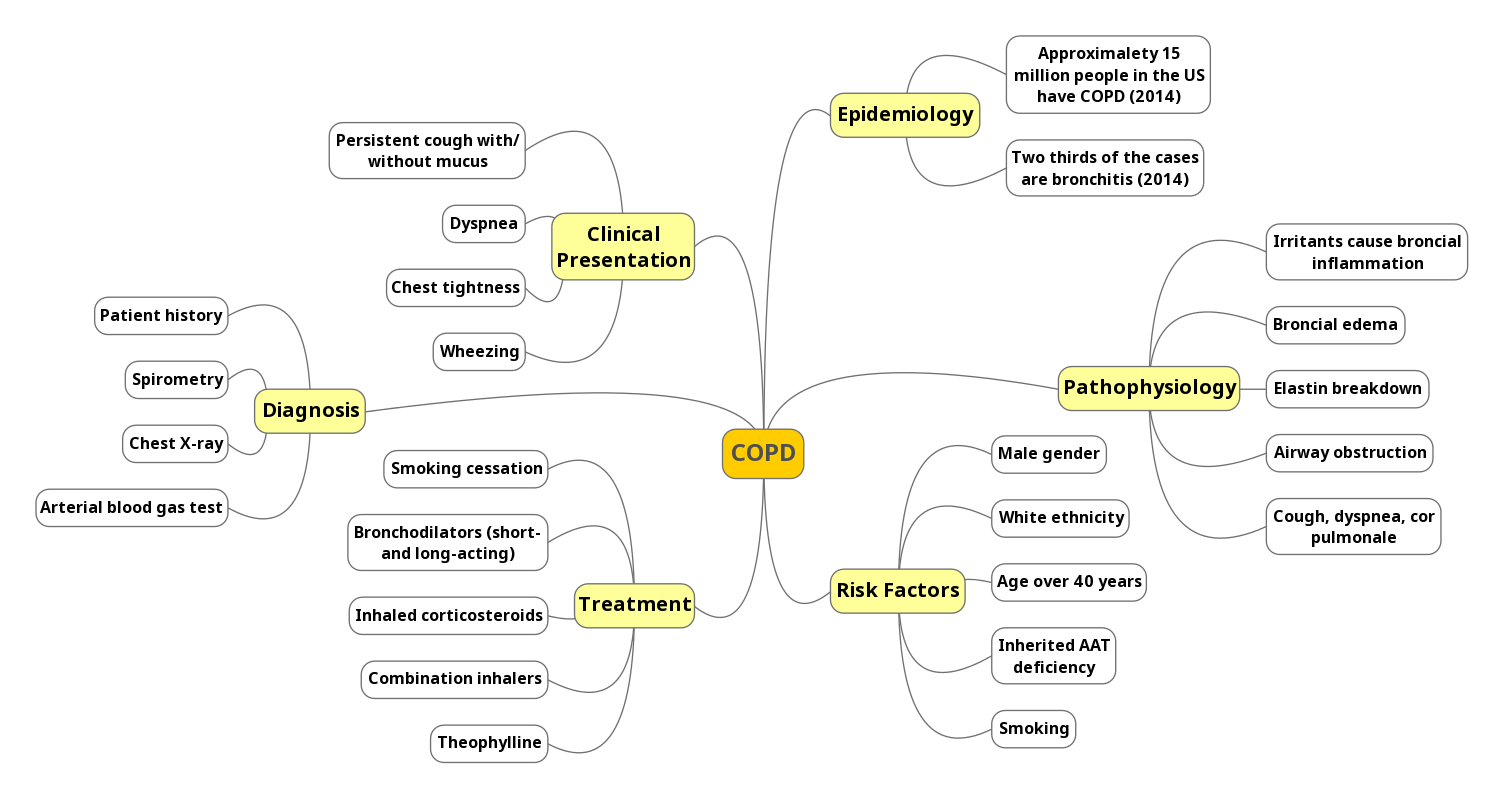
Mind Map
Conclusion
COPD is a chronic condition that is characterized by the obstruction of airways. It is caused by irritants such as tobacco smoke or fumes as well as some genetic factors. Older adults, men, white people, and smokers are at high risk of developing COPD. The alterations of this condition include a cough, mucus, dyspnea, and cor pulmonale, meaning that COPD affects the respiratory and cardiovascular systems of the body. This disorder can be prevented with lifestyle changes, and its treatment assists people in controlling the symptoms and avoiding exacerbations. The alterations of COPD can have a significant effect on people’s everyday lives, and its prevention provides more satisfactory results to patients than its management.
References
Barnes, P. J. (2016). Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. Journal of Allergy and Clinical Immunology, 138(1), 16-27.
Celli, B. R., Decramer, M., Wedzicha, J. A., Wilson, K. C., Agustí, A., Criner, G. J.,… ZuWallack, R. L. (2015). An official American Thoracic Society/European Respiratory Society statement: Research questions in chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine, 191(7), e4-e27.
Gilkes, A., Ashworth, M., Schofield, P., Harries, T. H., Durbaba, S., Weston, C., & White, P. (2016). Does COPD risk vary by ethnicity? A retrospective cross-sectional study. International Journal of Chronic Obstructive Pulmonary Disease, 11, 739-746.
Hammer, G. D., & McPhee, S. J. (2014). Pathophysiology of disease: An introduction to clinical medicine (7th ed.). New York, NY: McGraw-Hill Education.
Huether, S. E., & McCance, K. L. (2017). Understanding pathophysiology (6th ed.). St. Louis, MO: Mosby.
Kew, K. M., & Seniukovich, A. (2014). Inhaled steroids and risk of pneumonia for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews, 3, CD010115.