The Purpose
For this session, we will try to:
- to examine the validity of the selected Patient Treatment Form [PTF] when used with Traumatic Brain Injury Patients.
Assessment
Assessment will be correlated with other well-normed and well researched rating scale:
- Neurobehavioral Cognitive Status Examination [Cognistat];
- Functional Independence Measure [FIM];
- Other NeuroCognitive Screening Tools.
Correlation
- Patient Treatment Form;
- Cognistat;
- other cognitive screening tools;
- FIM (valid for measuring the brain injured population).
Provide health professionals a useful clinical tool focused on cognitive functioning to use in treatment and vocational planning, and rehabilitation outcome assessments.
If it is found that the Patient Treatment Form is correlated to the Cognistat and other cognitive screening tools, and FIM (valid for measuring the brain injured population).
- this would provide health professionals a useful clinical tool focused on cognitive functioning to use in treatment and vocational planning, and rehabilitation outcome assessments.
PTF is a useful tool
- in offering a comprehensive conceptualization of functioning and disability associated with health conditions;
- incorporating evaluations from all staff members associated with the care of the patient on a weekly basis, instead of relying solely on the intake assessment of the FIM.
Cognition &Mental Status Exams
Mental status examinations are a series of detailed but simple questions designed to test cognitive ability, the patient’s state of:
- consciousness;
- appearance;
- general behavior;
- mood;
- content of thought.
Mental status examinations are a series of detailed but simple questions designed to test intellectual resources such as orientation with reference to:
- time,
- place, and
- person and
- comprehension (Koelfan, Freund, Dinter, & Schmidt, 1997).
The patient may be:
- asked to remember objects that had been listed earlier in the course of the exam,
- repeat sentences,
- solve simple mathematical problems, or
- copy a three-dimensional drawing.
When speech and language are tested:
- the examiner listens to the character and fluency of the speech,
- the patient’s ability to understand
- and carry out simple or complex commands,
- and to read and write.
In addition to specific questions that make up the actual mental status exam, it is also important that the examiner observes the patient’s general behavior during the examination (Showalter, & Netsky, 2000).
Patient Treatment Form
- developed as a rating scale for assessing cognitive issues of the brain injured patient;
- assist staff towards effective rehabilitation;
- developed and modified to conceptualize functioning;
- compliment the use of diagnostic labels;
- to portray a patient’s health as a dynamic interaction between functioning and disability.
The Patient Treatment Form is developed as a rating scale for assessing cognitive issues of the brain injured patient, thereby assisting staff towards effective rehabilitation.
The Patient Treatment Form was developed and modified to conceptualize functioning and compliment the use of diagnostic labels and to portray a patient’s health as a dynamic interaction between functioning and disability.
- rating scale is utilized weekly at patient staff meetings to evaluate the progress of the patient,
- and offer a standardized framework for communicating clinical assessments to professionals directly associated with the health of the patient, administrators, and health care providers.
Therefore, the patient’s functional status is a more reliable indicator of service needs and treatment outcomes than diagnosis alone, and diagnosis should not be the determining factor for considering the eligibility of psychologists to provide services aimed at improving functioning (Peterson, 2005).
PTF measures various areas of cognitive levels through items relating to the patient’s
- orientation,
- awareness,
- attention,
- memory,
- problem solving and
- reasoning,
- executive function,
- visual perception,
- comprehension,
- expression, and social / behavior emotional competencies.
Neurological Cognitive Status Examination
- is a screening assessment that is used to determine cognitive ability.
- First uses a variety of independent tests to assess a patient’s level of consciousness, attention, and orientation.
- then it evaluates the patient’s level of functioning in five cognitive ability areas.
The Neurological Cognitive Status Examination is a screening assessment that is used to determine cognitive ability.
This assessment first uses a variety of independent tests to assess a patient’s level of consciousness, attention, and orientation.
Then it evaluates the patient’s level of functioning in five cognitive ability areas:
5 cognitive ability areas:
- Language,
- Constructions,
- Memory,
- Calculations
- and reasoning.
Attention
- to devote mental power on the things happening around you.
Neurobehavioral examination
- typically assess your attention span by asking you to perform simple mental tasks.
Your ability to devote mental power on the things happening around you is called your attention.
This is a complex subject.
The neurobehavioral examination will typically assess your attention span by asking you to perform simple mental tasks.
For example, your ability to count or to recite the alphabet is very rudimentary skills requiring attention.
The digit span task requires that you repeat the numbers after your examiner calls out a short list.
A more complex skill, involving a great deal of concentration, is to recite a series of numbers or letters in reverse order (e.g., spelling a word backwards or reciting the days of the week or months of the year in reverse order).
Orientation
- The ability to pay attention is critical for gathering data: day of the week, month of the year, current year, and one’s present location. These data are classified under orientation.
- A person’s ability to orient self in the world, and to be able to pay attention to it are fundamental skills required for virtually all other aspects of one’s mental and cognitive life.
A person’s ability to pay attention is critical for gathering information such as the day of the week, month of the year, current year, and one’s present location.
This data are all classified under the heading Orientation.
A person’s ability to orient yourself in the world, and to be able to pay attention to it are fundamental skills required for virtually all other aspects of one’s mental and cognitive life.
Person’s ability to communicate
- one of the most important human qualities.
- Involuntary aspects of speech:
- being able to make sounds;
- holding your mouth in the proper position to form those sounds into meaningful parts of speech.
A person’s ability to communicate with others is one of the most important human qualities. There are involuntary aspects of speech, such as being able to make sounds, and holding your mouth in the proper position to form those sounds into meaningful parts of speech.
In speech output, the appropriateness can be judged in terms of:
- Content,
- Speed,
- Clarity,
- Other factors.
Once there is some evidence of speech output, the appropriateness of this output can be judged in terms of content, speed, clarity, and other factors.
Reading and writing ability patient should be able to:
- name objects in their environment;
- repeat words, phrases, or sentences;
- comprehend and answer questions;
- use reasonable grammar and syntax.
A person’s reading and writing ability may also need to be assessed. A patient should be able to name objects in their environment, to repeat words, phrases, or sentences, to comprehend and answer questions, and to use reasonable grammar and syntax, which are all important components of the language assessment.
Memory the ability to store and retrieve information of all types:
- Pictures,
- Movies,
- Sounds,
- other images in the patient’s brain,
- events,
- situations, all in the appropriate time-sequenced order,
- material that the person learned throughout a lifetime.
Memory includes the ability to store and retrieve information of all types. This can include pictures, movies, sounds, or other images in the patient’s brain.
It can also include events and situations, all in the appropriate time-sequenced order.
It might involve material that the person learned throughout a lifetime.
Neurobehavioral Examination
- Assess the memory in terms of its storage of new information, retrieval of information from memory that has been stored, and ability to recognize information that has not been retrieved properly.
- Passing the screening means skill is considered intact and no further testing of that specific skill is required.
- Upon failure, a series of questions asked will provide a quantitative evaluation of the level of disability.
The neurobehavioral examination will assess the memory in terms of its storage of new information, retrieval of information from memory that has been stored, and ability to recognize information that has not been retrieved properly.
If the patient passes the screening for a particular skill, then that skill is considered intact and no further testing of that specific skill is required.
If the patient fails, a series of questions asked that will provide a quantitative evaluation of the level of disability.
Cognistat
- Designed to focus on the degree of disability.
- A space is provided on the examination for the explanation of factors that may have affected the patient’s performance on the exam:
- medications the patient is taking;
- any sensory-motor deficits they may have;
- performance anxiety.
The Cognistat was designed to focus on the degree of disability.
The test does not discriminate between average and superior performance, therefore, the range of scores within the non-disabled population is very small (Doninger, Bode, Heinemann, & Ambrose, 2000).
At the end of the examination, there is space provided for the examiner’s explanation of factors that may have affected the patient’s performance on the exam, such as medications the patient is taking, any sensory-motor deficits they may have, or performance anxiety.
Neurobehavioral Cognitive Status Examination
- A new approach to cognitive assessment designed to briefly provide an assessment of patients who are thought to be behaviorally disturbed.
- The examination has been revised six times since its implementation.
- The exam can be done by most physicians and is only part of the clinical examination process.
The Neurobehavioral Cognitive Status Examination is a new approach to cognitive assessment that was designed to briefly provide an assessment of patients who are thought to be behaviorally disturbed.
The examination has been revised a total of six times since its implementation.
The exam can be done by most physicians and is only part of the clinical examination process.
The Cognitive Status Exam refers to the component of the process that assesses the factors mentioned earlier.
Functional Independence Measure
- is well known through out the world of mental health and medicine.
- Used to assess the burden of care of patients suffering brain injury and may be unable to live without assistive care.
- Often used in hospitals and mental health facilities to help health care workers in setting goals for patients during their rehabilitation.
The Functional Independence Measure is well known through out the world of mental health and medicine.
It is used to assess the burden of care of patients who have suffered brain injury and may no longer be able to live without assistive care.
This measure is often recommended for use in hospitals and mental health facilities for helping health care workers in setting goals for patients during their rehabilitation.
- measures 18 items across 6 different domains:
- Self care;
- Sphincter control;
- Mobility;
- Locomotion;
- Communication;
- Social cognition.
The Functional Independence measure measures 18 items across 6 different domains.
These domains include self care, sphincter control, mobility, locomotion, communication, and social cognition. The individual is scored on an ordered scale of 7 down to 1 on each item in each domain. A score of 7 is achieved if the individual is able to perform the task independently and 1 indicates that the individual is fully dependent on another to complete the task.
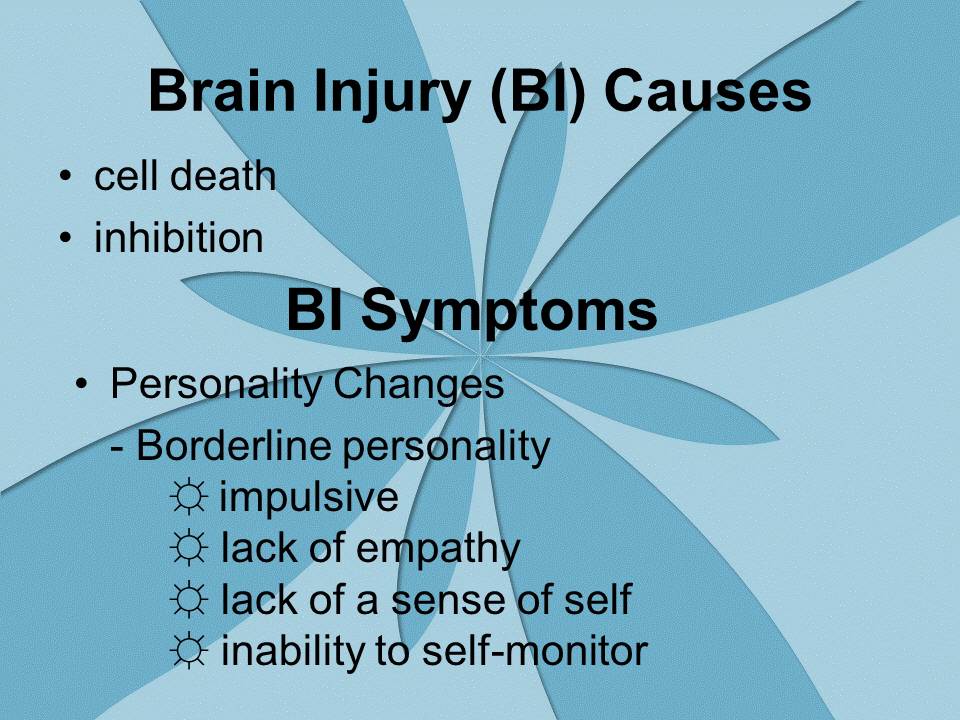
Brain Injury (BI) Causes
- cell death;
- inhibition.
BI Symptoms
- Personality Changes;
- Borderline personality:
- impulsive;
- lack of empathy;
- lack of a sense of self;
- inability to self-monitor.
When a person experiences a BI, the symptoms seen are generally due to two physiological responses, cell death or inhibition.
Several different types of symptoms are associated with BI. Personality changes have been seen as the most significant problem, (Livingston, Brooks & Bond, 1985). Patients with frontal lobe dysfunction may exhibit Borderline personality traits such as impulsively, lack of empathy, lack of a sense of self, and inability to self-monitor. The individual may display a retardation of the maturation process, so that they seem childish.
BI Symptoms
“Chameleon” quality
Person assumes behavioral characteristics based on the individuals in the immediate environment.
- difficulty in perceiving social situation;
- difficulty with self-control and monitoring;
- stimulus bound;
- emotional changes;
- incapacity to learn from social experiences.
Symptoms associated with BI include Personality changes, (Livingston, Brooks & Bond, 1985).
In 1978, Lezak described several differences in personality following a TBI; difficulty in perceiving social situation, difficulty with self-control and monitoring, stimulus bound, emotional changes, and incapacity to learn from social experiences.
- difficulties with abstract thought;
- loss of a sense of humor;
- difficulty to maintain one set of information;
- perform a simultaneous comparison of another set of data;
- impairment in capacity to encode incoming data;
- language disturbances.
Frontal lobe injuries may result in difficulties with abstract though and a loss of a sense of humor. This may be due to a difficulty to maintain one set of information and perform a simultaneous comparison of another set of data (Andrews, 2001).
Memory usually suffers when a person experiences a TBI. Specifically, the impairment in capacity to encode incoming data resides in the hippocampus. This may be due to the location of the hippocampus, which resides in the anterior temporal lobe when upon impact may force tissue into the sphenodial ridge (Andrews, 2001; Lezak, 1995). Language disturbances are observed in 8%-85% of individuals following a TBI, (Groher, 1977).
Language Disturbances
- verbal memory;
- auditory processing;
- integration and synthesis of linguistic information;
- word retrieval;
- spelling;
- speech spontaneity.
Language disturbances are observed in 8%-85% of individuals following a TBI, (Groher, 1977). Patients usually experience problems with verbal memory, auditory processing, integration and synthesis of linguistic information, word retrieval and spelling. Individuals may also experience a difficulty in the spontaneity of speech (Damasio & Damasio, 2000).