Pregnancy and Its Effects on Heart Health
All women planning pregnancy should be aware of changes to the heart associated with gestation. It is not a secret that being pregnant puts extra stress on the various systems of your body, which involves drastic increases in the volume of blood to support the nutritional needs of the developing fetus.
Pregnancy and Its Effects on Heart Health (Cont-d)
Due to changes in blood volume, the heart has to pump more blood per minute, which results in the increased cardiac output and heart rate. These and other changes can be particularly dangerous when it comes to women with specific pre-existing diagnoses, such as congenital heart defects, chronic hypertension, and diabetes. As you can see from the infographic, pregnancy is compared to the nature’s stress test on women’s cardiovascular system.

Heart Disease and Preparing for Pregnancy
Women with pre-existing heart diseases who wish to conceive should make decisions with reference to professional advice and make sure that they have timely access to relevant services. Before starting the attempts to get pregnant, it is highly recommended to visit your cardiologist and an obstetrician who is trained in high-risk pregnancy care to get additional information regarding contraindications to pregnancy in your specific case. Similarly, these specialists can support you in adjusting your current lifestyle to reduce the risks of complications to a minimum and make changes to your current medication plan since not all heart drugs are absolutely safe in pregnancy.
Prenatal Assessments and Cardiovascular Health
After becoming pregnant, it is of utmost importance to get regular health and pregnancy development assessments if you have increased risks of heart conditions or even a confirmed diagnosis. Aside from weight and blood pressure measurements and blood and urine tests, high-risk patients may need to undergo specific non-invasive heart function assessments. Electrocardiography is applied to learn more about the electrical activity of the heart. Next, your provider might implement echocardiography or an ultrasound of your heart to exclude the presence of blood clots and evaluate the valves’ functioning. Health providers will carefully evaluate your ECG and echocardiography results since changes on these tests are common in both normal and problematic pregnancies (Elkayam, 2019). Finally, there are safe submaximal stress tests that involve moderate exercise and the assessment of the body’s cardiovascular response to stress (Elkayam, 2019). Such tests are sometimes used in pregnant women to get a full picture of their heart health.
Symptoms and Concerns to Be Reported
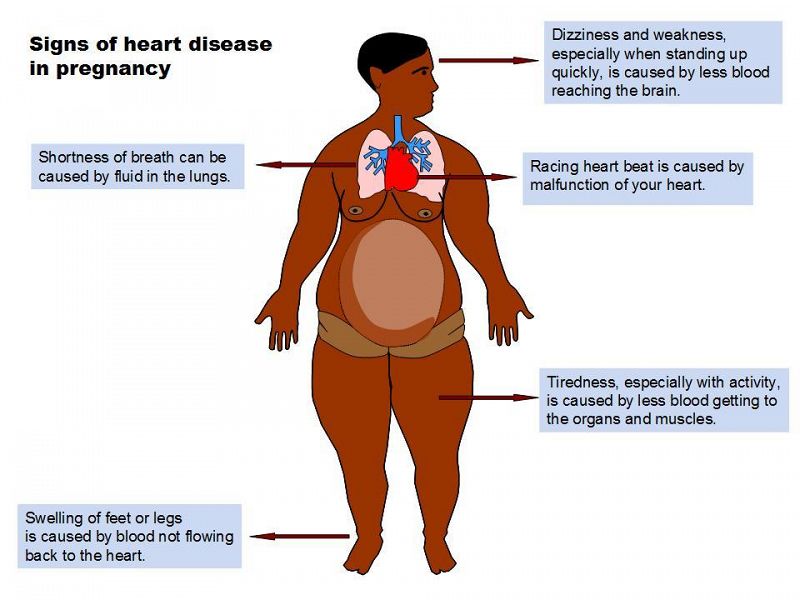
There is a series of warning symptoms that pregnant patients at risk of heart disease should be able to recognize and report to their healthcare providers as soon as possible. Paying attention to your general well-being is critical, and warning signs to be reported may include unreasonable fatigue, cough with blood, and chest pain.
Symptoms and Concerns to Be Reported (Cont-d)
HEDU Africa (n.d.) has prepared an infographic to discuss the warning signs in pregnant patients (see the slide).
Complication Prevention Recommendations
Pregnant women are often curious about the preventive measures they can implement to minimize the risks of cardiovascular disease and other complications. As a rule, all patients are recommended to utilize pregnancy healthcare services on a regular basis to let providers stay aware of the key health risks and propose treatments and lifestyle changes. Aside from regular appointments, it is essential to follow all medication recommendations. After becoming pregnant, women with chronic conditions often need their medication plans to be corrected to minimize harmful influences on the fetus, and following updated recommendations is critical, whereas self-medication involves substantial health-related risks.
Complication Prevention Recommendations and Lifestyle Changes
Communicating and collaborating with care providers to stay updated on your health is important for reducing anxiety, stemming from the sense of uncertainty. However, following general lifestyle improvement recommendations can also be helpful in promoting heart health in women with and without pre-existing heart problems. It includes avoiding exhaustive physical activity, getting enough rest on a daily basis, such as daytime naps (if possible), and making efforts to normalize your BMI and preventing excessive weight gains. Protecting cardiovascular health in pregnancy also requires breaking bad habits, which is often challenging to do without professional assistance.
Learning Objectives and NCLEX-Style Questions
The teaching presentation is aimed at increasing the awareness of heart problems in pregnant women and those planning pregnancy. After its implementation, patients are expected to meet three measurable learning objectives related to knowledge. They include the ability to demonstrate a basic understanding of essential pregnancy-related changes affecting the heart, worrying symptoms that require medical attention, and key recommendations for pregnant patients. Three NCLEX-style questions have been developed to facilitate the measurement of learning outcomes and knowledge gains, and the first question refers to the common health effects of becoming pregnant.
Q1. Which of the following is not among the normal effects of pregnancy on the heart?
- Increased blood volume
- Increased heart rate
- Low resting heart rate
- Increased cardiac output
The next multiple-choice question encourages the respondents to recollect information on the common symptoms of cardiovascular issues in pregnant women and find one incorrect answer. Finally, the last question is related to the third learning objective and encourages the audience to find one potentially problematic behavior in pregnancy.
Q2. Which of the following is not a common symptom of cardiovascular issues in pregnancy?
- Syncope
- Leg swelling and tiredness
- Chest pain
- Headache
Q3. Which of the following does not promote a healthy pregnancy?
- Eating a balanced diet
- Self-medication
- Regular weight gain tracking
- Breaking bad habits
References
Elkayam, U. (2019). Cardiovascular evaluation during pregnancy. In U. Elkayam (Ed.), Cardiac problems in pregnancy (4th ed., pp. 17-31). Wiley Publishing.
HEDU Africa. (n.d.). Shortness of breath during pregnancy can harm your unborn baby. Web.
CardioSmart. (2018). Pregnancy complications and heart disease risk. Web.
Iftikhar, S. F., & Biswas, M. (2020). Cardiac disease in pregnancy. StatPearls. Web.
Mayo Clinic. (2020). Heart conditions and pregnancy: Know the risks. Web.