Background, Purpose, and Nature
The lack of behavioral health resources in non-psychiatric facilities represents the larger issue explored within the frame of the project. The discrepancy between mentally unhealthy patients’ needs and staff members’ competencies in non-psychiatric services has been recognized only recently (Irigoyen-Otiñano et al., 2022; L’Esperance et al., 2021). As evidence from acute trusts and urgent care centers suggests, non-behavioral health nurses still encounter patients with complex mental health situations in addition to medical concerns, and their unpreparedness for handling such cases can be problematic (Herbert & Hetherington, 2021; Winokur et al., 2022). This unpreparedness can give rise to diverse nursing practice issues, including the inability to address patients’ aggression, adverse events with delusional patients that misunderstand their health concerns, patients’ emotional breakdowns affecting patient flow, attacks on nurses, and other concerns (Herbert & Hetherington, 2021). Its effects on the healthcare system might include care providers’ fear of dangerous encounters and the need for basic behavioral health training for urgent care nurses. This project explored such training as a potentially viable improvement strategy by focusing on the perceived feasibility of this measure.
Research Design and Data Collection
The self-assessment questionnaire and descriptive statistics focusing on the measures of frequency represent the utilized methods. Florence Nightingale’s holistic nursing framework informed the project by emphasizing and problematizing the absence of resources and education for urgent care nurses that would be focused on mental well-being and the nurse’s role in promoting it (Riegel et al., 2021). A three-part questionnaire contained a set of demographic questions and questions regarding the nurse-reported incidence of encounters with problematic patients. It incorporated self-assessment questions for nurses to quantify their perceived confidence in four competency areas, including suppressing stigma against behavioral health concerns, basic factual/diagnostic knowledge, assessing the need for behavioral professionals’ assistance, and practical skills pertaining to safety-maximizing precautions. The findings were then summarized quantitatively, with an emphasis on the measures of frequency. Such methods were selected to complete the preliminary summary of the issue and assess urgent care nurses’ readiness for behavioral health education prior to teaching program development.
Setting/Context
The project aimed at assessing the need for behavioral health education in urgent care nurses was set at a large urgent care center located in Baltimore, MD. The facility serves adult patients with non-life-threatening conditions that still require prompt medical care, and it does not have specialized resources for behaviorally/mentally challenged individuals in need of urgent care services. The organization employs over 50 RNs, 28 of which were surveyed within the project’s frame. Table 1 details the research sample’s demographic characteristics, including educational levels and experiences.
Table 1: Participant Profile Summary
Results
The results suggest urgent care nurses’ overall positive reactions to the idea of training to develop behavioral health skills and the need for improved practical competencies peculiar to managing mentally unstable individuals. The three visuals presented below add to the understanding of the practice issue by detailing the respondents’ perceptions of their skills and hypothetical education. Figure 1 summarizes the respondents’ opinions regarding behavioral health competency training’s ability to benefit urgent care nurses’ everyday work. Table 2 demonstrates the frequency of encounters with three categories of problematic patients. Finally, Table 3 presents trends in the respondents’ self-assessment with regards to four competency areas peculiar to managing clients with mental health needs and issues.
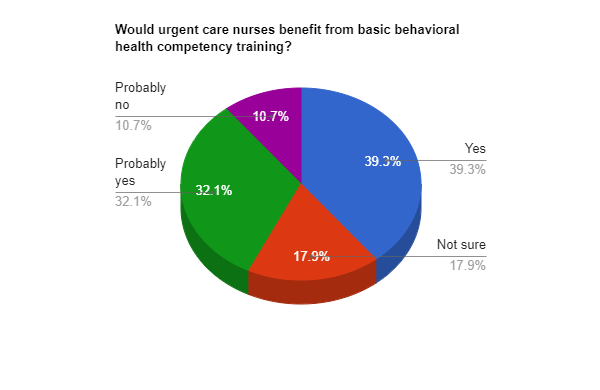
Table 2: Participants’ Encounters with Challenging Cases
Table 3: Knowledge Areas and Trends in the Respondents’ Self-Assessment
Evaluation
Interpretation of Findings
The findings presented above reveal three trends peculiar to the behavioral health resource issue. First, most urgent care nurses perceived behavioral health competency training as a viable intervention that could benefit them and improve their readiness for reacting to unexpected clinical situations and assessing risks when encountering patients in need of behavioral health resources. As Figure 1 demonstrates, no respondents were clearly against the idea or saw it as completely useless. Second, despite working for a facility not intended for mentally unstable populations, the urgent care nurses still encounter difficult-to-manage clients, especially those with clear signs of emotional dysregulation or addiction disorders, which also suggests additional training’s feasibility. Third, nurses’ self-assessment results suggest relatively low confidence in different areas not related to attitudes and stigma. Particularly, when encountering patients with unique behavioral issues, the respondents feel the inadequacy of their knowledge peculiar to common mental health diagnoses’ signs, the ability to distinguish between high-risk and manageable situations, and the understanding of extra precautions required in the case or unique communication strategies to implement. Together, the trends reveal a clear gap in the facility’s current staff training practices.
Translating the Findings into EBP and Impacts on the Project Issue
The findings above can be translated into EBP by informing training development and program evaluation focused on searching for strategies to address urgent care nurses’ specific knowledge and skill gaps, including the understanding of warning symptoms, analyzing the need for external assistance, and the use of extra safety measures. Teaching urgent care providers to recognize mental health conditions that might give rise to explicit aggression, delusional complaints, or rapid mood swings could benefit their overall preparedness for handling challenging cases (Asanova & Khaustova, 2018; Tuominen et al., 2022). Mental health crisis support training for urgent care nurses has been shown to increase the latter’s self-efficacy and professional confidence (Maindonald et al., 2020). With that in mind, another training program to address the aforementioned gaps would offer a meaningful opportunity for applying the revealed trends to practice. Despite the inability to eliminate the main problem, the lack of behavioral health resources for urgent care patients, such training would partially address it by providing staff members with safety-maximizing skills and teaching them to react to challenging situations without high-risk strategies.
References
Asanova, A., & Khaustova, O. (2018). Typical difficult situations in doctor-patient interactions.Psychosomatic Medicine and General Practice, 3(3), 1-11. Web.
Herbert, S., & Hetherington, T. (2021). What do nurses in acute trusts need to provide mental health care. Nursing Times, 117(6), 44-46. Web.
Irigoyen-Otiñano, M., González-Pinto, A., Llorca-Bofí, V., Adrados-Pérez, M., Arenas-Pijoan, L., Torterolo, G., Casalilla, M. S., Buil, E., Nikolau-Subires, E., Albert-Porcar, C., Ibarra-Pertusa, L., & Puigdevall-Ruestes, M. (2022). Increase in urgent care for patients with an eating disorder during the COVID-19 pandemic in a Spanish province.Revista de Psiquiatría y Salud Mental (English Edition), 15(2), 142-146. Web.
L’Esperance, V., Schofield, P., & Ashworth, M. (2021). The provision of additional services in primary care: A cross-sectional study of incentivised additional services, social deprivation, and ethnic group.BJGP Open, 5(1), 1-8. Web.
Maindonald, R., Attoe, C., Gasston-Hales, M., Memon, P., & Barley, E. (2020). Mental health crisis training for non-mental health professionals.The Journal of Mental Health Training, Education and Practice, 15(4), 223-235. Web.
Riegel, F., Crossetti, M. D. G. O., Martini, J. G., & Nes, A. A. G. (2021). Florence Nightingale’s theory and her contributions to holistic critical thinking in nursing. Revista Brasileira de Enfermagem, 74, 1-5. Web.
Tuominen, J., Tölli, S., & Häggman-Laitila, A. (2022). Violence by clients and patients against social and healthcare staff: An integrative review of staff’s well-being at work, implementation of work and leaders’ activities.Journal of Clinical Nursing, 1-12. Web.
Winokur, E., Zamil, T., Loucks, J., Munoz, K., & Rutledge, D. N. (2022). Hospital nurse competency to care for patients with behavioral health concerns: A follow-up study.Journal for Nurses in Professional Development, 38(2), 71-75. Web.