Summary of a Healthcare Problem
Nowadays, the problems of postnatal care and the necessity to offer as many improvements and interventions as possible are frequently discussed by researchers around the whole world. Women, who have currently given birth to their children, should be ready for several changes in their lives and the necessity to complete several new duties and tasks. As a rule, in such situations, many women lose control over their lives and have to focus on their children.
Still, it is also important to remember that their personal needs, family obligations, and social relations cannot be neglected. Therefore, certain attention should be paid to postnatal care and its dependence on the incomes of families. The problems in postnatal care could be explained by poorly trained nurses and midwives, and the inabilities to clarify what kind of help should be offered to the families with newborns (Gauba, Chhugani, & Arora, 2015; Mirmolaei, Valizadeh, Mahmoodi, & Tavakol, 2014).
The current practice includes the improvements in the work of mid-level medical workers and education. Postnatal care could be offered by mid-level health workers and by high-level health workers (Lassi, Cometto, Huicho, & Bhutta, 2013). Its quality depends on not only the level of knowledge of medical workers and their abilities to help but also on the abilities of parents to analyze situations, use their knowledge, and be ready to help a child in a short period.
Besides, women have to understand how crucial participative learning could be because they could observe what steps to take when they start caring for babies, check their readiness for being mothers, and use their settings to achieve good results in postnatal care (Prost et al., 2013). Parent education is one of the main concepts in postnatal care because it involves both, mothers and fathers, and helps to create appropriate conditions for taking care of children (Khresheh, Suhaimat, Jalamdeh, & Barclay, 2011).
Postnatal care could have several forms, and mothers have to be aware of them and know when and how to ask for it. Sometimes, nurses (midwives) visit families with newborns at home. Sometimes, parents visit hospitals independently. Each method has its positive and negative sides as well as positive and negative outcomes for children and their families. The level of income defines the quality of postnatal care that could be offered to people. Unfortunately, this truth cannot be neglected. Therefore, various situations when postnatal care is offered should be investigated to prove that such interventions as home visiting, telephone hotlines, and parent education could improve family satisfaction, prevent maltreatment, and change the quality of life.
PICO Question
In low-income families who need postnatal care (P), do home visiting programs, telephone hotline services, and parent education (I) compared to usual treatment (C) influence family satisfaction, maltreatment prevention, and the quality of life (O)?
Search Strategy
The topic of postnatal care is frequently discussed by many researchers and writers. On the one hand, it is not that difficult to put such keywords as “postnatal care”, “low income”, “home visit”, “parent education”, and “postnatal care interventions” for the search and find several different sources. Many educational and advertising sources could be found, and general facts and information about how it means to be a mother for the first time or how to deal with parental stress are offered. On the other hand, the current research strategy requires the presence of sources with research evidence and non-research evidence. Therefore, it is important to add the required type of study to a search engine. It is better to address credible sites and consider peer-reviewed articles.
Such search engines as Scholar. Google and Medscape were chosen. Regarding the requirements of the project, about 1000 articles were found. At the same time, it was necessary to identify the time frames and choose the articles that were written after 2011. The results help to clarify that several qualitative and quantitative research methods were used by the researchers from different parts of the world to cover the topic of postnatal care, develop various interventions, and identify the challenges that medical workers, parents, and even children could have in case postnatal care is poorly organized.
People tried to discover different aspects of the topic and prove that mothers, as well as medical workers, should pay much attention to the development of the level of knowledge that was required to take care of a newborn. Research articles by Gauba et al. (2015) about the importance of training programs for nurses who offer postnatal care and Lassi et al. (2013) about the quality of services offered by mid-level and high-level medical workers helped to understand what kind of work had been already done in the chosen sphere and what contributions were expected. Such types of articles aim at discovering reviews and randomized controlled trials where people face a particular problem and find an effective solution.
These research evidence sources are numerous because people want to improve postnatal care from different aspects and make sure that the level of income does not influence the quality of care offered to mothers. Non-research articles provide the reader with the analysis of the already offered interventions, activities, and decisions. Such non-research articles like Ong et al. (2014) about the interventions that help to deal with postpartum stress among first-time mothers and Dayton, Walsh, Oh, and Volling (2015) about the types of soothing behaviors inherent to fathers and mothers of infants are used to explain what kind of help could be offered during postnatal care and what steps young people should take to succeed as parents.
The presence of research and non-research evidence sources proves that the topic of postnatal care has to be discussed and developed nowadays. There are many technological innovations and possibilities for people, and the chosen research strategy shows that researchers want to continue investigating this issue and introduce as many solutions, recommendations, and interventions as possible to make sure that medical workers including nurses, midwives, therapists, and other doctors, as well as mothers, fathers, and other members of families with newborns could understand their roles and take the steps that improve the quality of life, prevent maltreatment, and promote family satisfaction.
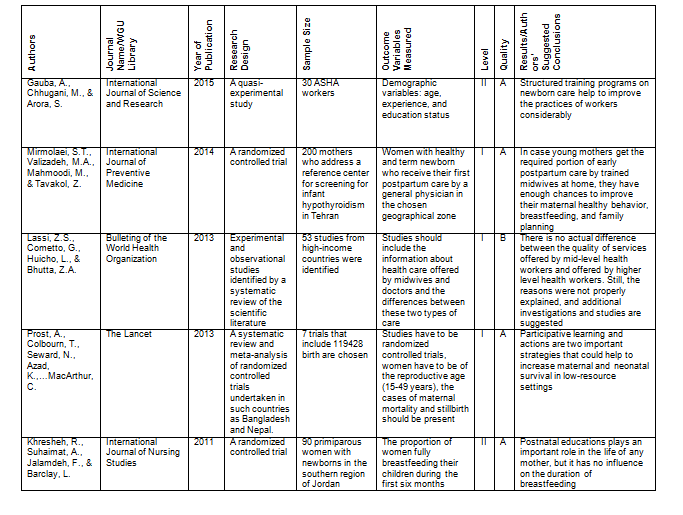
Evidence Matrix: Research Evidence Sources
Recommended Practice Change
Postnatal care is the type of care that should be offered to mothers and babies by experienced midwives during the first six months after birth. Regarding the current developments, technological achievements, and considerably changed patients’ expectations, some aspects of postnatal care should be improved, and new recommendations should be given. The current goals of postnatal care include family satisfaction, maltreatment prevention, and improved quality of life.
All these objectives could be achieved in case midwives accept the recommended practice change and understand the importance of such interventions as the development of home visiting programs, telephone hotline services, and parent education. Cooperation between midwives and parents is the main practice change that should be developed in the current project. Nurses, who have to work with mothers and their babies, have to comprehend how crucial their role to families could be. First, many mothers do not know what to expect as soon as they stay with their babies alone, and the outcomes of maternal healthy behavior remain to be unclear (Mirmolaei et al., 2014).
Besides, many parents experience stressful situations and the inabilities to live their normal lives with babies. Therefore, they think that it is normal to address midwives or even higher-level health workers and ask for professional help (Lassi et al., 2013). Still, the investigations prove that the level of medical workers does not influence the quality and variety of help. Much attention should be paid to the development of special training programs that aim at newborn care (Gauba et al., 2015), explanations of the ideas of participative learning among parents (Prost et al., 2013), and support of postnatal parent education that could be used to improve the quality of a baby’s life (Khresheh et. al., 2011). All these improvements and changes are possible through home visits, telephone calls, and direct lessons.
The essence of such recommendation practice change is to focus on the information that is offered to parents (mothers in particular) by midwives, nurses, and doctors. It is not enough to make sure that some lessons are given, and some brief facts about baby care are explained. Doctors have to make sure that mothers and babies have normal health indicators, nurses should check the psychological and physical condition of patients, and midwives have to clarify if mothers have enough skills and knowledge to continue taking care of their children with time.
Such conclusions cannot be made in two or even five days after birth. Therefore, home visits by midwives turn out to be one of the best practices that could be used to assist mothers, deprive them of extra doubts or concerns, and provide babies with the best care.
Telephone hotlines are also crucial for the development of communication between mothers and midwives about postnatal care. Finally, the changes in parent education are important because mothers have to know how to provide their babies with routine care, how to feed them, and how to use and change diapers. There are several mothers, who feel discomfort and uncertainty when they have to stay with their children alone. Therefore, the additional help of midwives through home visits and telephone calls could improve the level of parent education and the quality of all family members’ lives.
Recommendation Implementation
To promote the recommended change practice, it is necessary to understand what stakeholders should be involved in the project, to identify what barriers could occur, to develop the strategies with the help of which barriers could be overcome, and effective solutions could be offered, and to describe the indicators with the help of which it is possible to measure the outcomes of recommendations.
There are three possible groups of people, who could be involved in the decision to implement the offered recommendation in postnatal care. First, mothers have to participate in this change. They should share their opinions and experiences to create an appropriate basis for a change. Their opinions, challenges, and expectations should be identified to explain what improvements of postnatal care should be made. Another group of stakeholders to be mentioned includes nurses and midwives who have to share their knowledge about how to take care of newborns. Finally, it is possible to include social workers in this kind of change so that they could observe the results of cooperation between mothers and midwives and consider the effects of improvements offered on children and the general well-being of a family.
However, some barriers may occur in case such change is offered in the nursing practice setting. First, mothers could have different levels of knowledge about the postnatal care they have to provide their children with. Second, not all nurses are ready to cooperate with mothers when they leave hospitals. Finally, the stakeholders identified for this change may face a challenge to start cooperating. There is a need for a guide for all those stakeholders and a system to follow.
Such strategies as online questionnaires and the introduction of a coordinator could help to solve the problems and implement the change successfully. Online questionnaires should help mothers share their experiences and not be confused with the necessity to discover personal shortages in public. As soon as mothers visit hospitals to ask for prenatal care, they have to fill in special questions about the knowledge they have about child care and their readiness to take care of their children independently. As soon as the material is given by the mothers, it is necessary to find a person who could analyze the answers and think about the needs of every mother.
The idea to have a special postnatal care coordinator seems to be a good way out. In the nursing practice setting, there should be one person who investigates the conditions of mothers, their readiness to take care of newborns, and their need for additional help in the form of midwives during home visits. Such a coordinator could provide a midwife with the required portion of information about a mother and underline what kind of help should be offered.
During a home visit or a telephone call, a midwife or another medical worker has the required portion of knowledge and material that can be used. In general, two main strategies that are the development of online questionnaires and the promotion of a postnatal care coordinator could be offered in the project that should help mothers enjoy postnatal care regardless of their level of knowledge or the level of income.
To succeed in the development of this project, one indicator has to be clarified. It helps to measure the outcome related to the offered recommendation. In this case, the indicator is the level of family satisfaction that could be “High”, “Middle”, and “Low”. After the six months of postnatal care are over, parents should share their opinions about their satisfaction with their new status (being a parent) and the cooperation with midwives.
Low-income families could think that their inabilities to pay for extra help could influence the quality of life, family satisfaction, and even the ability to prevent maltreatment. Still, this project does not require much time to identify the needs of mothers and many people to organize the necessary portion of work. Home visiting, telephone hotline services, and the abilities to improve parent education are the main outcomes of the healthcare problem under consideration.
Several low-income families believe that their financial challenges lead to problematic and poor postnatal care. However, such concerns could be solved, and the conditions under which postnatal care is offered could be improved. Parents have to understand that their information and the abilities, to tell the truth and define personal uncertainties serve as the basis for the work of midwives. If medical workers are misinformed, the quality of help and support could be poor as well as the level of family satisfaction could below.
References
Dayton, C.J., Walsh, T.B., Oh, W., & Volling, B. (2015). Hush now baby: Mothers’ and fathers’ strategies for soothing their infants and associated parenting outcomes. Journal of Pediatric Health Care, 29(2), 145-155.
Gauba, A., Chhugani, M., & Arora, S. (2015). A quasi experimental study to assess the effectiveness of structures training program on practices of Asha workers related to new born care based on Asha module – 6 skills that saves lives in a selected communities of Delhi. International Journal of Science and Research, 4(11), 2341-2345.
Khresheh, R., Suhaimat, A., Jalamdeh, F., & Barclay, L. (2011). The effect of a postnatal education and support program on breastfeeding among primiparous women: A randomized controlled trial. International Journal of Nursing Studies, 48(9), 1058-1065.
Lassi, Z. S., Cometto, G., Huicho, L., & Bhutta, Z. A. (2013). Quality of care provided by mid-level health workers: Systematic review and meta-analysis. Bulletin of the World Health Organization, 91(11), 824-833.
Mirmolaei, S. T., Valizadeh, M. A., Mahmoodi, M., & Tavakol, Z. (2014). Comparison of effects of home visits and routine postpartum care on the healthy behaviors of Iranian low-risk mothers. International Journal of Preventive Medicine, 5(1), 61-68.
Ong, S.F., Chan, W.C.S., Shorey, S., Chong, Y.S., Klainin-Yobas, P., & He, H.G. (2014). Postnatal experiences and support needs of first-time mothers in Singapore: A descriptive qualitative study. Midwifery, 30(6), 772-778.
Prost, A., Colbourn, T., Seward, N., Azad, K., Coomarasamy, A., Copas, A.,… & MacArthur, C. (2013). Women’s groups practicing participatory learning and action to improve maternal and newborn health in low-resource settings: A systematic review and meta-analysis. The Lancet, 381(9879), 1736-1746.