Introduction
As a developed nation, Canada is experiencing an aging population in its demographics. Due to the advancement in healthcare, more people are living longer than before, despite an increase in the number of chronic illnesses among the senior population. However, according to Hsiao, the share of the population of seniors in Canada is smaller than many other developed western countries (950). The country has been experiencing a rise in its aging population in the last 40 years. Notably, at the beginning of 2011, the first baby-boomers attained the age of 65 years. Hence, the aging population is expected to accelerate very fast onwards. According to Morgan, Daw, and Law, the number of seniors in 2005 was 4.2 million (41). The number is expected to rise up to 9.8 million by 2036. In 2005, the aging population represented 13.2% as of 2005.
It will represent 24.5 % of the whole population by 2036. From 2036-2056, it is projected that the rate of increase in the older population will be slower. It will go up only from 9.8 million to 11.5 million. This increment represents 27.2% of the Canadian population in 2056 (Kutzin, Cashin, and Jakab 17). The increase in the aging population corresponds with the increase in life expectancy in the country. For instance, in 2012, it was estimated that the life expectancy was 81 years as compared to 76 years in 1981. The increase in life expectancy explains the rising number of the aged people in the country. Another major reason why the aging population is increasing is the reduction in fertility rate, which stands at 1.5 children per woman (Steinbrook 1661). This figure is below the replacement level of 2.1 children per woman.
Although the issue of aging population in Canada has come later as compared to other industrialized nations, there are conflicting messages on what an increase in aged population will imply to the provision of health care services and health care expenditure in the Canadian context (Kutzin, Cashin, and Jakab 17). On one side are those who believe that the senior population takes a disproportionate share of the healthcare costs as compared to other populations in the country. Hence, as this population grows, the health care expenditure is likely to explode, thus leading to the collapse of healthcare systems if adequate measures to reconstruct the financing of the sector are not put in place. On the other hand, there are those who argue that the increase in the elderly population is only one element that will contribute to increased health costs. The supporters assert that the other elements are manageable. Thus, if handled well, they will ensure adaptability of the healthcare sector to cater for all people’s health care needs.
In this paper, the impact of the aging population on the healthcare expenditure in Canada will be discussed. Further, the paper will provide recommendations on the future adjustments that will guarantee sustainability of the healthcare subsystem, regardless of the increased costs. Concisely, the paper will show that despite the increase in healthcare spending due to the rising aging population, such changes will not destabilize the health care system because of proper planning to address the outcomes of the changes in the demographics of the nation.
The Elderly Population Representation in Canada
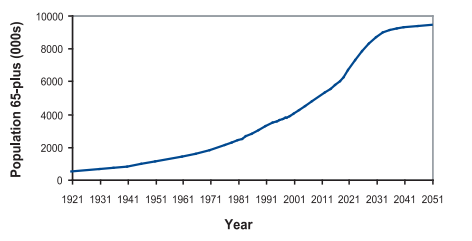
The representation of a given population as part of the whole population is majorly done using percentages. In this case, it is important to represent the elderly population as a measure of the whole population to guarantee a clear understanding of the future health impacts of the population changes. A population is viewed as aging when the people above 65 years are increasing as a measure of the other population (Kutzin, Cashin, and Jakab 18). The graph below represents the change in the population of those above 65 years in the country as a measure of the remaining population since 1920.
Canada’s Population Age 65 Years and above (aggregate)
The above population projections are represented as a percentage of the whole population as shown in the graph below:
Canada’s Population Age 65 Years and above (Percentage)
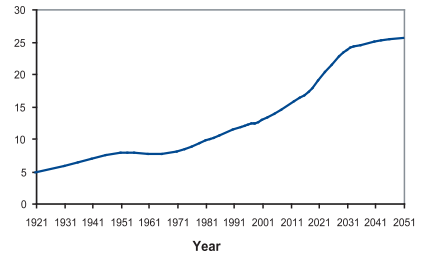
From the information represented above, there were 3.9 million seniors in 2001 that represented 12.6% of the population. The figures represented a rise of 63% from 1981 when the population of seniors (65 years and above) was 2.4 million. In 1921, only 5% of the population was above 65 years of age. The trend in the rise of the senior population is expected to continue in the 21st century with 7 million senior being expected in 2021. The rise will represent 19% of the total population (Sammartin 1133). By 2041, the population of the 65-year-olds and above will represent 25% of the population that will have gone to 9 million people.
Another important indicator of the rise in the number of aging population as a share of the whole population is the dependency ratio. According to Steinbrook, the aging population in the country as a share of the working class is increasing over the years (1661). This rise is a sign of future problems that may affect the economy and the healthcare sector. Since more people depend on the working class, the burden of health care increases on the working. This situation is likely to have an impact on the health care sector, as it will be discussed later. The graph below shows the dependency ratio in Canada as observed since 1971 and as projected up to 2056.
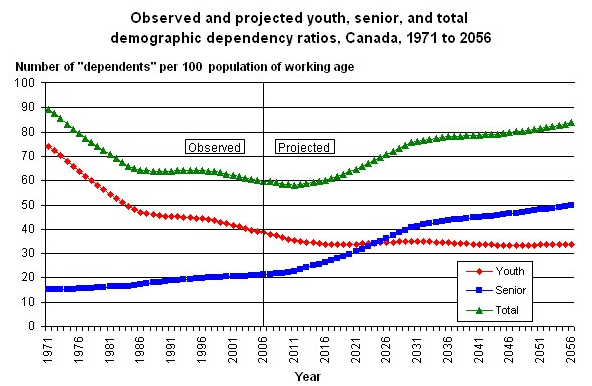
The graph above shows that the dependency ratio of the youths below 15 years has been decreasing. The situation is projected to drop and stabilize at 35 per 100 population of working. Further, the population of the dependants above 65 years has been on the rise. It has wiped out the benefits of the decreasing youth dependency. It is projected that by 2026, the dependency ratio of those below 15 years and/or above 65 years will be equal. Thereafter, senior people will constitute the major share of dependants in Canada.
The median age of a population is an important indicator of an aging population in a country. The median age represents the exact half of the population where one half is older while the other half is younger. Since 1966 when the last baby boomers were born, the median age has been on the rise from a median age of 25.4 years. In 2001, the median age of the population in the country was 37.6 years as compared to 35.3 years recorded in 1996, which represented the largest census-to-census increase of median age in the country (Flood and Haugan 320). Further, the 2.3-year increase in the media age was linked to the decrease in number of births since 1991. Projection shows that the median age will reach 44.8 years by 2030 and 45.8 years by 2050.
The Impact of the Aging Population on Canadian Health Care Spending
From the demographic discussion above, it is important to accept that the Canadian elderly population will continue to grow. Further, since the route is a health deteriorating process, people in this age group will be the greatest consumers of health care services in Canada (Steinbrook 1663). With the high number of elderly people, the implications to the economy and most importantly the health care services and health care budgets will be greatly affected in the country. In this section, the focus is on the projected costs and changes in the health care sector to reflect the changing health care demands in Canada.
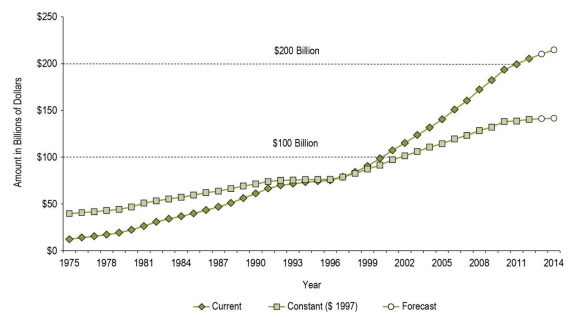
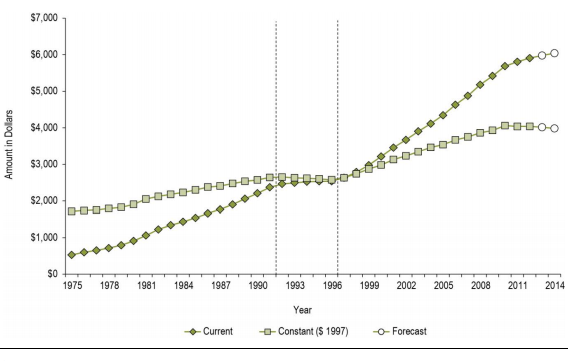
Firstly, the health expenditure in the county has been rising steadily over the years, partly because of inflation, economic changes, and due to the increase in the elderly population. Since 1997, the country’s healthcare spending has been increasing. In 2003, the country spent $121 billion on healthcare, which was an equivalent of $4,000 per person (Kutzin, Cashin, and Jakab 19). During the time, the private health sector accounted for approximately 33% of the total expenditure. In 2001, the county’s healthcare expenditure was equivalent to 10% of the Gross Domestic Product (GDP). According to Morgan, Daw, and Law, the healthcare budget had been projected to increase from $80.7 billion in 2000 to more than $250 billion in 2020 (44). During the same time, it is projected that the provincial and territorial governments’ expenditure will increase from $55.9 billion to $102.5 billion. In total, this increase in healthcare spending will represent 83% rise for the period spanning 20 years. The gravity of this increase in health spending can be well understood when compared to other public expenditures that are only projected to rise by only 36.5% during the same time (Kutzin, Cashin, and Jakab 22). The following graph shows the total healthcare spending in the period 1975-2014:
Total Healthcare Spending 1975-2014
The per capita spending of the country on health care was approximately $4000 in 2003. It increased to $5911 in 2012. In 2015, the total health care per capita reached $6,045 (Morgan, Daw, and Law 46). Between 1997 and 2010, the total health care expenditure per capita grew faster than the population growth and inflation combined. The total healthcare expenditure per capita is represented below:
Per Capita Healthcare Spending in Canada 1975-2014
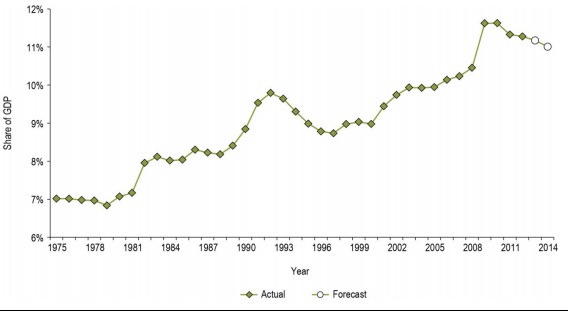
In 2003, the healthcare expenditure was approximately 10% of the GDP. It rose to 11.2% in 2012. In 2013, the healthcare expenditure rose to 11.2% but slowed down to 11.0% in 2014. Since 2000 to 2012, the expenditure on healthcare was rising by an average of $8.9 billion annually (Steinbrook 1662). The graph below represents the healthcare expenditure as a percentage of the GDP in Canada from 1975 to 2014.
Total Health Expenditure as a Percentage of GDP 1975-2014
More than 50% of an individual healthcare spending occurs after the age of 65 years. This observation shows that that an increase in the elderly population in a country will most likely increase the cost of health care. The population of Canada is growing. The elderly population is also increasing drastically. Its projected continued growth will result in higher healthcare expenditure (Hsiao 953). To understand the current healthcare expenditure, it is important to know the current healthcare spending by age and sex in the country. The following graph shows the 2012 total/provincial/territorial government expenditure in Canada.
Total Health Care Expenditure in Canada by Age/Sex in 2012
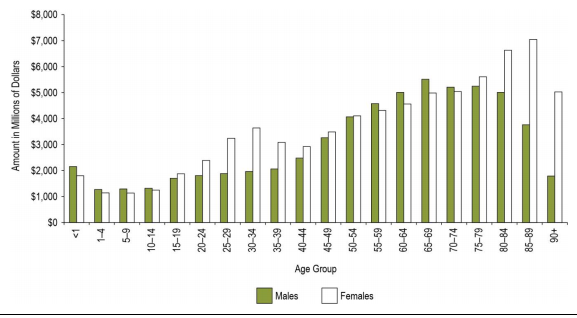
The graph above shows that more money was spent on the healthcare of the elderly than for other age groups in the country. On the other hand, females between the age of 25-34 and above 80 years had more healthcare expenses compared to their male counterparts during the same age groups. The disparity can be explained by the fact that women tend to have more health care costs during their childbearing years, that is, 24-34. Further, since females have a higher life expectancy, there is more expenditure for women above 80 years.
Although it is evident that the increase of 65 years leads to greater health care costs, seniors are a diverse group where the health care expenses vary considerably across the age group. In this case, those above the age of 80 years have the highest health care spending per person.
Government Healthcare Expenditure per Capita, by Age Group, Canada, 2012
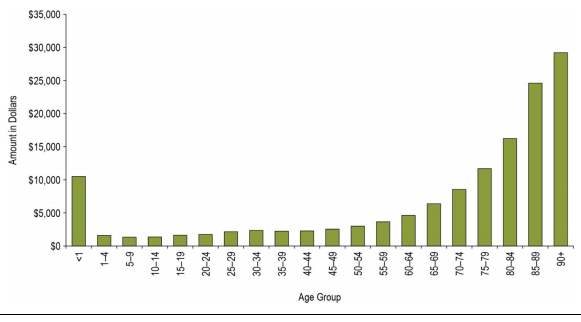
The graph above shows that as people age, there is a significant increase on health care spending. For instance, in 2001 the per capita expenditure on healthcare was approximately was over $17000 for people above 85 years. This figure has risen to approximately $30,000 in 2012 (Morgan, Daw, and Law 48). The seniors above 65 years represent approximately 12.6%, yet they account for approximately 43% of the government spending. The older the person, the higher the healthcare costs they incur.
The development in medical technology is expected to continue exerting more pressure on healthcare spending across all the age groups in the country. However, such a trend will lead to a very sharp increase in health care expenditure for the elderly population whose current healthcare spending is already very high at about three to five times as compared to those below 65 years (Kutzin, Cashin, and Jakab 24). Two demographic factors, namely a high population share of old people and the older people who live longer in their final years, are driving health care cost up. According to Steinbrook, higher medical and hospital costs are incurred at the final period of death (1663). Further, the higher costs of health care are incurred during the final two years of a person’s life. Since older people are living longer, the cumulative healthcare costs are very high due to frail health at this period of age.
One in four elderly people in the country has a long-term disability while a large number suffers from chronic health conditions such as high blood pressure, arthritis, rheumatism, diabetes, dementia, and chronic heart diseases among other illnesses. It is further estimated that more than 500,000 elderly people in Canada will be suffering from Alzheimer’s disease by 2031 (Kutzin, Cashin, and Jakab 25). However, the health of the population and other demographics are not the only factors that amplify the cost of health spending. Instead, other factors such as technology, pharmaceuticals, and public expectations among others can have an impact on the health care costs in a country. Aging alone will contribute to 0.8% increase in health care costs of the 5.3% annual nominal increase in health cost.
Other developed countries are experiencing similar problems in the healthcare systems due to the aging population. In addition, some of the countries such as Japan, France, and the United Kingdom have a higher population of older people. However, they have managed to keep their costs of health care as a share of the GDP lower than Canada’s situation. Evidence shows that despite the increase in aging population, modest growth of economies in most of the developed countries has allowed the health care costs to be controlled.
The Impact of the Aging Healthcare Workforce in Canada
The health care sector is a labor-intensive segment of the economy. Thus, for quality services and care, the health care workforce is critical. The sector faces major challenges in terms of workforce. This challenge is driving the cost of health care in the country. The health care and social service sector employs one in 10 Canadians. However, despite the impressive figures on the number of employees in the workforce, there have been concerns that the sector faces major challenges. The challenges are likely to lead to higher costs in the healthcare sector. The amplified costs will lead to more challenges as the aging population increases.
One of the major challenges facing the healthcare sector is the aging health care workforce in the country. In 2011, the average age of registered nurses was 45 years. Further, approximately 28.4% of the nursing workforce in the health sector was above the age of 55 while 13.4% of nurses were beyond the age of 60 years (Sibley and Weiner 22). Indeed, in 2007, for every nurse who was 35 years or younger, two nurses were above 50 years. The higher age of the health care workforce is a clear indicator of the dire need for workforce in the sector to respond to the rising health needs in the country. With more than a third of the nurses above 50 years, the increasing number of nursing professionals who are retiring by 56 years is a concern for the whole health sector in Canada. Further, due to the increasing cost of the healthcare education, it is worrying that more nurses graduated in 1972 than in 2002, despite the increase in population by more than 50%. As such, in terms of ratio, there were more nurses per population in 1972 than in 2002. There is a large disparity in the distribution of healthcare professionals across region in the country. This situation led to a high inter-provisional competition for healthcare professionals in the country. Such competition has pushed the cost of hiring nurses very high. The healthcare sector has to cater for the increased workforce costs.
As of 2014, there was a shortage of more than 22,000 nurses. The situation was only masked by heavy workload and delayed retirement in the sector (Sibley and Weiner 24). The shortage of nurses in the country will reach 60,000 by 2022. The rise is likely to put the health care sector into crisis. The sector also employs the highest number of part-time workforce of any other sector in the country. For instance, the recommended fulltime-to-part time workforce is 70:30, yet statistical findings show that more than 45% of nurses work on casual/part-time basis in the healthcare sector (Steinbrook 1663).
Long-term Care and Family Support
The increase in aging population not only indicates an increase in dependency ratio in the country but also an increasing burden to families and healthcare sector in providing long-term care and support to the aged. Aging makes people become frail. It also increases their chances to be ill. Hence, they need support to ensure that they can run their daily activities (Morgan, Daw, and Law 46). As such, the long-term care is a major area of concern since it poses a strain on public, family, and personal resources. The support provided to the aging population can be formal or informal. The formal support can be grouped into two areas. The first support is in the form of community-based care, which allows an older person to receive community-based health and social services at home. The second approach to formal support is the institution-based care where the aged receive care in government-provided-and-controlled areas at subsidized costs.
On the other hand, family members, friends, or neighbors provide informal care. In most cases, informal care is largely provided by other elderly people, especially the spouses. It is estimated that the informal support caters for more than 90% of the care needs in the country (Hsiao 956). In this case, more than three million people provide the informal care to the elderly. The projected increase in elderly dependency ratio, as well as the decline in the working people in comparison with the older people is likely to have serious consequences where there are fewer people to take care of the older generation.
In 2014, approximately 16% of the older Canadians are receiving regular long-term care is long-term care facilities where the costs of accessing such services costs more than $3,000 per month, which represents a high cost to families (Sibley and Weiner 26). However, despite the increasing costs of accessing long-term care, very few people at only 12% are protected by long-term care insurance (Morgan, Daw, and Law 46). The cost of care to the elderly will extend to the labor force where those who leave workforce to care for their older relatives will contribute to labor shortage in the country. The shortage will further lead to societal opportunity cost due to the lost productive capacity and tax revenues. It is further suggested that those who provide long-term care in the home setting are likely to develop their health complications. Indeed, in case the spouses were caring for their frail partners, they were likely to die earlier than their counterparts who did not offer such care.
The interest on palliative care has increased because of the increasing aged population in the country. In this case, it is estimated that more than 317,300 deaths will be recorded in 2020 as compared to 227,620 recorded in 2002 (Sammartin 1136). More than 75% of the deaths in Canada occur in hospital environments, yet the beds dedicated to palliative care (end of life care) are very few. Hence, most patients end up in up in acute care beds. Consequently, the situation worsens the already precarious state of affairs in such hospitals. More than 90% of the people in the country prefer to spend their final days at home with their loved ones. However, such a situation requires the family members to spend approximately 54 hours per week with their frail parents. Such time is difficult for one to dedicate due to the strains on resources the elderly already bring to the family.
Restructuring the Healthcare System in Canada
The discussion above shows the dire need for reforms in the healthcare sector in Canada to cater for the needs of the aging population while ensuring sustainability of healthcare financing without compromising the quality of care. As such, there is the need to restructure the health sector through various approaches that target financing, the quality of care, training workforce, and technological advancements.
Restructuring Financing Structure
One of the biggest challenges facing the healthcare sector in the country due to the increase in the aging population is the access to funds to guarantee continuity of the sector. Over the years, the need to reform the financing of the healthcare sector has attracted increasing attention, yet very little has been achieved. According to Sibley and Weiner, some of the analysts in the healthcare sector argue that the increasing costs of health care will be manageable in a growing economy where the government revenues are expected to grow in equal measure (26). However, major concerns have been raised on the pay-as-you-go approach to healthcare budgeting. The approach to budgeting is unsustainable since it places the burden of caring the elderly on the ensuing generations (Kutzin, Cashin, and Jakab 48). Those who oppose the pay-as-you-go approach to budgeting argue that it is important to take action now when the economic conditions are ideal. Surplus budget makes it possible to have such actions undertaken now for future response to the increasing healthcare costs. So far, various options have been suggested to reduce future health costs in the country. These options include reducing health services, increasing taxes or introducing user fees to cover pay-as-you-go healthcare expenses, diverting resources from other sectors, and using the current taxation to pre-fund future health care expenditure.
However, it is unlikely that the public or the government will support the first three options suggested above. The situation suggests a funding gap because of the increased healthcare expenditure. The gap is attributable to the aging population and the falling national income due to the reduced workforce. More people will be moving to the senior age group. To address this gap, the prefunding option is the most appropriate approach. This option focuses on pre-funding of future health care expenditures. Hence, it may be supported. However, various approaches have been suggested under the option of pre-funding of future health care expenditure through the current taxation (Hsiao 957). Firstly, the approach suggests the establishment of seniors’ health grant to be incorporated into the Canada Health and Social Transfer (CHST) body.
This strategy will ensure that the government can allocate money to the provinces in relation to their population that reaches 65 years and above. The grant will be adjusted annually through an accelerator provision that will be tied to the nominal GDP. However, it will require all seniors to have an equal fixed allocation per annum. Another option is the creation of a “seniors’ health account” that will operate in a similar manner since the Canada Pension Plan will grow over the years to fund some of the elderly health care in the country (Sammartin 1138). If adeptly implemented, the two recommendations will greatly help in offsetting the burden that future generations will incur in health care costs towards the elderly population.
Another approach that has been recommended for the prefunding of the future healthcare costs of the elderly is through insurance. Compulsory insurance schemes like the employment insurance would be an important avenue of cost sharing in financing future healthcare expenditure in the aging population.
Lastly, private long-term care insurance is another source of income that is highly viable. The insurance approach ensures accessibility and affordability of care without exerting a lot of pressure on the economy and emotional burden on family members. Such insurance can offer reprieve to families since it can cater for home-based care and provide options to patients who require home-based care. Sibley and Weiner assert that such private long-term care insurance is important for women since they are likely to outlive their husbands and hence more likely to face financial challenges in their widowhood (26).
Primary Care Reform
In the recent past, there has been focus on the improvement of primary care in the country. Primary care represents the entry point into the healthcare system. As such, it is important to dedicate resources, quality, and access to primary care since it is likely to have a major impact on the entire system. When the quality of primary care is good, the health outcomes are likely to reflect in generations since diseases are detected and treated early, thus reducing the number of people with serious health conditions in their old age. Concisely, a robust primary care sector will lead to healthy aging, which will ultimately reduce health care cost in old age.
Human Resource Planning
Major factors have been highlighted as leading to the increased health care expenditure challenges in the workforce in the sector. Some of the concerns include professional shortages, growing recruitment and retention costs, and an aging healthcare workforce. To address this issue, effective human resource planning is very important.
Firstly, there is the need to ensure recruitment of adequate staff members in the country. To increase the recruitment, the major approach that the government should focus on is the training of more professionals in the sector. The number of trained personnel that is graduating from institutions of learning has reduced drastically over the years. As such, promoting more training of healthcare professionals is one way of ensuring that the current challenges concerning workforce shortages are reduced (Flood and Haugan 323). It is projected that institutions of learning will need to graduate approximately 12,000 nurses to keep up with the demand, yet they have been falling short over the years.
For instance, in 2005, only 10,074 nurses graduated. This figure represents a shortfall of approximately 2000 nurses. Such a cumulative shortage can explain the current shortage that reached up to 22000 as of 2014 (Sibley and Weiner 29). More than 60% of the institutions in the country have a shortage of faculty members. The situation has consequently limited the number of students who can be admitted. A further 70% of the institutions have expressed shortage in financing. The situation has a repercussion on the number of students who they can admit. Another study found that 40-50% of the institutions have inadequate space (Sibley and Weiner 24). However, with adequate financing, many of the institutions pointed out they could increase their enrolment by up to 50%, which would consequently lead to more nursing professions among others in the country. Further, the recruitment and retention policies should be re-examined to ensure that they can promote recruitment both internally and externally to attract workforce from within and outside the country.
The second important approach that the healthcare sector should focus on includes strategies that are geared towards improvement of productivity and reduction of costs. Such strategies should include the use technology, upgrading of skills through training, enhancing scope of practice among the existing workforce, and using evidence-based research. For instance, since the nursing workforce comprises the largest share of the healthcare workforce, training them to handle some physicians’ work may be a great step towards a better health care system in the country.
There is the need to focus on the promotion of healthy and safe workplaces. Approximately 12,000 nurses do not attend duties since they are off on injury or illness-related issues (Morgan, Daw, and Law 48). Further, the workload that the nurses have due to the shortages facing the healthcare sector is another area that contributes to low quality of care and the increasing expenditure of healthcare in the country. There is the need to focus on the development of strategies that will lead to healthy workplace initiatives, innovative staffing initiatives such as nurse-patient ratios, workload management systems, and approaches to increasing productivity without jeopardizing the safety of the workers (Sammartin 1139).
For instance, increasing the productivity of nurses will be important to relieve nurses and other practitioners of non-nursing roles such as housekeeping, clerical, and caretaker functions among others than only acting to divert the efforts of nurses from providing healthcare services. This approach is very costly to the economy. Further, it affects the quality of care. Other important approaches include the provision of adequate and up-to-date technologies to ensure that nurses and healthcare providers can deliver health care fast and at high levels of quality. Working in the healthcare environment exposes practitioners to many risks such as disease, harm from patients, and emotional stress among other risks (Flood and Haugan 336). It is important for measures to be put in place to ensure that service providers are safe in their work environments.
Technological Developments
Technological advancement or adoption into the healthcare sector is another area that requires emphasis in the country. There is the need for more research on healthcare technologies that will allow better diagnosis, faster healthcare procedures, and better outcomes for the overall healthcare sector. However, technology can only be viewed as beneficial if it reduces healthcare costs and/or improves healthcare outcomes (Sammartin 1139). The unpredictability of technology in terms of when it will be discovered or used in the healthcare sector makes it an unreliable strategy in the short-term. Regardless of such shortcomings, it is still important to dedicate resources to the development or acquisition of better technology into the healthcare sector.
Focus on Quality of Healthcare
It is important to note that future health conditions are linked to the lifestyle and healthcare that an individual receives while young. Te future is determined by key factors such as adequate income, education, housing, transportation, and social support, among other factors. Consequently, it is very important to integrate and promote the incorporation of healthy aging needs into a population’s public health approach to the aging societies such as Canada. There is a need to ensure adequate research to understand the factors that lead to many health conditions faced by the elderly in the society such as cancer, diabetes, dementia, and cardiovascular diseases among other ailments that are common in the old age.
Initiatives that focus on chronic diseases can translate into cost saving that can help to reduce the burden of healthcare costs to the economy. For instance, delaying the onset of diseases such as Alzheimer’s condition, which is one of the most costly chronic diseases, can translate into billions of dollars in savings annually (Flood and Haugan 324). Programs that focus on health promotion such as primary prevention of falls in old age lead to better health outcomes and reduced healthcare costs at the household and national levels.
Home Care and Institutionalized Care
Hospitalization is one of the major areas that elderly population incurs high health care costs. The ability to reduce hospitalization or postpone institutionalization is an important approach that reduces costs, enhances the quality of life, and/or provides greater choices for the elderly (Sammartin 1137). It is also evident that most elderly people would prefer to be cared for from the comfort of their homes. As such, there is the need to dedicate efforts that will not only reduce hospitalization but also promote strategies that will ensure that the elderly people can receive care at the comfort of their homes. There is the need to dedicate more resources to the homecare and community support. Despite the potential that home-based care has on reducing the overall cost of healthcare among the aged, many territories in the country only spend between 4% and 5% of the healthcare budgets on homecare. The respite services can include adult-day programs, housekeeping, temporary breaks, personal emergency system, counseling, and peer support among others.
Conclusion
It is evident that more people are living longer because of the improved health and related technologies and services. With more than 12 million elderly people expected in the country by 2041, representing more than 25% of the population, The Canadian health care system must be ready to address the increasing healthcare cost. Such a large elderly population will exert pressure on the country’s budget and economy. The increased chronic diseases and the reduced working class will place an overwhelming pressure on the working people. Further, a higher elderly population will also mean that more workers will also be older and less productive, hence making the situation even more difficult. However, through proper planning and budgeting, it is likely that the healthcare financing in the country will remain sustainable. Firstly, the steady economic growth that the country is experiencing will be enough to cover the extra cost that the elderly population poses. Other important measures that may help include higher adoption of technology, revising recruitment and retention strategies, and reviewing the funding approaches in the country to include other approaches to funding such as prefunding of healthcare through current taxation and insurance. In conclusion, with the changes proposed above, the healthcare sector funding will remain sustainable even with the increase in the population of elderly people in the country.
Works Cited
Flood, Colleen, and Amanda Haugan. “Is Canada odd? A comparison of European and Canadian approaches to choice and regulation of the public/private divide in health care.” Health Economics, Policy and Law 5.03(2010): 319-341. Print.
Hsiao, William. “Why is a systemic view of health financing necessary?” Health Affairs 26.4(2007): 950-961. Print.
Kutzin, Joseph, Cheryl Cashin, and Melitta Jakab. “Implementing health financing reform.” World Health Organisation on behalf of the European Observatory on Health Systems and Policies 7.5(2010): 16-31. Print.
Morgan, Steve, Jamie Daw, and Michael Law. “Rethinking pharmacare in Canada.” CD Howe Institute Commentary 384.3(2013): 41-53. Print.
Sammartin, Claudia. “Comparing health and health care use in Canada and the United States.” Health Affairs 25.4(2006): 1133-1142. Print.
Sibley, Lyn, and Jonathan Weiner. “An evaluation of access to health care services along the rural-urban continuum in Canada.” BMC health services research 11.1(2014): 20-36. Print.
Steinbrook, Robert. “Private health care in Canada.” New England Journal of Medicine 354.16(2006): 1661-1664. Print.