Background and Aim
There is an increase in the elderly population in Australia, and they require significant medical care. At the same time, according to the Royal Commission’s Final Report into Aged Care Quality and Safety, mental health care is of the lowest quality, which signals the need for change (Searle, 2021). Access to psychological care, the role and responsibilities of service providers, and the management of mental health care are among the gaps and challenges in the field (Searle, 2021). Reform of the existing care system for the aged population can solve these problems.
Inadequate quality of care is associated with widespread mental health problems in the older population. According to a review by Better Place Australia (n.d.), 30-50% of people in this age group suffer from depression. At the same time, studies by Creighton et al. (2018) indicate that the prevalence of “threshold and subthreshold anxiety disorders was 19.4% and 11.7% respectively” (as cited in Better Place Australia, n.d., para. 7). The pandemic COVID-19 suggests growth in anxiety levels and increased risks of mental health problems in the older generation (Goh & Dow, 2020). An essential factor is that it is difficult for more aged people to discuss mental issues with health care providers due to the stigma of the mental problems. These facts point to the importance of providing quality services to the older generation in maintaining their mental health.
Based on the presented background, the study aims to determine healthcare providers’ readiness to work with mental problems in the older generation. Thus, population (P) is patients of the aged care sector, intervention (I) is personnel’s equipment and training, and outcome (O) is caring for patients with mental health problems, with nothing for comparison (C). Therefore, the PICO question: ‘for patients of the aged care sector, is current personnel’s equipment and training enough to care for people with mental health problems?’.
Method
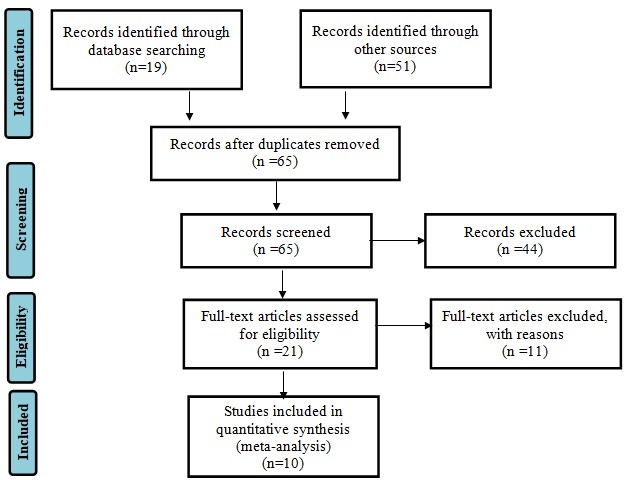
The study begins with the search for the literature necessary to achieve the goal and reveal the topic. Databases such as PubMed and PubMed Central (PMC) were the primary sites for searching for literature on the issue. Additional sources for the search were Google and Google Scholar search engines, and publications dates were limited to 2017-2021 years. Search terms included: aged care sector patients, mental health problem, mental health, Australian aged care sector, staff and nurses training, staff and nurses’ equipment, care for elderly patients’ mental health. The total number of literature for selection also included sources found through other articles and references in them.
Initially, 67 records were found from all sources using key terms, of which 63 were left after duplicates removal. Screening of 63 articles allowed an additional 42 papers to be excluded, which meant that 21 sources remained for thorough verification with the Critical Appraisal Skills Program (CASP). CASP checklists (n.d.) provide tools for evaluating different types of research, such as qualitative, review, cohort study, and other papers. Through the questions, checklists helped select the most reliable and suitable sources, and the final result includes ten articles.
The main inclusion criteria are:
- publication in a peer-reviewed journal;
- English language;
- be published within the last five years;
- the appropriate age of the groups studied – the older generation;
- the studying patients with mental health conditions or the desire to contact mental health specialists;
- the disclosure of the topic of quality of health services;
- having significant implications for practice.
Sources that focused on the treatment process (rather than quality) or described only factors causing the condition or complications were excluded.
Results
Discussion
This review includes ten studies to understand better how modern health care providers are ready to work with older adults with mental problems. The study by Amare et al. (2020) provides an idea of the prevalence of mental disorders in the Australian older generation – in the cohort studied, almost 58% had various conditions. Currently, access for the older generation to professional psychological care is insignificant (Dawson et al., 2017; Stargatt et al., 2017; Tabatabaei-Jafari et al., 2020). However, current technologies allow increasing access, as demonstrated by Christensen et al. (2020). There is considerable prejudice against both older people and people with mental problems, which manifests itself in discrimination, ageism and negatively affects the group’s quality of life (Benjenk et al., 2019; Lyons et al., 2017; Rush et al., 2017; Smith et al., 2019; Temple et al., 2021). Thus, most studies indicate a lack of knowledge and training among professionals.
Discrimination and prejudice against the older generation and mental problems limit access to health care. Benjenk et al. (2019) and Rush et al. (2017) note significant negative beliefs in nursing students against both groups, affecting their choice of work direction. As a result, the area of psychological assistance for the older generation has a staff shortage, which is also noted in research by Dawson et al. (2017) and Stargatt et al. (2017). At the same time, studies reporting negative relationships focus mainly on nurses. Participants of Smith et al. (2019) survey, in turn, also included psychologists, psychiatrists, and social workers. Although these professionals were more friendly to the older population, particularly LGBT representatives, they also noted a lack of knowledge (Smith et al., 2019). These facts suggest gaps in the training of various professionals.
Conclusion
Mental health problems carry the risk of physical health problems for the older generation up to early death, which justifies the need to study the issue carefully. This survey points to significant problems in providing professional psychological assistance to the elderly. Politicians and representatives of medical services should pay attention to training and expand their programs with themes of care for older adults with mental health disorders. Given the nation’s aging and the increase in the number of older populations, there is the urgency of drawing attention to the problem.
The current review has limitations since a small amount of literature is devoted to preparing staff to work with older people with mental problems. Although the sources studied are relevant to the topic, future studies may concentrate on physicians as more focus has been shifted to nursing training. Moreover, attention should be paid to studying methods to make psychological services more accessible for the older generation and allow better education of employees of various specialties. Nevertheless, the significance of the review is in demonstrating gaps and drawing attention to the complexity and multilateralism of the issue.
References
Amare, A. T., Caughey, G. E., Whitehead, C., Lang, C. E., Bray, S. C., Corlis, M., Visvanathan, R., Wesselingh, S. & Inacio, M. C. (2020). The prevalence, trends and determinants of mental health disorders in older Australians living in permanent residential aged care: implications for policy and quality of aged care services.Australian & New Zealand Journal of Psychiatry, 54(12), 1200-1211.
Benjenk, I., Buchongo, P., Amaize, A., Martinez, G. S., & Chen, J. (2019). Overcoming the dual stigma of mental illness and aging: Preparing new nurses to care for the mental health needs of older adults.The American Journal of Geriatric Psychiatry, 27(7), 664-674.
Better Place Australia. (n.d.). Mental health interventions in aged care. The Centre for Better Relationships.
CASP checklists. (n.d.). Critical Appraisal Skills Programme CASP.
Christensen, L. F., Moller, A. M., Hansen, J. P., Nielsen, C. T., & Gildberg, F. A. (2020). Patients’ and providers’ experiences with video consultations used in the treatment of older patients with unipolar depression: A systematic review.Journal of Psychiatric and Mental Health Nursing, 27(3), 258-271.
Creighton, A. S., Davison, T. E., & Kissane, D. W. (2018). The prevalence, reporting, and treatment of anxiety among older adults in nursing homes and other residential aged care facilities. Journal of Affective Disorders, 227, 416-423.
Dawson, S., Gerace, A., Muir-Cochrane, E., O’Kane, D., Henderson, J., Lawn, S., & Fuller, J. (2017). Carers’ experiences of accessing and navigating mental health care for older people in a rural area in Australia. Aging & Mental Health, 21(2), 216–223.
Goh, A., & Dow, B. (2020). People in aged care sector need psychological as well as physical protection. The University of Melbourne.
Lyons, A., Alba, B., Heywood, W., Fileborn, B., Minichiello, V., Barrett, C., Hinchliff, S., Malta, S., & Dow, B. (2018). Experiences of ageism and the mental health of older adults.Aging & Mental Health, 22(11), 1456-1464.
Rush, K. L., Hickey, S., Epp, S., & Janke, R. (2017). Nurses’ attitudes towards older people care: An integrative review. Journal of Clinical Nursing, 26(23-24), 4105-4116.
Searle, L. (2021). Mental health concerns among the most common in Aged Care Royal Commission. Mental Health Australia. Web.
Smith, R. W., Altman, J. K., Meeks, S., & Hinrichs, K. L. (2019). Mental health care for LGBT older adults in long-term care settings: Competency, training, and barriers for mental health providers.Clinical Gerontologist, 42(2), 198-203.
Stargatt, J., Bhar, S. S., Davison, T. E., Pachana, N. A., Mitchell, L., Koder, D., Hunter, C., Doyle, C., Wells, Y., & Helmes, E. (2017). The availability of psychological services for aged care residents in Australia: A survey of facility staff.Australian Psychologist, 52(6), 406-413.
Tabatabaei-Jafari, H., Salinas-Perez, J. A., Furst, M. A., Bagheri, N., Mendoza, J., Burke, D., McGeorge, P., & Salvador-Carulla, L. (2020). Patterns of service provision in older people’s mental health care in Australia.International Journal of Environmental Research and Public Health, 17(22), 8516.
Temple, J. B., Brijnath, B., Enticott, J., Utomo, A., Williams, R., & Kelaher, M. (2021). Discrimination reported by older adults living with mental health conditions: Types, contexts and association with healthcare barriers.Social Psychiatry and Psychiatric Epidemiology, 56(6), 1003-1014.