Researchers use theoretical frameworks in their work to identify the problem under investigation. Scholars also use theory to guide the data selection and interpretation process, and to underpin the results they observe after data extrapolation. A review of the two articles by Connelly (2014) and Green (2014) reveals that researchers use theories to support their findings and buttress the importance of the new research.
The research also utilizes theoretical frameworks to guide changes in practice based on the findings. Analysis of the evidence for the proposed study also showed that researchers use theories to provide rationale for the findings and importance of practice change. Some of the theories cited in these resources include Kurt Lewin’s change theory, system’s thinking theory of change, the theory of human caring, Neuman’s system theory, and Peplau’s theory of interpersonal relations. These theories primarily underpin the importance of change within systems by recognizing that the healthcare system comprises various components that must work together to achieve a common goal.
The theories also highlight the process that implementers should follow when initiating change in practice. Theoretical models not only support the change but also provide a guideline on how clinicians can optimize results through the process. There is a common theme that appears in the evidence. For example, the research recognizes that the healthcare system comprises various components, which may compromise the success of the change initiatives if not aligned. Therefore, the theories provide a guideline on how implementers can streamline all these components to achieve the highest effectiveness with the change projects. Another theme that emerges from the analysis is the use of theory to explain the clinicians’ roles and actions toward their patients.
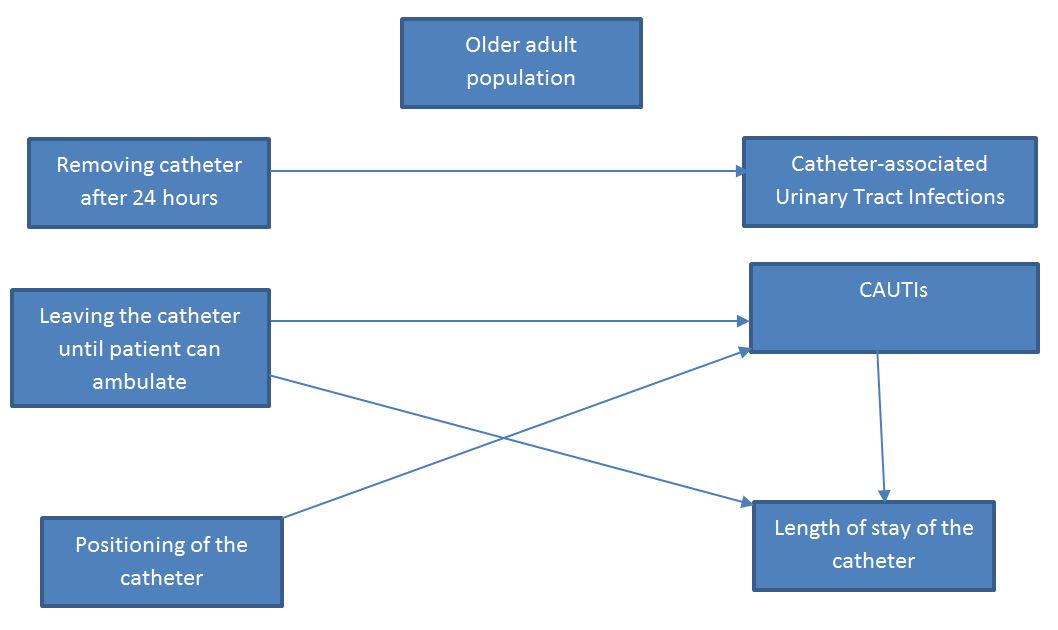
The theory provides rationale for all the actions that practitioners take toward providing care for their patients. The conceptual model below is a representation of a healthcare system, showcasing the relationships and concepts.
Relational Statements
- Removing the catheter 24 hours after insertion reduces the risk of CAUTIs
- The age of a patient increases the risk of CAUTIs
- Leaving the catheter until the patient can ambulate effectively, increases the risk of CAUTI
- Positioning of the catheter influences CAUTIs
- Leaving the catheter longer than 24 hours increases the risk of CAUTIs
References
Connelly, L. M. (2014). Use of theoretical frameworks in research. Medsurg Nursing, 23(3), 187-188. Web.
Green, H. E. (2014). Use of theoretical and conceptual frameworks in qualitative research. Nurse Researcher, 21(6), 34-38. Web.