Introduction
Patient safety is a significant aspect in the delivery of quality care in a patient-centered care system. It is defined as the prevention of harm to patients while placing more emphasis on delivering care that minimizes or stops errors from happening and learn from previous mistakes to avoid the same in the future (Kulinski et al., 2017). Therefore, in essence, patient safety articulates measures that a healthcare organization can develop and implement within the hospital setting to protect its patients from errors, injuries, infections, and accidents. According to a report by the Agency for Healthcare Research and Quality, patient falls are observed as the most common cause of patient injuries, principally in elderly patients (as cited in White et al., 2016). While most of these falls are not intentional, some of such cases can be averted. This report identifies measures that can be implemented by Al Amal Hospital to mitigate patient falls using U-control charts with lower and upper control limits and the mean of ±3 standard deviations.
Background
Falls are becoming an increasingly significant concern in the healthcare sector. As stated in a published survey by the World Health Organization (WHO), many patient falls are preventable in more advanced countries (as cited in Kulinski et al., 2017). Most of these falls are not influenced by poor performance or negligence by the care providing staff but occur because of a lack of effective mitigation strategies in their functional designs. Due to the high costs associated with falls, it is vital to determine strategies that can reduce injuries related to patient care (Florence, 2018). In the United States, patient falls that occur accidentally account for a substantial number of nonfatal injuries associated with older people (Kulinski et al., 2017). Patients above the age of 60 tend to be most vulnerable to the condition.
Objectives of the Study
Al Amal is a general hospital with a bed capacity of 300. On January 1, 2009, healthcare management introduced an obligatory incident conveying scheme and a fall prevention program two years later. The data on patient falls, the number of discharges, and occupied bed days per month for January 2009 through December 2011 was provided. In this sense, the study aims at identifying measures that can be put in place to prevent patient falls using a U-control chart with lower and upper control limits and a mean of ±3 standard deviations.
The Need for a Control Chart in Falls Prevention
In most cases, the financial spending used in treating and containing falls is excessive. Citing from a report by White et al. (2016), a larger proportion of patients treated for wounds and damages associated with falls account for 15 percent of hospital admissions. Implementation of an effective fall prevention program for patient safety will help patients, their families, and society to minimize the unnecessary spending of funds to treat the condition (White et al., 2016). Therefore, incorporating U-charts as a prevention mechanism is an effective strategy to help fall patients manage their anxiety and reduce their inactiveness. Successful implementation of this program will ensure that patients have a clear understanding of their surroundings, become more fit by undertaking numerous physical activities and attain balance, thereby reducing the prevalence of falls.
Reasons for Selecting the U-Chart
Notably, the U-chart was the most appropriate control chart for this report. This is because it is mostly utilized when monitoring the proportion of unconventionality regarding samples of units obtained from a condition such as falls based on days, months, and weeks. Suman & Prajapati (2018) assert that it is crucial in this report because it purposely examines a single unit for a nonconformity. It is a simple graphical tool that facilitates the monitoring of process performance. Its design assists a researcher in determining the type of variation existing in a process. Moreover, they are not only simple to construct and interpret, but they also help highlight critical aspects of performance, which need further investigation.
Methodology
This report utilized the U-control chart to analyze the data from Al Amal Hospital. The study used the method of control carts in the analysis of the data. Control charts are an efficient method of analyzing performance data to assess a process (Smith, 2019). The study used the data to draw a U-chart after selecting the most appropriate type of chart and justifying the selection. A graph representing patient fall was also drawn, followed by the setting of the control limits. The use of the control chart as a useful prevention tool can be evaluated based on the analysis. Data from 2009 to 2011 can be collected and analyzed to determine the effectiveness of this fall prevention program. In essence, data showing the number of patients’ falls recorded, the number of discharges, the number of hospital readmissions, and the number of fall-related readmissions will be significant for assessing the program.
Results and Discussions
- The fall rates were calculated by dividing the number of falls by the number of occupied bed days in each month. For instance, the fall rate for January 2009 was:
- Numbers of falls = 60 = 0.009803922
- Number of occupied bed days 6120
- The average fall rate was calculated by dividing the sum of all the fall rate by the total number of occupied bed days
- Sum of fall rate = Average
- Sum of occupied bed days
- The standard deviation was calculated as follows:
- SD = SQRT([Average] / [Number of occupied bed days])
- The upper and lower control limits were calculated with a mean of ±3 standard deviations as follows.
- UCL = [Average] + 3*[Standard Deviation]
- LCL = [Average] – 3*[Standard Deviation]
The results of the calculations of fall rates, averages, standard deviation, and upper and lower control limits are presented in the table below.
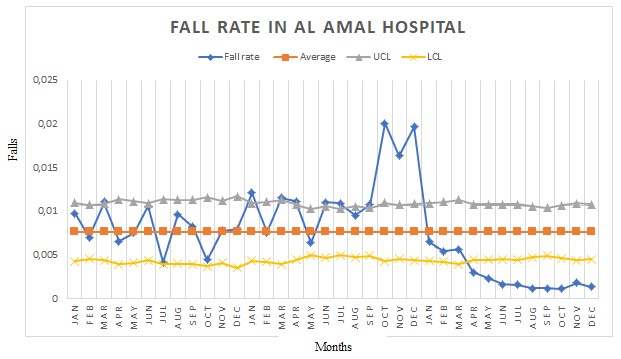
The U-control chart below was obtained based on the calculated data, revealing that the highest number of falls was experienced in 2010, with the highest fall rate of 0.02 recorded in October and December. On the contrary, the lowest number of falls was observed in 2011 between Augusts and December. Based on the data, there are outliers and special cause variation within the analysis because the graph is not in control, considering that some of the monthly data are recorded outside the centraline. For instance, in 2010, outliers were observed in January, March, April, June, July, September, October, November, and December, with October having the maximum outlier range of 0.02. Similarly, there were outliers in 2011 from April to December with August, September, and October, each having the minimum outlier range of 0.001.
Additionally, special cause variation was evident because of the abnormal increase in the rate of falls. For example, in 2010, the fall rate suddenly increased in October, November, and December at high values of 0.02, 0.017, and 0.019, respectively, that broadly vary from the zero target. Notably, the abnormalities occurred because some deviations made the control limits to be surpassed. On the other hand, the fall prevention program’s implementation caused another special cause variation from April to December of 2011. This impact is evidenced by the sudden drop of the fall rates below the center line and below the lower control limit to a minimum value of 0.001 in August, September, and October. This positive change is good since it aligns with the objective of reducing the fall rate towards the zero point at Al Amal Hospital.
On that note, the outliers and special cause variation imply the need for Al Amal Hospital to adjust its control limits. Citing from Saghir & Lin (2015), this approach will help the hospital accurately determine when the control chart strategy becomes unstable towards fall prevention when it lands outside the control limits. Furthermore, the special cause variation means that the hospital must investigate its control limits and make appropriate corrections to improve the U-control chart’s effectiveness. Besides, this signals the hospital’s urgency to develop an unpredictable factor in the control chart that has not yet been accounted for by the current control limits to reach the target, which is zero.
Conclusion
This report determines measures that can be put in place to prevent patient falls using a U-control chart with lower and upper control limits and a mean of ±3 standard deviations. The U-control charts analysis reveals that there were outliers and a special cause variation because all the graphs were not control considering that some of the monthly data were recorded outside the centraline. Furthermore, deviations were observed in the variables, thereby surpassing the control limits.
References
Florence, C. S., Bergen, G., Atherly, A., Burns, E., Stevens, J., & Drake, C. (2018). Medical costs of fatal and nonfatal falls in older adults. Journal of the American Geriatrics Society, 66(4), 693-698.
Kulinski, K., DiCocco, C., Skowronski, S., & Sprowls, P. (2017). Advancing community-based falls prevention programs for older adults—the work of the Administration for Community Living/Administration on Aging. Frontiers in public health, 5, 4.
Saghir, A., & Lin, Z. (2015). Control charts for dispersed count data: An overview.Quality and Reliability Engineering International, 31(5), 725-739.
Smith, E. S. (2019). Introduction to statistical quality control. (2 ed). London: Oxford University Press
Suman, G., & Prajapati, D. (2018). Control chart applications in healthcare: A literature review. International Journal of Metrology and Quality Engineering, 9, 5.
White, K. M., Dudley-Brown, S., & Terhaar, M. F. (2016). Translation of evidence into nursing and health care. (1 ed.). Springer Publishing Company.